AL amyloidosis is the most common form of systemic amyloidosis and is associated with an underlying plasma cell dyscrasia. It is often difficult to recognize because of its many manifestations. Recent diagnostic and prognostic advances include the serum-free light chain assay, cardiac MRI, and serologic cardiac biomarkers. Treatment strategies that have evolved during the past decade are prolonging survival and preserving organ function. This article outlines the role of high-dose melphalan and stem cell transplantation. This year marks the 20th anniversary for the first patient who underwent successful stem cell transplantation for this disease at Boston Medical Center.
Key points
- •
High-dose melphalan (HDM) and autologous peripheral blood stem cell transplantation (SCT) can lead to durable remissions and long-term survival in AL amyloidosis.
- •
The morbidity and mortality of HDM-SCT in AL amyloidosis patients can be minimized with careful patient selection and center experience.
- •
Survival strongly depends on achievement of a hematologic complete response and patients with less organ involvement and absence of cardiac involvement do better.
- •
Continued efforts to refine patient selection and management, and incorporate novel antiplasma cell agents in combination or sequentially, should further improve prognosis in AL amyloidosis.
Introduction
The amyloidoses are a group of diseases that share a common feature of extracellular deposition of pathologic, insoluble, fibrils in many tissues and organs. These fibrils have a characteristic beta-pleated sheet configuration that stains with the Congo red dye, producing apple green birefringence under polarized light microscopy. Classification of the amyloidoses is based on the precursor protein that forms the amyloid fibrils, and the distribution of amyloid deposition (systemic or localized).
AL amyloidosis (ie, immunoglobulin light chain amyloidosis) is the most common form of systemic amyloidosis in the United States and Europe. Although AL amyloidosis is considered an uncommon disease, it has an incidence similar to Hodgkin lymphoma or chronic myelogenous leukemia. It affects 5 to 12 persons per million per year, although autopsy studies suggest that the actual incidence might be higher. The annual incidence of AL amyloidosis in Olmstead County, Minnesota, is 8 in a million patients. The amyloidogenic precursor protein in AL amyloidosis is an immunoglobulin light chain or a fragment of light chain, usually the variable region, produced by the clonal plasma cell population in the bone marrow. The plasma cell burden in this disorder is usually low (5%–10%), although AL amyloidosis can be associated with multiple myeloma in 10% to 15% of cases.
Introduction
The amyloidoses are a group of diseases that share a common feature of extracellular deposition of pathologic, insoluble, fibrils in many tissues and organs. These fibrils have a characteristic beta-pleated sheet configuration that stains with the Congo red dye, producing apple green birefringence under polarized light microscopy. Classification of the amyloidoses is based on the precursor protein that forms the amyloid fibrils, and the distribution of amyloid deposition (systemic or localized).
AL amyloidosis (ie, immunoglobulin light chain amyloidosis) is the most common form of systemic amyloidosis in the United States and Europe. Although AL amyloidosis is considered an uncommon disease, it has an incidence similar to Hodgkin lymphoma or chronic myelogenous leukemia. It affects 5 to 12 persons per million per year, although autopsy studies suggest that the actual incidence might be higher. The annual incidence of AL amyloidosis in Olmstead County, Minnesota, is 8 in a million patients. The amyloidogenic precursor protein in AL amyloidosis is an immunoglobulin light chain or a fragment of light chain, usually the variable region, produced by the clonal plasma cell population in the bone marrow. The plasma cell burden in this disorder is usually low (5%–10%), although AL amyloidosis can be associated with multiple myeloma in 10% to 15% of cases.
Treatment targets
A detailed elaboration of the pathogenesis of AL amyloidosis is beyond the scope of this article. However, each of the steps in the pathogenesis of amyloidosis, from the production of the precursor protein to formation of amyloid deposits, is a potential target for treatment. Preclinical and clinical studies are being designed or are ongoing for several of these targets. Reducing the amyloidogenic precursor protein (ie, light chains produced by the clonal plasma cell dyscrasia) with chemotherapeutic agents has been used for the past several decades. Several interventions aimed at facilitating degradation of the amyloid deposits have been reported in AL amyloidosis. A detailed description of all the treatment options is beyond the scope of this article, which is focused on targeting the clonal plasma cell dyscrasia.
Treatment: general principles
The keys to effective treatment of AL amyloidosis are early diagnosis and correct typing. Ideally, treatment should be started before irreversible organ damage has occurred. Once the diagnosis of AL has been firmly established, the design of the therapeutic strategy depends on a fine balance between the efficacy of the chosen regimen and the individual patient’s expected ability to tolerate the toxicity of the treatment regimen, especially in the setting of cardiac involvement with amyloidosis. The current therapeutic approach to systemic AL amyloidosis is based on the observation that organ function is restored if the synthesis of the amyloidogenic protein precursor is shut down. Therefore, the aim of therapy is to rapidly reduce the supply of misfolded amyloid-forming monoclonal free light chains by suppressing the underlying plasma cell dyscrasia while using supportive measures to preserve target organ functions.
Monitoring the therapeutic effect
The criteria for hematologic and organ responses have been unified, formalized, and recently updated at the XIIth International Symposium on Amyloidosis. Hematologic response usually translates into clinically improved organ function and is associated with a substantial survival advantage and improved quality of life. However, if the organ damage is advanced, it may be irreversible despite hematologic remission. Most patients with a hematologic response show a clinical response after 3 to 6 months, although late responses have been observed. Even though partial hematologic responses can be beneficial, it seems that significant reductions in free light chain levels are associated with the best clinical responses. However, the rate of clinical response is higher in patients with a complete hematologic response than in those with a partial one.
Initial pilot studies of high-dose chemotherapy and stem cell transplantation in AL amyloidosis
Intravenous high-dose melphalan (HDM) chemotherapy and autologous peripheral blood stem cell transplantation (SCT) has been successful in inducing complete hematologic remissions and prolonging survival in multiple myeloma. Therefore, it was logical to apply this approach to the treatment of AL amyloidosis. The Amyloid Research and Treatment Program, now called the Amyloidosis Center, at Boston University School of Medicine, has a long-standing investigative interest in the pathophysiology and treatment of the various forms of systemic amyloidoses. In 1994, a multidisciplinary clinical group was formed at Boston University Medical Center to develop high-dose chemotherapy protocols for AL amyloidosis. This group was made up of clinicians allied with the Amyloid Research and Treatment Program, representing the disciplines of cardiology, nephrology, pulmonology, neurology, gastroenterology, and rheumatology, together with hematologists in the Stem Cell Transplant Program of the Section of Hematology and Oncology and clinical pathologists from the Apheresis and Blood Bank.
The initial experience with HDM-SCT in 5 subjects with AL amyloidosis was reported in 1996. This pilot study showed that AL amyloidosis subjects with significant systemic disease could be successfully treated with HDM-SCT. Furthermore, 3 of the 5 subjects achieved a complete hematologic response (CR), with disappearance of their underlying clonal plasma cell disorder following treatment. Moreover, all 5 subjects experienced reversal of amyloid-related organ dysfunction.
Cumulative experience of high-dose melphalan and stem cell transplantation at a single center
An expanded series with 312 subjects was conducted by the Amyloidosis Center in 2004. Hematologic complete response (CR) occurred in 40% of evaluable subjects and 66% of the subjects achieved improvement in at least 1 organ function with a hematologic CR. Moreover, the median survival was 4.6 years for this cohort.
The long-term follow-up of 80 subjects treated in the first 3 years of the program (1994–1997) was reviewed. The early death rate, within 100 days of SCT, was 14%. Hematologic CR was achieved by 51% (32 of 63) and the median survival was 4.75 years. The median survival exceeded 10 years for subjects achieving a CR after HDM-SCT, compared with 50 months for those not achieving a CR. The long-term survival beyond 10 years was achieved in 23.5% (95% CI, 15% and 33%) of subjects with AL amyloidosis treated with HDM-SCT. Hematologic relapses occurred in 34% (n = 11/32) subjects at a median time of 2.5 years (range 2–8).
Recently, the outcomes of 421 subjects treated with HDM-SCT from July 1994 to December 2008 were analyzed. Treatment-related mortality was 11% overall and decreased to 6% in the last 5 years. For this group, the median event-free survival (EFS) and overall survival (OS) were 2.6 and 6.3 years, respectively. Of 340 subjects evaluable at 1 year beyond HDM-SCT, 43% achieved a CR and 78% of them experienced an organ response. For CR subjects, median EFS and OS were 8.3 and 13.2 years, respectively. Among the 195 subjects who did not obtain CR, 52% reached an organ response, and the median EFS and OS were 2 and 5.9 years, respectively. A subgroup of 26% of the non-CR subjects remained clinically stable at 5 years of follow-up. Hematologic relapses occurred in 40 subjects (28%) at a median time of 3.7 years (range, 1.5–12.7).
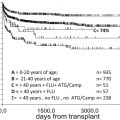
Most recently, long-term outcomes of 607 subjects with AL amyloidosis undergoing HDM-SCT from July 1994 to Aug 2013 were analyzed. The median age was 57 years. Of these, 53% had cardiac involvement and 41% had multiorgan involvement. Treatment-related mortality was 9% and 80% of the deaths were associated with cardiac involvement. Hematologic CR was achieved by 34% by an intention-to-treat analysis. Hematologic CR was 45% for those who received 200 mg/m 2 of melphalan compared to 33% for those who received 100 to 140 mg/m 2 melphalan ( P = .02). The median OS was 6.7 years. The median OS was significantly better for those who achieved a hematologic CR, for those without cardiac involvement, and for those with less than 2 organ systems involvement ( Figs. 1–3 ). Hematologic relapses occurred in 20% of subjects with hematologic CR at a median of 4 years (range 1.6–12.4 years).
Eligibility criteria for high-dose melphalan and stem cell transplantation
The Amyloidosis Center eligibility criteria for treatment with HDM-SCT are a confirmed tissue diagnosis of amyloidosis, clear evidence of a clonal plasma cell dyscrasia, age greater than 18 years, and minimum measures of performance status (Southwest Oncology Group [SWOG] 0–2), cardiac function (left ventricular ejection fraction >40%), pulmonary function (oxygen saturation >95% on room air), and hemodynamic stability (baseline systolic blood pressure >90 mm Hg). Patients on hemodialysis or peritoneal dialysis for renal failure are not excluded if other eligibility criteria are met. The dose of melphalan can vary from 100 to 200 mg/m 2 based on the risk-adapted approach, described by Comenzo and Gertz, to reduce treatment-related morbidity and mortality associated with HDM-SCT. The patients can be stratified into 3 risk categories: (1) good-risk patients are of any age and have 1 to 2 organs involved, no cardiac involvement, and creatinine clearance greater than 50 mL/min; (2) intermediate-risk patients are less than 71 years old and have 1 to 2 organs involved, 1 of which must include cardiac or renal with creatinine clearance less than 51 mL/min; and (3) poor-risk patients have either 3 organs involved or advanced cardiac involvement. The cardiac biomarker staging system can also define risk of treatment-related complications while undergoing HDM-SCT. Elevated cardiac troponin T levels are associated with poor survival while undergoing HDM-SCT.
Induction regimens, choice, and duration
Because the burden of clonal plasma cells is modest in most patients with AL amyloidosis, induction with a cytoreductive regimen before HDM-SCT, as is done in multiple myeloma, seems unnecessary, although possible benefits from infusional vincristine, adriamycin and dexamethasone (VAD) treatment before SCT have been reported. Evidence from a randomized clinical trial indicates that the delay associated with pretransplant cytoreduction, using oral melphalan and prednisone, can allow disease progression and can lead to survival disadvantage in patients with cardiac involvement. Induction therapy with novel agents before HDM-SCT, specifically bortezomib and dexamethasone, is being explored in the setting of a clinical trial and data seem promising. However, induction therapy should be used with caution so that it does not cause delay of more definitive treatment or deterioration of organ function.
Stem cell mobilization and collection
Previous exposure to alkylating agents impairs hematopoietic stem cell collection. A total dose of oral melphalan exceeding 200 mg may significantly reduce the ability to mobilize CD34+ cells. Contrary to the common experience in multiple myeloma, deaths have been reported during mobilization and leukapheresis of patients with AL amyloidosis who have cardiac or multiorgan involvement. Overall, the incidence of major complications during stem cell mobilization and collection is approximately 15%. To minimize the risk of toxicity, it is recommended that only granulocyte colony-stimulating factor (G-CSF) be used for mobilization because its use in combination with cyclophosphamide is associated with increased cardiac morbidity, a significantly higher number of aphereses required for CD34 harvesting, greater need of hospitalization, and increased toxicity. However, cyclophosphamide may have a role in stem cell mobilization in patients with AL amyloidosis and multiple myeloma. The recommended dosage of G-CSF is 10 to 16 mcg/kg/d, either as a single dose or in 2 divided doses, 3 days before stem cell collection. The recommended optimal dose of CD34+ cells in AL patients is at least 5 × 10 6 CD34+ cells/kg. Contamination of the apheresis product with clonotypic plasma cells has been demonstrated but CD34 selection is not presently recommended. Plerixafor, CXCR4 receptor antagonist, as a stem cell mobilization regimen has not been studied in subjects with AL amyloidosis in a well-designed clinical trial ; however, it can be beneficial in patients with fluid overload to reduce the dose of G-CSF, reduce the risk of capillary leak syndrome, and reduce the number of leukapheresis sessions needed for optimal stem cell collection yield.
Conditioning regimens before stem cell transplantation
Total body irradiation (550 cGy) before SCT was investigated in a small feasibility study; however, it is not used in current regimens because of cardiac toxicity and what seems to be greater overall morbidity and mortality. Thus, conditioning is usually performed with intravenous melphalan alone, using a risk-adapted dose-modification schema. Tandem cycles of HDM have shown to improve the proportion of subjects who ultimately achieve a hematologic CR in 31% of subjects, leading to overall CR rate of 67%. A pilot study of incorporation of bortezomib with HDM in the treatment of AL amyloidosis has shown promising results with high hematologic response rates.
Clinical responses to high-dose melphalan and stem cell transplantation
The initial report of renal responses following HDM-SCT was published in 2001. In this report, 36% of patients had a renal response at 12 months defined as a 50% reduction in 24-hour urinary protein excretion in the absence of a 25% or greater reduction in creatinine clearance. There was a striking difference in renal response rate among those with a complete hematologic response (71%) and those with persistence of the plasma cell dyscrasia (11%). Since then, reports of improvements in quality of life, hepatic responses, and cardiac responses have been published. Similar to renal response, clinical responses in other organ systems are more evident with hematologic responses and can take up to 6 to 12 months or longer to occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree