History, Origin, Spread, and Virology of SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first emerged in China’s Hubei Province at the end of 2019. It quickly spread throughout the province’s largest city, Wuhan, before escaping into other parts of China, Southeast Asia, and then the rest of the world. The virus is responsible for coronavirus disease of 2019 (COVID-19), which is now recognized to not only cause acute respiratory disease but also have a system-wide effect throughout the body. This chapter examines the historical context in which the outbreak took place by looking at previous pandemics and outbreaks involving other coronaviruses; follows the timeline between the first emergence of the virus until March 2020, when COVID-19 was declared a pandemic by the World Health Organization (WHO); and the basic virology of SARS-CoV-2.
The Dawn of the COVID Era
As 2019 came to an end, hospitals in Wuhan, a city in China’s Hubei Province, reported that they were seeing an alarming rise in cases of atypical pneumonia. Several days later, the genome of SARS-CoV-2 was sequenced, and the WHO announced that the novel coronavirus was the pathogen behind the wave of illness.1 On January 9, 2020, the first fatality due to coronavirus disease 2019 (COVID-19) was recorded.2 In the weeks that followed, the virus spread throughout the world, infecting thousands.
It was finally declared a pandemic by the WHO on March 11, 2020. In the months that followed, the virus brought world commerce grinding to a halt as the number of infections rose exponentially due to multiple concurrent surges.
It was finally declared a pandemic by the WHO on March 11, 2020. In the months that followed, the virus brought world commerce grinding to a halt as the number of infections rose exponentially due to multiple concurrent surges.
By the dawn of 2021, the pandemic had gone through at least three distinct waves of infections across the globe, and as of the summer of 2021, the pandemic was still not under control and many now believe that COVID-19 may become endemic, particularly in areas where vaccination efforts have lagged. However, various preventative measures had likely saved at least hundreds of thousands of lives and many national health care systems from collapse, while the herculean effort to create and test both the efficacy and the safety of multiple vaccines in record time had yielded several viable results that were approved for emergency use by governments around the world. Since that time, challenges have persisted in manufacturing and distributing the vaccines on an international basis, numerous variants of concern have emerged, and surges in the Americas, Europe, and Southeast Asia have caused innumerable deaths, but the worst of the initial phases of the pandemic appear to be behind us as we enter the autumn of 2021. It should be noted that this is cautious optimism based on emerging evidence rather than a prediction, and that we are by no means out of the woods yet, especially in regions where there is limited access to vaccines or where medical resources are scarce.
In the coming years, we will likely struggle to fully grasp the horrific impact of the pandemic between 2020 and 2021, even if SARS-CoV-2 continues to persist as an endemic illness. Beyond the immediate emotional and financial turmoil that the pandemic left in its wake, millions of people will grapple with long-term psychological problems due to an array of stressors that were directly and indirectly related to the pandemic, and these will likely be compounded by political and economic repercussions that will continue to evolve for months or years to come. For an unfathomably large number of individuals across the globe, recovery will require rethinking how they approach their mental health and coming to terms with the fact that a return to normalcy, as defined by routines from the prepandemic period, may not be possible. This includes not only those who have since been diagnosed with posttraumatic stress disorder (PTSD) due to the experience of being stricken ill by the virus or those who have struggled with cognitive issues (eg, “brain fog,” memory lapses, migraine) following a less severe or asymptomatic case of COVID-19. It also concerns those who remained in isolation for months and emerged to find themselves incapable of simply resuming “normal” activities as if nothing had changed.
Before delving into these issues, however, we must first understand the scope of the pandemic and the science of the SARS-CoV-2 virus. In this
chapter, as well as the three subsequent chapters, I will explore multiple aspects of the virus, including historic precedent, the timeline of the pandemic, and the virology and epidemiology of SARS-CoV-2. This is by no means an exhaustive review of all the material on the coronavirus or COVID-19, and it is certainly not to be taken as the final word but merely a summation of the best information that is available at the time of this writing.i
chapter, as well as the three subsequent chapters, I will explore multiple aspects of the virus, including historic precedent, the timeline of the pandemic, and the virology and epidemiology of SARS-CoV-2. This is by no means an exhaustive review of all the material on the coronavirus or COVID-19, and it is certainly not to be taken as the final word but merely a summation of the best information that is available at the time of this writing.i
Pandemics
When an infectious disease suddenly and rapidly spreads throughout a community, it is known as an epidemic (a combination of the Greek words epi and demos, meaning “among” and “people,” respectively). When an infectious disease rapidly spreads between and affects multiple communities across countries or continents, it is known as a pandemic (pan-coming from the Greek for “all”). When an infectious disease has become common within a population, it is known as being endemic (en is Greek for “in”). It means it is literally part of the community. As Devi Sridhar, chair of global public health at the University of Edinburgh, told the Washington Post in an article published in June 2021, “Throughout history, pandemics have ended when the disease ceases to dominate daily life and retreats into the background like other health challenges.”3 As of early 2021, a majority of epidemiologists interviewed by Nature said this is the most likely outcome for the SARS-CoV-2 virus.4
Those of us who have lived through the events of 2020 and early 2021 will likely shudder at the very mention of the word “pandemic” for years to come. The word will be associated with quarantine, social distancing measures, rolling death counts on the nightly news, and specific personal tragedies and traumas. However, most pandemics, while no doubt deadly, do not elicit the kind of global response that has been necessary to reduce the spread of SARS-CoV-2. When one uses the classical definition of a pandemic, “an epidemic occurring worldwide, over a very wide area crossing international boundaries and usually affecting a large
number of people,”5 these events turn out to be surprisingly common given our globalized world. This will likely continue to be the case so long as communities remain economically and culturally interconnected, and so long as worldwide travel remains quick, easy, and affordable. As Mark Harrison concluded in Contagion, his seminal work on the subject, “Commerce has been a major factor in the redistribution of diseases, allowing pathogens and their vectors to circulate more widely than before, often with catastrophic results.”6
number of people,”5 these events turn out to be surprisingly common given our globalized world. This will likely continue to be the case so long as communities remain economically and culturally interconnected, and so long as worldwide travel remains quick, easy, and affordable. As Mark Harrison concluded in Contagion, his seminal work on the subject, “Commerce has been a major factor in the redistribution of diseases, allowing pathogens and their vectors to circulate more widely than before, often with catastrophic results.”6
Given the above definition and the fact that increasing commercial activity has allowed for pathogens to spread across the globe more easily, it should not be surprising that most people had already lived through at least one pandemic by the time SARS-CoV-2 emerged in Wuhan. Just over a decade before, in 2009, the “swine flu,” which was caused by the influenza A (H5N1) pdm09 virus, jumped from a pig to a human in a Mexican village and proceeded to rapidly spread around the world.7 By June of that year, the WHO declared that it was a pandemic. By the end of 2010, the virus had infected tens of millions of people and led to the deaths of an estimated 284,500 individuals.8
While this is no doubt an enormous tragedy, most of us have but a hazy recollection of a very bad flu season between fall 2009 and spring 2010. A similar thing can be said for those who remember the influenza pandemics of 1957 or 1968.9 Worldwide, the two pandemics caused between 500,000 and 2 million and between 1 million and 2 million deaths, respectively, but they did not lead to widespread closures of public institutions or even modest changes to the lives of most people.10 The only somewhat recent influenza pandemic to rival the response of the COVID-19 pandemic occurred between 1918 and 1919. In those two years, three distinct waves of infection spread around the world and caused the deaths of between 45 and 100 million people.11, 12 The Great War, which ranged from 1914 to 1919, is estimated to have only killed around 20 million people.
Beyond the extremely high number of deaths, the 1918-1919 flu (known as “the Spanish flu”) and the COVID-19 pandemic share a number of unfortunate similarities according to historical records and the testimonies of the handful of people who lived to see both.13 Like the COVID-19 pandemic, the influenza pandemic’s rapacity was only matched by its scope. It was a truly global phenomenon because the introduction of modern means of travel had made it possible to reach even the most remote locations on Earth. Public health measures were also taken during the influenza pandemic to stop the spread, including closing schools, churches, theaters, and other public spaces. It was also found that cities that took proactive steps to stop the spread of disease and mandated social distancing measures typically fared better than those that did not, and
that reopening too early often proved to be disastrous. For example, New York City, which reacted quicker than other cities in the United States by requiring quarantines and staggering business hours, experienced one of the lowest death rates in the Northeast.12 Philadelphia, unfortunately, waited to implement similar measures. To make matters worse, the city infamously held a parade to support the war effort even though cases of the virus had been reported in the area. An estimated 200,000 people attended the parade, and the effects were both swift and nothing short of cataclysmic.14 Every bed in all 31 area hospitals was filled within 72 hours. The city ultimately saw the sharpest spike and highest peak death rate of any American city.12
that reopening too early often proved to be disastrous. For example, New York City, which reacted quicker than other cities in the United States by requiring quarantines and staggering business hours, experienced one of the lowest death rates in the Northeast.12 Philadelphia, unfortunately, waited to implement similar measures. To make matters worse, the city infamously held a parade to support the war effort even though cases of the virus had been reported in the area. An estimated 200,000 people attended the parade, and the effects were both swift and nothing short of cataclysmic.14 Every bed in all 31 area hospitals was filled within 72 hours. The city ultimately saw the sharpest spike and highest peak death rate of any American city.12
As was the case in 2020, masks also became a common part of everyday life and mandatory face mask laws went into effect in a myriad of cities (see Figure 1.1). They also became a symbol of division. While it does not seem as though resistance was nearly as partisan or widespread as it was in 2020 or 2021, there were some organized efforts to fight mandatory face coverings as being either ineffective or unconstitutional. The most notable example of the latter was the Anti-Mask League in San Francisco.15 An example of the former can be found in a statement issued by the U.S. Navy in 1919, which read: “Masks of improper design, made of wide-mesh gauze, which rest against the mouth and nose, become wet with saliva, soiled with fingers, and are changed infrequently, may lead to infection rather than prevent it, especially when worn by persons who have not even a rudimentary knowledge of the mode of transmission of the causative agents of communicative diseases.”16 This condescending remark occurred more than a decade before influenza A was isolated and identified as a virus.17
In addition to the discord between those who demanded the public take part in efforts to stem the spread of the disease and those who
believed that such demands were examples of governmental overreach, there was yet another similarity between the viruses that led to the pandemic of 1918 and the COVID-19 pandemic. Part of what made the 1918 flu so deadly was the novelty of the influenza strain (H5N1), particularly among communities of individuals who had experienced limited or no exposure to most “Old World” diseases (measles, smallpox, cholera, influenza, etc). Indigenous peoples in the United States, New Zealand, and Australia were found to have fatality rates of four times that of surrounding populations, which were predominately comprised of individuals of European descent.18 Among the Māori of New Zealand, the death rate was calculated to be 4230 per 100,000—7.3 times higher than the European rate.19 Virtually every Pacific island affected by the virus saw at least 5% of their population perish. In Western Samoa, 22% (approximately 38,000 individuals) of the population died in a matter of weeks.18 The novelty of SARS-CoV-2 has also been one of the reasons why it is so deadly; there does not appear to be any group of people who possess a comparable form of immunity.
believed that such demands were examples of governmental overreach, there was yet another similarity between the viruses that led to the pandemic of 1918 and the COVID-19 pandemic. Part of what made the 1918 flu so deadly was the novelty of the influenza strain (H5N1), particularly among communities of individuals who had experienced limited or no exposure to most “Old World” diseases (measles, smallpox, cholera, influenza, etc). Indigenous peoples in the United States, New Zealand, and Australia were found to have fatality rates of four times that of surrounding populations, which were predominately comprised of individuals of European descent.18 Among the Māori of New Zealand, the death rate was calculated to be 4230 per 100,000—7.3 times higher than the European rate.19 Virtually every Pacific island affected by the virus saw at least 5% of their population perish. In Western Samoa, 22% (approximately 38,000 individuals) of the population died in a matter of weeks.18 The novelty of SARS-CoV-2 has also been one of the reasons why it is so deadly; there does not appear to be any group of people who possess a comparable form of immunity.
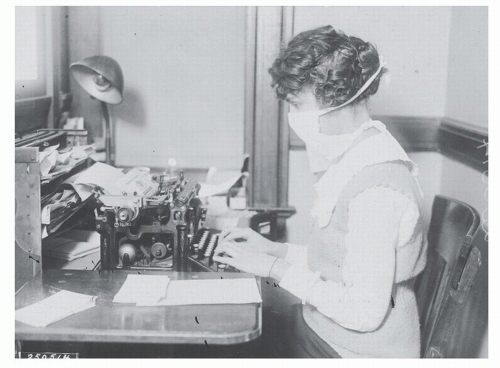 Figure 1.1 Woman in mask while working in an office circa. 1919. (Image used with the permission of the National Archives [local identifier: 165-WW-269B-16].) |
Beyond the dangers of novel viruses, there are three takeaways to be gathered from the comparisons between the H1N1 flu of 1918 and the SARS-CoV-2 virus that first emerged in 2019.
First, the COVID-19 pandemic was not unprecedented. Precedents for pandemics have been set multiple times, perhaps no more explicitly than 100 years before the SARS-CoV-2 virus emerged in Wuhan. The only thing that was unprecedented was how much we chose to ignore the lessons learned from experience. As Wendy Parmet and Mark Rothstein wrote in an introductory segment to the American Journal of Public Health’s centennial on the 1918 influenza pandemic, which was published in November 2018: “Today, three of the leading threats to global public health are attitudinal: hubris, isolationism, and distrust. As to hubris, it is true that we live in the age of genomics, vaccines, antibiotics, mechanical ventilators, and other features of high-technology medicine that were unavailable in 1918. Nevertheless, our technology remains woefully ineffective in preventing influenza.” They continued, “As to the second threat, isolationism, some world leaders erroneously believe that they can seal off their nation’s borders after a public health threat emerges and thus escape the ravages of epidemics in other parts of the world. Public health experts universally reject this naive approach. More than ever, a public health event in any part of the world can create a public health threat everywhere.” Rather presciently, they concluded, “A third problem is distrust. In our era of political polarization, ‘fake news,’ and tribal politics, trust in the media, government officials, and even science is fading. This can be catastrophic if an influenza or another type of pandemic arises. Under such circumstances,
the public’s failure to trust the guidance offered by public health officials may well make a bad situation worse.”20
the public’s failure to trust the guidance offered by public health officials may well make a bad situation worse.”20
The second takeaway is that the classical definition of a pandemic refers to scope rather than mortality rate. Consequently, the number of fatalities associated with even a seemingly minor pandemic (which certainly sounds oxymoronic) becomes astronomical because of the sheer number of individuals who become infected. Even if an outbreak that hits pandemic levels seems relatively mild in hindsight, millions of people may be made severely ill or perish.ii,21 For example, a 1.0% mortality rate may sound like no big deal, but it could amount to 10 million deaths if 1 billion people are infected with the disease.
Third, pandemics are relatively common. This does not mean that they are events that can be ignored or that one does not need to take them seriously. Just the opposite. We should view this information as a reminder that we have enjoyed a relatively tranquil window free of pestilence for a long time, and that this is not the normal state of affairs. There have been several near misses that raised alarm bells when they occurred, but then relatively quickly faded from public memory. Ebola is but one example. Far more worrisome was the H5N1 “bird flu” that emerged in Vietnam in January 2005. Human-to-human transmission did not ever appear to occur, but the virus was extremely transmissible among chickens, ducks, geese, and other fowl raised for human consumption, and hundreds of humans who interacted with infected birds became sick over the course of that year. Had it mutated in a way to make human-to-human transmission possible, there is no telling how deadly it could have been.
Writing just before the SARS-CoV-2 pandemic, the esteemed Czech-Canadian scientist Vaclav Smil observed that, “The typical frequency of influenza pandemics was once every 50 to 60 years between 1700 and 1889
… and only once every 10 to 40 years since 1889. The recurrence interval, calculated simply as the mean time elapsed between the last six known pandemics, is about 28 years, with the extremes of 6 and 53 years.”22 In other words, Smil’s calculations reveal that, at present, influenza pandemics occur roughly every 28 years and may occur as little as six years apart.
… and only once every 10 to 40 years since 1889. The recurrence interval, calculated simply as the mean time elapsed between the last six known pandemics, is about 28 years, with the extremes of 6 and 53 years.”22 In other words, Smil’s calculations reveal that, at present, influenza pandemics occur roughly every 28 years and may occur as little as six years apart.
What is perhaps most concerning is that Smil’s figures are for just one virus: Influenza A. We have discovered more than 200 other species of virus that have demonstrated the ability to infect humans.23 There are an untold number of other novel viruses on this Earth that we have yet to discover, and the number of outbreaks and the number of emerging and novel pathogens has been increasing since 1980.24 These figures will continue to increase as long as human population growth continues, the globalization of goods and travel continues, deforestation continues, and humans continue to practice intensive animal farming where cramped conditions make the spread of disease extremely easy.25
The writing is on the wall. Outbreaks are likely to become more common, and these diseases will have a better chance of reaching pandemic levels if we do not take steps to prepare ourselves. We ignore the lessons that we have learned from the past and the COVID-19 pandemic at our own peril.
Previous Coronavirus Outbreaks
Previous coronavirus outbreaks were far less widespread than the COVID-19 pandemic. This was extremely fortunate, as severe acute respiratory syndrome (SARS) and Middle Eastern respiratory syndrome (MERS) both have terrifyingly high mortality rates—9.56% and approximately 34.5%, respectively.26 As is the case with many coronaviruses, both the SARS and the MERS viruses appear to have come originally from bats. As of late May 2021, the theory on the origin of SARS suggests that a single population of horseshoe bat from China’s Yunnan province appears to be the natural reservoir of the virus. Research has shown that the virus was passed from bats to masked palm civets (Paguma larvata) at an animal market in Guangdong, and then to humans, and subsequently led to human-to-human transmission that then fueled the epidemic.27 Raccoon dogs (Nyctereutes procyonoides) may have also served as intermediaries.28 In the case of MERS, the reservoir bat species appears to be based in Africa, and dromedary camels are believed to be the source of zoonotic infection.29 MERS appears to be endemic among these beasts of burden in Africa but reports of MERS infections have all been tied to the Arabian Peninsula. It is not clear if this is due to extreme
underreporting in Africa, some form of natural immunity, or if it is because MERS strains on the continent are less virulent than those found on the Arabian Peninsula.30
underreporting in Africa, some form of natural immunity, or if it is because MERS strains on the continent are less virulent than those found on the Arabian Peninsula.30
SARS (2002-2004)
The SARS-CoV virus was the first known coronavirus to cause severe illness in humans. The most common clinical features include persistent fever, nonproductive cough, myalgia, chills/rigor, headache, and shortness of breath. Symptoms may also include joint pain, sore throat, rhinorrhea, dizziness, nausea, vomiting, and diarrhea. Diarrhea was reported in 60% of patients and appears to have played a role in virus transmission.31 Renal failure was also reported, with 6.6% of patients developing acute renal failure at a median time of 20 days following symptom onset.31
Though SARS was assumed to be spread via close contact or respiratory droplets when an infected individual coughed or sneezed, strong evidence of a fecal-oral route also emerged.32 This suggests that the virus can be aerosolized and that airborne transmission is possible (see Chapter 2: Transmission of SARS-CoV-2). The high rate of infection among health care workers lends additional credence to the possibility of airborne transmission, since aerosols are generated by procedures like endotracheal intubation and bronchoscopy.33 These were common procedures used to manage patients critically ill with SARS.34
SARS was first observed in China’s Guangdong Province on November 16, 2002. It was initially referred to as a case of atypical pneumonia. Officially, 305 cases were reported in the province between November and February 9, 2003, many of whom were health care workers. Later that month, on February 22, a doctor from Guangdong arrived in Hong Kong, stayed at Metropole Hotel, and spread the virus to 10 other people after either coughing or vomiting in the hallway of his floor. From these 10 individuals, the virus then spread to 29 countries.35 The outbreak peaked in May and ultimately lasted through July 2003, infecting 8098 and causing the deaths of 774 people.36 Following the primary outbreak, a few additional cases of SARS were reported at the end of 2003 and early 2004 and were linked to zoonotic transmission involving civet cats from live animal markets in Guangdong.35
A disproportionate number of health care workers were infected around the world and represented as many as 20% of worldwide cases of SARS.37 This is due to several factors, including workers’ close contact with patients, but infections may have also occurred following procedures that created aerosolized particles laden with viable viruses.
The latter seems possible because secondary illness rates in households were reportedly only 15% in Hong Kong and 6% in Singapore, while total household secondary attack rates were reportedly 7.5%.35, 38 Another peculiarity concerned transmission rates on airplanes, with at least 40 known flights carrying symptomatic cases on board, yet only 29 secondary cases have been linked to these flights. Furthermore, 22 of these cases can be linked to a single flight. Even then, only 22 of 119 (18%) passengers became ill.35
The latter seems possible because secondary illness rates in households were reportedly only 15% in Hong Kong and 6% in Singapore, while total household secondary attack rates were reportedly 7.5%.35, 38 Another peculiarity concerned transmission rates on airplanes, with at least 40 known flights carrying symptomatic cases on board, yet only 29 secondary cases have been linked to these flights. Furthermore, 22 of these cases can be linked to a single flight. Even then, only 22 of 119 (18%) passengers became ill.35
Clearly, SARS was a very contagious virus, but we did not witness the kind of spread that has taken place with SARS-CoV-2. One of the primary reasons for the lack of widespread transmission was due to the symptoms associated with SARS. Individuals infected with SARS were acutely aware of the illness and were able to differentiate symptoms from seasonal allergies or a common cold, and more importantly, asymptomatic cases were exceptionally rare. Also, contrary to SARS-CoV-2, symptom onset was relatively quick—occurring within a few days so individuals knew relatively early whether or not they had been infected. This made contact tracing and quarantining far easier and helped to prevent community spread (when the source of the infection comes from somewhere in the community rather than a specific source or person).
Another important reason behind the successful containment of SARS was due to the relatively early identification of the outbreak. This allowed for some logistical advantages since WHO coordinators, pathologists, and epidemiologists arrived in affected locations before the number of infected patients had swelled, and, consequently, teams could concentrate their efforts and not stretch resources too thin.39 They were able to quarantine those who had been infected and focus on treating those who were sick. As a result of early identification and appropriate distribution of resources, they were able to contain the outbreak and bring it to an end more effectively.
Though the timely global response and collective action that quickly snuffed out the SARS outbreak was praised worldwide, the WHO recognized the need for a more organized response to outbreaks and issued new International Health Regulations that went into force in 2007.6 Despite a positive outcome, many organizations and governments also recognized that the outbreak could have been contained far sooner had the Chinese government been more forthcoming. Consequently, the Chinese government faced a great deal of international criticism not only because of their failure to inform the WHO of the outbreak, but for their decision to wait for more than two months to tell Chinese citizens about the cases of atypical pneumonia in Guangdong.40
MERS (2012-Ongoing)
The first case of MERS appears to have occurred in Zarqa, Jordan, in April 2012.10 It was identified initially only as an acute respiratory illness at a public hospital, and those infected included three civilians and eight health care workers. One of the nurses later died.41 An individual in Saudi Arabia reported similar symptoms in June 2012 and died after being admitted to the hospital. After testing sputum from the patient, it was determined that the cause of death was a novel form of coronavirus—Middle Eastern respiratory syndrome coronavirus (MERS-CoV).10
From 2012 until December 2019, sporadic outbreaks of MERS have occurred around the Arabian Peninsula, with the highest number of cases occurring in Saudi Arabia, and all cases can be traced back to this part of the world. This includes the 2015 outbreak in South Korea, as well as the handful of cases reported in Europe, the United Kingdom, and the United States. As of late May 2021, the WHO reports that there have been 2574 laboratory-confirmed cases in 27 countries with 886 reported deaths.42
Similar to SARS, the clinical presentation of MERS may include flulike symptoms (cough, fever, chills, rhinorrhea, myalgia, fatigue, joint pain, etc) or may include more severe symptoms like shortness of breath and respiratory failure, which may require intubation and ventilation. Gastrointestinal symptoms (nausea, vomiting, diarrhea, abdominal pain, etc) have also been reported.43 Acute renal damage has occurred in more than half of patients, and the majority of cases have required renal replacement therapy.31
Infections originating in a hospital setting (nosocomial) are very common with MERS. The basic reproduction (R0) number for the virus is estimated to be below 1, but it has been calculated to be in the range of 2 to 5 in a hospital setting.44 Like SARS, this suggests that there is a possibility of aerosolization following certain medical procedures (ie, endotracheal intubation, bronchoscopy), which could allow for airborne transmission even if close contact with infected individuals and droplet transmission are believed to be the most common routes of infection.45
The most notable differences between MERS and SARS are that MERS is far deadlier, having a 34.4% mortality rate, and that it appears to jump from dromedary camel to humans relatively easily.42 The incidence of MERS in camel shepherds and slaughterhouse workers is 15 and 23 times higher, respectively, compared to the general population.43
H5N1 (2005)
The 2005 H1N1 “bird flu” outbreak occurred following the outbreak of SARS and prior to the first case of MERS. Though the threat of
human-to-human transmission did not materialize, the high probability that a similar flu variant might do so in the future led the United States to ramp up their biodefense and biosurveillance capabilities and to devise strategies to quickly respond to pandemic scenarios.
human-to-human transmission did not materialize, the high probability that a similar flu variant might do so in the future led the United States to ramp up their biodefense and biosurveillance capabilities and to devise strategies to quickly respond to pandemic scenarios.
One positive outcome of this interest in biodefense was a program called Global Argus, which monitored open-source information to detect and track early indications of foreign biological events that may represent threats to global health and national security. The general idea was that indirect and public information could be far more valuable to epidemiologists than waiting for confirmation of an outbreak from a government that may lack the resources for effective biomonitoring or may actively seek to suppress information that would clearly indicate that an epidemic or pandemic was brewing. An individual who worked on the program explained to The Atlantic’s James Fallows that the indicators could be something that would seem insignificant to the untrained eye. Take, for example, a sudden fall in the price of chicken in a village in Thailand. Fluctuations in price are extremely common and a momentary crash in price may be due to a variety of reasons that have nothing to do with disease. Conversely, a sudden drop in price may mean that a novel form of avian flu has entered into circulation in the region and that several farmers have slaughtered their entire flock at once and sent them to market on the same day.46 It may not be a telltale sign of an outbreak on its own, but if enough of pieces like this come together in a region where new strains of avian flus frequently materialize, it could spell trouble.
Ultimately, the project was capable of processing quarter million pieces of news per day. In the waning days of the Obama administration, the Pandemic Prediction and Forecasting Science Technology Working Group released a report showcasing the advances in prediction technology since the early days of Global Argus and described an even more sophisticated biosurveillance system that had been supercharged by faster processing speeds and advances in artificial intelligences systems.47 It did not go into details, but given that Global Argus predated the release of the first iPhone, there is good reason to believe that the capabilities of the new monitoring systems are exponentially more advanced.
These open-source monitoring programs were enhanced by teams of epidemiological observers who were stationed around the world, including in China, under the United States Agency for International Development’s PREDICT program. The program was created in 2009 in a response to the H5N1 outbreak as a way to improve detection of new disease threats, improve preparedness, and promote ways to minimize practices that trigger spillover (zoonotic) events.48 Unfortunately, fieldwork ended in September 2019 after the program’s funding was eliminated.49
These two biosurveillance programs were buttressed by playbooks created by the Bush and Obama administrations—the “National Strategy for Pandemic Influenza” and “Playbook for Early Response to High-Consequence Emerging Infectious Disease Threats and Biological Incidents,” respectively. Though the technologies referred to in the guidebooks were vastly different because they are separated by 10 years, and though the Bush and Obama administrations differed in several crucial respects, their recommendations and their strategies for monitoring, containing, and (in the worst-case scenario) responding to outbreaks of transmissible and potentially deadly pathogens were very similar.46
Emergence of SARS-CoV-2 (Fall 2019-January 2020)
It is unclear exactly when or where the first human was infected with SARS-CoV-2. There have been numerous stories about different individuals playing the part of “patient zero,” as well as attempts to use indirect means to trace the virus back to an origin point, but no definitive answer has been produced yet. The consensus at this point in time seems to be that the virus began circulating in Wuhan in October or November 2019.
There is no shortage of theories that question this timeline, and in the United States alone hundreds, perhaps even thousands, of people claim that they had COVID-19 in November or December of 2019. This assumption is based on their perception that their symptoms were more severe than the typical seasonal illnesses that most people suffer from at that time of the year.50 As sick as many of these people became, it is extremely unlikely that the illness was COVID-19. All available evidence suggests that SARS-CoV-2 did not arrive in the United States until December 2019 at the earliest, which means extensive community spread in 2019 would not have been possible. An unrelated program that collected blood specimens on patients from January 2, 2020, through March 18, 2020, found that 9 out of 24,079 (0.037%) participants tested positive for SARS-CoV-2 antibodies, and that the earliest positive sample was taken on January 7, 2020, in Illinois, and January 8, 2020, in Massachusetts.51 Since it takes approximately 14 days from the time of infection for the body to develop enough antibodies to be detectable, this means infection may have occurred around December 24, 2019, or a little earlier.
Some evidence presents more significant aberrations from the generally accepted timeline. Several teams of researchers, not all of whom were searching for the origins of the pandemic, have found indications of SARS-CoV-2 circulation dating back to months before the virus was believed to have arrived in their respective regions. Brazilian researchers
found evidence of the virus in a sample of wastewater from the southern city of Florianópolis dating back to November 27, 2019.52 An Italian team screening patients for lung cancer found evidence of SARS-CoV-2 antibodies in samples dating back to September 2019.53 Finally, Spanish researchers found traces of the virus in Barcelona wastewater samples taken all the way back in March 2019.54 If any of these findings are confirmed, it would radically disrupt our understanding of how events unfolded, but contamination or false positives cannot not be ruled out at this time.
found evidence of the virus in a sample of wastewater from the southern city of Florianópolis dating back to November 27, 2019.52 An Italian team screening patients for lung cancer found evidence of SARS-CoV-2 antibodies in samples dating back to September 2019.53 Finally, Spanish researchers found traces of the virus in Barcelona wastewater samples taken all the way back in March 2019.54 If any of these findings are confirmed, it would radically disrupt our understanding of how events unfolded, but contamination or false positives cannot not be ruled out at this time.
A more unconventional attempt to reconstruct a timeline of the outbreak examined satellite images of traffic in Wuhan. These researchers found that there was increased traffic around the city’s hospitals from late August through December 2019. They also found increased online searches for symptoms associated with COVID-19, including “cough” and “diarrhea.”55 The researchers behind this claim conclude that the virus could have entered circulation in late summer 2019.
One of the more promising means of searching for an origin point was performed by researchers based at the University of California San Diego School of Medicine, the University of Arizona, and Illumina, Inc. They used epidemiological simulations and retrospective molecular clock inference to answer how long the virus had been circulating in China before it was discovered and combined three important pieces of information: a detailed understanding of how SARS-CoV-2 spread in Wuhan prior to the lockdown, the genetic diversity of the virus in China, and reports documenting the earliest cases of COVID-19 in Hubei. “By combining these disparate lines of evidence, we were able to put an upper limit of mid-October,” the authors wrote in a report that was published in Science in March 2021.56 They also found that the virus fizzled out without starting a pandemic in approximately 67% of simulations.
One of the most frequently cited accounts of a patient zero story stems from a March 2020 report from the South China Morning Post, which claimed that a 55-year-old from Hubei province was the first known person to be infected with the virus. She reportedly became ill on November 17, 2020, and while this story cannot be corroborated, and though there is no indication that this woman was the first to be infected, it does suggest that community spread could have already been occurring in Hubei as early as November 2020.40
The murkiness of the early timeline of the virus is exacerbated by the fact that the origin of the virus also continues to be an open question as of this writing. There are more theories about where the virus came from than can be addressed here, but the vast majority of them fall into one of two camps that can be generalized as coming from (1) a spillover event (zoonosis) or (2) a laboratory. Unfortunately, hard evidence to support
either is simply not available, so each must be treated as viable, even if the implications of the latter are difficult to accept. In May 2021, the nation’s top security agencies began an investigation to delve deep into the origins of the virus as more information has given more credibility to the hypothesis of a laboratory accident and a cover-up. Unfortunately, the final report was unable to conclude whether the virus emerged from a laboratory or if it was a spillover event that occurred outside of a research facility.57
either is simply not available, so each must be treated as viable, even if the implications of the latter are difficult to accept. In May 2021, the nation’s top security agencies began an investigation to delve deep into the origins of the virus as more information has given more credibility to the hypothesis of a laboratory accident and a cover-up. Unfortunately, the final report was unable to conclude whether the virus emerged from a laboratory or if it was a spillover event that occurred outside of a research facility.57
The zoonosis model claims that the SARS-CoV-2 virus was transmitted from a bat to a human, possibly at a wet market in Wuhan, in either November or very early December 2019. Based on prior pandemics, it is possible that an intermediary species may have been involved. Some have posited that the intermediary species was a Malayan pangolin, Manis javanica, and there is some evidence to support this claim. The receptor-binding domain (see Viruses below) of pangolin coronaviruses is similar to the receptor-binding domain of SARS-CoV-2. Moreover, pangolin coronaviruses have shown strong binding affinities to the human proteins that the SARS-CoV-2 virus uses to break into cells, at least one group of pangolins that was smuggled into China have tested positive for coronaviruses closely related to SARS-CoV-2, and pangolins are sold in Chinese wet markets, but there are inherent problems with this evidence, too. For one, the smuggled pangolins found to be infected with the coronavirus similar to SARS-CoV-2 may have been infected by their abductors.58 Secondly, pangolin coronaviruses do not appear to be well adapted to pangolins, suggesting limited natural intraspecies spread.59 Finally, pangolins are largely solitary animals, which would also have impeded intraspecies spread. These critiques do not discount the theory, but they do make it unlikely. Direct transmission to a human, most likely from a horseshoe bat that was captured in a relatively remote part of southern China, seems far more plausible even if direct evidence is currently lacking.60 A more detailed examination of routes of transmission will be explored in Chapter 2: Transmission of SARS-CoV-2.
The second group of origin stories support the far more controversial claim that the virus escaped from a laboratory, most likely the Wuhan Institute of Virology. This was once a third rail belief, but it is not as farfetched as many of the theories that have arisen in the wake of the COVID-19 pandemic. To discount it because it has been supported by individuals who have proposed more incoherent ideas about the virus is a case of guilt by association.
None of the central tenets of the laboratory theory are particularly outlandish. The SARS outbreak did emerge from bat populations that were traced back to southern China, and there was a legitimate concern that another coronavirus outbreak could turn into a very deadly pandemic if
a particularly rapacious virus were to jump to a human host following a spillover event. It was no secret that the Wuhan Institute of Virology was studying coronaviruses precisely for this reason. In some cases, researchers were traveling to remote parts of China to retrieve samples of bat coronaviruses that were known to be dangerous. For example, the RaTG13 coronavirus (which shares 96.2% of its genetic identity with SARS-CoV-2) was recovered from the Tongguan mineshaft in Mojiang in 2013, a year after six miners who had been working in the same tunnel cleaning guano developed a severe, pneumonia-like illness that proved fatal to three of those affected.61 Researchers working at the laboratory even wrote in a 2017 paper published in PLOS Pathogens that their work “provides new insights into the origin and evolution of SARS-CoV and highlights the necessity of preparedness for future emergence of SARS-like diseases.”62
a particularly rapacious virus were to jump to a human host following a spillover event. It was no secret that the Wuhan Institute of Virology was studying coronaviruses precisely for this reason. In some cases, researchers were traveling to remote parts of China to retrieve samples of bat coronaviruses that were known to be dangerous. For example, the RaTG13 coronavirus (which shares 96.2% of its genetic identity with SARS-CoV-2) was recovered from the Tongguan mineshaft in Mojiang in 2013, a year after six miners who had been working in the same tunnel cleaning guano developed a severe, pneumonia-like illness that proved fatal to three of those affected.61 Researchers working at the laboratory even wrote in a 2017 paper published in PLOS Pathogens that their work “provides new insights into the origin and evolution of SARS-CoV and highlights the necessity of preparedness for future emergence of SARS-like diseases.”62
The Wuhan Institute of Virology was not a minor research facility. It was extremely sophisticated and the first laboratory in China to achieve the highest level of international bioresearch safety (BSL-4) when it opened in 2017,63 but, unfortunately, it did not seem to be operated in a safe manner. Between 2017 and 2018 diplomats from the United States repeatedly visited the institute and reported back to Washington their worries about the facility. In a Politico article adapted from his book, Chaos Under Heaven, Washington Post columnist Josh Rogin noted that the two most concerning findings were that the researchers “didn’t have enough properly trained technicians to safely operate their BSL-4 lab” and that they “had found new bat coronaviruses that could easily infect human cells.”64
This would be deeply concerning on its own, but US intelligence reports have come to light claiming that three researchers from the Wuhan Institute of Virology sought hospital care in November 2019 for an illness with symptoms consistent with “both COVID-19 and common seasonal illnesses.”65 This would fall within the bounds of the generally accepted belief about when the virus was introduced to the community, but Chinese officials have denied the veracity of the report, as it would make the theory that the virus was introduced to the community via laboratory escape entirely possible. The US intelligence report has yet to be corroborated, and as of this writing, agents are actively searching for evidence to either support or disprove this hypothesis. As of September 2021, whether or not the virus escaped from a laboratory continues to be a thoroughly debated issue as facts about its origins are still coming to light.
While these two theories are vastly dissimilar, they do agree that the city of Wuhan, the sprawling capital of central China’s Hubei province, is the site of the first major outbreak of the virus, and that it was the hub from which the virus began its spread within China, and then to the rest of the world. Evidence of the spread from late December 2019 forward is relatively
well documented and will be reviewed. For those who would like a more precise version of the early months of the outbreak, it is recommended that they consult the unclassified timeline complied by the Congressional Research Service, which is freely available online.40
well documented and will be reviewed. For those who would like a more precise version of the early months of the outbreak, it is recommended that they consult the unclassified timeline complied by the Congressional Research Service, which is freely available online.40
December 2019
In December 2019, hospitals in the city of Wuhan began seeing cases of atypical pneumonia that were caused by an unknown pathogen. According to the WHO, the earliest that any patient reported symptom onset was December 8, 2019.66 Contrary to this timeline, Huang and colleagues published an online article in The Lancet at the end of January 2020 on the clinical features of patients infected with the virus claiming, “The symptom onset date of the first patient identified was December 1, 2019.”67 These two accounts indicate that the first infections were taking place in mid- to late-November 2019. Interestingly, the account from Huang and colleagues notes that none of the first patient’s family members became ill and that an epidemiological link could not be established between this patient and the others, 66% of whom had a connection to the Huanan Seafood Wholesale Market. This would suggest that the market was but one of the many locations that played a role in the beginnings of the outbreak.
Physicians from hospitals around Wuhan began taking samples from patients and sending them to commercial companies for analysis in late December 2019. At least eight patient samples were sent out to different genomics companies.68 The first completed genomic sequencing of the virus is believed to have been performed by BGI Genomics on December 29, 2019, based on a sample that was sent out on December 26, 2019. This was several days before the Wuhan Institute of Virology successfully sequenced the genome.68
Meanwhile, the earliest sample that later confirmed infection appears to have been taken on December 24, 2019, from a 65-year-old deliveryman who worked at the Huanan Seafood Wholesale Market. This patient had been admitted to the Central Hospital of Wuhan on December 18, 2019, with pneumonia and later died. The patient’s samples were sent to Guangzhou-based Vision Medicals on December 27, 2019, and a representative from the company made the unusual move of calling the hospital and speaking with the head of respiratory medicine, Dr. Zhao Su. The representative said that the company had sequenced most of the virus’s genome and they recognized that it appeared to be a novel coronavirus closely related to SARS. Several representatives from the company later visited the city of Wuhan in person and spoke directly to both hospital officials and disease control authorities.68
A separate sample, also from the Central Hospital of Wuhan, was taken from a 41-year-old patient on December 27, 2019, and sent to Beijing-based CapitalBio MedLab. Though this patient had no history of contact with the Huanan Seafood Wholesale Market, his test results, which became available on December 30, 2019, would show a false positive for SARS.68 Dr. Ai Fen, head of emergency medicine at Wuhan Central Hospital, circled the word SARS, took a photograph of the report, and shared the document with colleagues and a former classmate from Tongji Hospital.40 Earlier in the day, Ai had also recorded an 11-second clip of a CT scan of the patient and sent it to the colleague from Tongji Hospital, who had read online that the Wuhan Municipal Health Commission had issued “urgent notices” to area hospitals earlier in the day about cases of pneumonia said to be linked to the Huanan Seafood Wholesale Market. The 11-second clip and the image of the report showing a false positive for SARS quickly began spreading around the medical community in Wuhan.
A few hours later, the image and the video were sent to Ai via WeChat by an ophthalmologist colleague who also worked at Wuhan Center Hospital, but with whom she has no personal relationship. The sender, Dr. Li Wenliang, included several other recipients in the chat and encouraged them to take precautions against any potential outbreak. Li’s messages were circulated widely online, sparking uproar among average citizens who demanded to know more information about the virus. Both Ai and Li were reprimanded by senior officials, and Li was later summoned to the Public Security Bureau to sign a statement agreeing to stop “spreading rumors” or face punishment but he continued to speak out despite the danger of doing so. He was hospitalized with COVID-19 symptoms on January 12, 2020, and died on February 7, 2020, at the age of 33 years.69
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree