Allogeneic hematopoietic stem cell transplantation has been shown to be curative for well-described as well as newly discovered immunodeficiencies. However, it is difficulty to define a universal transplant regimen given the rarity of these disorders and the varied pathophysiology these disorders encompass. This article discusses those primary immunodeficiencies most commonly treated by hematopoietic stem cell transplant and describes the transplant issues specific to these disorders.
Key points
- •
Transplantation is curative for many types of immunodeficiency.
- •
Conditioning regimens should vary depending on the disease and patient condition.
- •
Full donor engraftment may not be required for cure.
- •
Outcomes improve with earlier transplant before infection and/or end-organ damage.
Introduction
The first hematopoietic stem cell transplants (HSCT) for patients with primary immunodeficiencies (PIDS), specifically severe combined immunodeficiency (SCID) and Wiskott-Aldrich syndrome (WAS), were performed in 1968. Since then, HSCT has been regularly used to treat a growing spectrum of immunodeficiencies. A recent Primary Immune Deficiency Treatment Consortium (PIDTC) survey reported more than 1000 patients transplanted in North America alone for SCID, WAS, or chronic granulomatous disease (CGD), which are the three most common types of PID.
Further, more than 200 distinct immunodeficiencies have now been described and at least 10 new genetic forms of PIDS are described each year: many of these new diseases have successfully been treated by HSCT. Thus transplantation is a major treatment option for patients with genetic mutations in cells of the hematopoietic system that lead to an impaired immune response. However, the rarity of these disorders and the unique aspects intrinsic to each disease make it difficult to define a universal transplant regimen. This article discusses those PIDs most commonly treated by HSCT and disease-specific issues regarding transplantation for these patients.
Introduction
The first hematopoietic stem cell transplants (HSCT) for patients with primary immunodeficiencies (PIDS), specifically severe combined immunodeficiency (SCID) and Wiskott-Aldrich syndrome (WAS), were performed in 1968. Since then, HSCT has been regularly used to treat a growing spectrum of immunodeficiencies. A recent Primary Immune Deficiency Treatment Consortium (PIDTC) survey reported more than 1000 patients transplanted in North America alone for SCID, WAS, or chronic granulomatous disease (CGD), which are the three most common types of PID.
Further, more than 200 distinct immunodeficiencies have now been described and at least 10 new genetic forms of PIDS are described each year: many of these new diseases have successfully been treated by HSCT. Thus transplantation is a major treatment option for patients with genetic mutations in cells of the hematopoietic system that lead to an impaired immune response. However, the rarity of these disorders and the unique aspects intrinsic to each disease make it difficult to define a universal transplant regimen. This article discusses those PIDs most commonly treated by HSCT and disease-specific issues regarding transplantation for these patients.
Severe Combined Immunodeficiencies and Related Disorders
SCID comprises several disorders mainly characterized by a lack of functional T cells caused by (1) a failure to produce cytokines necessary for T-cell maturation (interleukin [IL]-2 receptor common gamma chain, Jak3, and IL7RA deficiencies) (2) accumulation of toxic purine metabolites (Adenosine Deaminase [ADA]-SCID), (3) defective differentiation of a neutrophil/T-cell precursor (reticular dysgenesis), or (4) defective VDJ rearrangements (Rag2, Rag2, Artemis). SCID disorders can also be characterized by the presence or absence of natural killer (NK) or B cells.
Patients with these disorders usually do not survive beyond the first year of life. The only chance of long-term survival is immunologic reconstitution by normal T cells. The SCID genotype has significant implications on the need for conditioning and transplant outcome. Although immunosuppression is typically not required for these patients because the absence of T lymphocytes prevents graft rejection, there are some SCID variants in which immunosuppressive agents may be required to facilitate long-term immunoreconstitution. Preexisting infections, particularly viral infections, such as cytomegalovirus (CMV) or adenovirus, may limit the ability to use myeloablative chemotherapy conditioning, although reduced intensity conditioning (RIC) may be tolerated. In addition, maternal engraftment of leukocytes during pregnancy is common in some SCID genotypes because there are no autologous T cells to reject transplacental maternal T cells. Maternal T lymphocytes do not provide effective immunity, but may cause maternofetal graft-versus-host disease (GvHD) manifesting as an eczematous rash, splenomegaly, and occasionally pneumonitis or other complications. There is also the potential complication of a graft-versus-graft (GvG) reaction depending on the donor used. Infusion of unfractionated human leukocyte antigen (HLA)–identical sibling marrow can lead to rejection of the maternal T lymphocytes, with or without a clinical GvG reaction. Using a maternal donor can result in rapid immune reconstitution with or without GvHD that is usually amenable to treatment with low-dose steroids. In contrast, rejection of a paternal graft can occur either with or without a clinical GvG reaction.
The best donor is an HLA-matched sibling donor, with a 90% overall survival rate in the most favorable circumstances. When a matched sibling or family donor is unavailable, an alternative donor is necessary. Given the lack of autologous T cells and the ready availability of a parental donor, haploidentical transplants are a common choice. Bone marrow grafts depleted of T cells were studied prospectively resulting in an 81% overall survival with 77 patients having received a haploidentical graft and 12 using an HLA-matched related donor. All grafts were infused without preconditioning (except for 2 receiving placental blood) or posttransplant GvHD prophylaxis and most deaths occurred within 12 months following transplantation, most from preexisting infection. Note that 68 of the 72 had normal T-cell function but 45 of the 72 survivors required intravenous immunoglobulin replacement. Although this method means that patients without an HLA-identical sibling donor can be offered transplantation and cure, there is a significant, albeit diminishing, mortality risk associated with T lymphocyte–depleted transplants.
The results from HSCT are superior when the procedure is performed early, before end-organ damage occurs from infection. Twenty-one infants diagnosed early because of a positive family history were transplanted within 28 days of birth, 16 of whom had IL-2 receptor gamma chain–deficient or JAK3-deficient SCID, and all received T lymphocyte–depleted stem cells, without any conditioning or GvHD prophylaxis. Twenty patients (95%) survived, with a maximum follow-up of 19 years. A 2-center study from the United Kingdom similarly compared outcomes of 48 probands and 60 older affected siblings with an overall survival in the early transplants of 90% versus 60% in the older siblings. A recent report from the PIDTC on 240 children with SCID transplanted between 2000 and 2009 showed that survival in older patients was as good as in those transplanted at less than 3 months, as long as they were infection free or previous infection had cleared. Initiatives to mandate testing for SCID at birth are therefore underway in many US states and Canadian provinces.
Attempts to perform in utero transplantation have been made in patients with a positive family history of SCID. However, confirming the diagnosis requires invasive procedures, which can lead to fetal loss, and T lymphocytopenia with diminished mitogen response has been reported after some procedures, leaving the patient at risk of opportunistic infection. Furthermore, occult maternofetal T-lymphocyte engraftment may lead to graft rejection, and obtaining maternal stem cells to treat the patient is not feasible during pregnancy. GvHD is also undetectable in utero, and treatment via the mother and monitoring of the fetal responses are either not possible or impractical. Thus, for those patients with a positive family history, the preferred option is to confirm the diagnosis, initiate prophylactic antimicrobial treatment at birth, and search for a donor to perform a transplant as soon as possible.
More recently with high sequencing analysis of HLA, the results of matched unrelated donor transplantation using adult donors or umbilical cord blood (UCB) is gaining support as a viable alternative. HSCT using HLA-matched unrelated donors provides similar results to those of HLA-matched siblings. UCB products that are already banked are more readily available, allowing early transplantation. Fernandes and colleagues compared the results of UCB transplant with mismatched related donor transplant in a retrospective study involving 249 transplants (74 UCB vs 174 mismatched related donor). Most UCB transplants were done with a myeloablative conditioning regimen and recipients had a higher frequency of complete donor chimerism and faster lymphocyte count recovery, but there was a trend toward more severe acute GvHD and more chronic GvHD. The 5-year survival rates were similar at 62% for mismatched related donor transplant versus 57% for UCB.
In addition, the role of conditioning remains undetermined. Although comprehensive studies are lacking, certain tenets apply and considerations for pretransplant conditioning include the presence of infection or end-organ damage, the molecular diagnosis, the type of donor available, the likelihood of full immune reconstitution, and the risk of short-term and long-term side effects. In a multicenter study between the United States and Europe of 103 patients with SCID, infusion of stem cells from an unrelated donor restored T-lymphocyte immune reconstitution, although the risk of GvHD was significantly higher than when a matched related donor was used. A study of 77 patients with SCID in the United Kingdom, who received stem cell infusions, showed a 90% survival in matched sibling donor/matched family donor transplants but only 60% when alternative donors were used. Infants with NK − SCID were more likely to survive and had high-level donor T-cell chimerism with superior long-term recovery of CD4 T-cell immunity than NK + recipients. A third of patients with NK + SCID required additional transplant procedures.
In a series of 98 patients with SCID, 32% received pretransplant chemotherapy conditioning: the rate of engraftment was significantly higher in these patients than in nonconditioned patients, but overall survival was less, mainly because of infection-related deaths. More recently, European centers have described the outcome of transplantation for 699 patients with SCID, of whom 25% had a T-B- phenotype, and of whom 42% received conditioning. There was no survival advantage for the nonconditioned patients. A small single-center study of 24 patients, of whom at least half had T-B- SCID, showed more favorable outcomes for patients who received conditioning and, in a multicenter study of 178 patients with SCID, the molecular diagnosis significantly affected outcome. Patients with T-B- SCID had worse survival, with diminished rates of stem cell engraftment, and slower T and B lymphocyte immune reconstitution, but there a better overall rate of cure of disease in patients who had received conditioning. These findings were replicated in the most recent European report.
In NK-SCID (IL-2, Jak3, IL7RA, ADA-SCID), prethymic and early intrathymic stromal niches are vacant and thus available for donor T-lymphocyte precursor engraftment, leading to sustained donor-derived thymopoiesis in the absence of myelopoiesis. In contrast, in NK+ SCID caused by VDJ recombination defects, later stages of T-lymphocyte differentiation are blocked; therefore, without conditioning, high numbers of DN2/DN3 cells compete with donor T-lymphocyte progenitors for thymic niches, resulting in a restricted T-cell repertoire and reliance on postthymic T-lymphocyte expansion. Infusion of large doses of stem cells as well as other stromal factors aids engraftment of donor stem cells and improves immune reconstitution. Myeloid engraftment, most often achieved following conditioning, facilitates engraftment of donor stem cells, permitting long-term thymopoiesis, even in NK- SCID phenotypes.
Moreover, although restoration of T lymphocytes occurs following infusion of T-depleted stem cells, many patients with nonconditioned transplants fail to gain functional B lymphocytes, particularly patients with VDJ recombination defects. Recipient B lymphocytes have reduced numbers of memory and isotype-switched B lymphocytes, and poor antibody responses to antigen stimulation, compared with donor-derived B lymphocytes. In contrast, recipient B lymphocytes from patients with IL7RA-deficient SCID are able to function in the presence of donor T lymphocytes and produce antibody to appropriate antigen stimulation. Also, patients with IL-2 receptor gamma chain–deficient or JAK3-deficient SCID without conditioning can develop B lymphocyte function, likely because of donor B-lymphocyte microchimerism. In contrast, not all conditioned transplants achieve donor B lymphocyte engraftment and independence from immunoglobulin replacement.
Patients with ADA-deficient SCID differ from those with other molecular defects because accumulation of toxic metabolites causes common lymphoid precursor toxicity leading to abnormalities of T, B, and NK lymphocyte development and function. In addition, patients often have preexisting inflammatory pneumonitis caused by the metabolic defect. In a retrospective multicenter study of 106 infants with ADA-deficient SCID, outcomes were better for patients who had matched sibling and family donors than matched unrelated or T lymphocyte–depleted donors. Superior survival was seen in patients who received nonconditioned transplants rather than myeloablative procedures. When using haploidentical donors without conditioning, nonengraftment was a major problem, although donor B-lymphocyte engraftment was achieved even after nonconditioned transplants.
In addition, the use of chemotherapeutic agents, even when beneficial, has long-term implications. Patients with Artemis-deficient SCID experience significant long-term sequelae following the use of alkylating agents, including significant growth failure, dental problems, and autoimmunity; findings that are not associated with nonconditioned transplants. Impaired fertility is associated with many of the conditioning agents used, although detailed information from the SCID cohort is not available. Moreover, the long-term risk of malignancy may be increased, at least in some patients who receive irradiation as part of the preconditioning regimen, but the only data are anecdotal. Therefore, more studies are needed to delineate specific long-term immunologic and general health outcomes in large cohorts of patients with the same molecular diagnoses, conditioning regimens, and donors. In addition, more data are needed on the use of nonmyeloablative regimens or RIC so that optimum treatment can be offered to appropriate patient groups.
Non–severe combined immunodeficiencies
In general, patients with non-SCID disorders have at least some residual T lymphocyte–mediated immunity, thus requiring the use of at least some immunosuppression and/or conditioning to ensure engraftment of donor cells. In addition, there is often sufficient time to look for alternative nonfamily adult matched donors or cord blood stem cell units from national and international registries. Moreover, depending on the genetic defect, full donor chimerism may not be necessary to restore immune function. This aspect, combined with improvements in conditioning regimens, has resulted in the use of RIC with good outcomes. In addition, T lymphocyte–depleted haploidentical donors were not used in these conditions because of the risk of nonengraftment or rejection. These patients are often older with preexisting viral infections, and T-lymphocyte depletion prolongs the time to reconstitution, thus increasing the risk of death from disseminated viral infection. However, several groups have been investigating modified grafts depleting specific T-cell subsets, while keeping others to maintain engraftment and antiviral activity, or using posttransplant cyclophosphamide to reduce reactive T cells after the graft infusion.
Wiskott-Aldrich Syndrome
WAS protein (WASP) is expressed in hematologic cells and is necessary for cellular activation and production of cell synapses. Without WASP activation, cells have difficulty migrating and signaling appropriately, leading to recurrent infections as well as thrombocytopenia and autoimmunity.
The median life expectancy for patients with WAS is only 15 years without successful immune reconstitution following HSCT. Transplantation using related HLA-matched donors leads to survival rates of 71% to 80%. As with all other PIDs, HLA-matched unrelated donors including UCB have also been used to treat patients with WAS. Patients transplanted at an earlier age, and those without infection-related damage, do better. Although there are data showing a significantly worse 5-year survival for patients who are transplanted after age 5 years, this may be more related to the presence of more end-organ damage in the older patients than actual age. Transplants using T lymphocyte–depleted HSCT from HLA-mismatched family donors had previously been less satisfactory, with survival rates between 37% and 55%. However, a multicenter study of 194 patients showed comparable results for matched family or unrelated donors, and significant improvement in survival with T lymphocyte–depleted HLA-mismatched family donors, particularly in transplants performed since 2000. Only a myeloablative conditioning regimen facilitates sufficient donor stem cell and stable multilineage engraftment fully correcting the hematological and immunologic defects, but 10% of patients still reject the graft, and more develop mixed or split donor cell chimerism. Autoimmunity is common in long-term survivors after transplantation, particularly for those with persistent mixed or split donor chimerism after receiving stem cells from a matched unrelated donor.
CD40 Ligand
CD40 ligand is expressed on activated T cells and is necessary for the proliferation and isotype switching of B cells in response to T-cell antigens. As a result, patients are unable to switch from making immunoglobulin (Ig) M to making IgG, IgA, or IgE and have a variable defect in T-lymphocyte and macrophage maturation. CD40 ligand–deficient patients are susceptible to infection from a wide variety of pathogens, including parasites like cryptosporidium, and are also at increased risk for developing autoimmune disorders and malignancies. Replacement gamma globulin is the standard treatment but the only curative option is HSCT.
To date, the largest reported series of transplants consists of 38 patients from 8 European countries. The cohort was heterogenous in terms of age and physical condition at time of transplant, donor type, and conditioning regimen used. Of the 38, 21 had significant preexisting respiratory or hepatic disease. Overall survival was almost 70%, although 4 patients experienced autologous reconstitution. Cure of the disease was achieved in 58% of the cohort. The presence of lung disease, but not liver disease, as well as an HLA-mismatched donor correlated with poor survival. The outcome for patients with an HLA-matched unrelated donor was the same as for those with an HLA-matched sibling. There were too few patients included in the study to determine the optimum conditioning regimen.
Patients have also been successfully transplanted using RIC. These regimens may reduce the risk of toxicity in sick patients, but there is a risk of rejection, which was a significant problem in the European series. Cryptosporidial infection can complicate the transplant procedure in these patients even when initial pretransplant testing of stool was negative by microscopy. Patients with severe liver damage who are too sick to tolerate HSCT can receive an orthotopic liver graft before HSCT but once liver transplant has been achieved HSCT should proceed promptly to prevent cryptosporidial infection in the transplanted liver. In addition, there is a report of 1 patient undergoing a successful transplant using a haploidentical donor with T-cell depletion and using T-cell add backs to establish full donor chimerism as well as to help clear a CMV reactivation.
Chronic Granulomatous Disease
Mutations in one of the 6 genes responsible for the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex results in a phagocyte disorder predisposing patients to risk from specific bacterial and fungal infections. Patients also have a higher incidence of autoimmune or inflammatory disorders, including pneumonitis or colitis as well as the development of granulomas, which can lead to luminal obstruction. Standard management includes use of prophylactic antibiotics; antifungals; immunosuppressants for the granuloma or autoinflammatory problems; and, in the United States, interferon gamma. At present, the only available cure is HSCT.
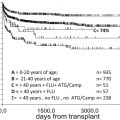
From 1973 until 2011 approximately 99 transplants (not including cord blood transplants) were performed for CGD, and 50 of those occurred in the last 10 years. The first large multicenter study described the results in 27 patients using a myeloablative regimen except for 4 patients with RIC, 2 of whom lost their grafts. Thus the recommendation at that time was to use myeloablative conditioning regimens. Investigators at the National Institutes of Health (NIH) showed the feasibility of using a nonmyeloablative regimen and HLA-matched sibling donors, particularly in high-risk patients, including those with an ongoing infection.
As in other disorders, matched unrelated donor transplants are also being considered more frequently and the largest multicenter study to date reported results in 56 patients with CGD undergoing either related (21) or unrelated (35) donor transplantation. The nonmyeloablative conditioning regimen consisted of targeted-dose busulfan with fludarabine and serotherapy, and resulted in a 93% overall survival with 75% of the patients being categorized as high risk (presence of ongoing infection or active autoinflammatory process).
UCB transplants have also been performed, first reported in 1999. An 8-year-old boy was conditioned with 10 Gy of total body irradiation (TBI), combined with antithymocyte globulin (ATG) and Cytoxan, but died at day 51 because of infection. Since then a total of 11 reported patients have undergone cord blood transplantation from either related or unrelated donors. Several patients have required retransplantation because of graft failure, but all have done well with either autologous recovery or engraftment after a second transplant. Given these results, it seems that a myeloablative regimen is necessary for UCB.
For many immunologists and pediatricians, the decision as to whom to refer for transplant is still not clear. This disorder is not fatal, and, although it is associated with a shortened life expectancy and significant morbidity, several patients have long infection-free periods and can have a good quality of life. Although the overall survival was the same between transplanted versus nontransplanted patients, quality of life seemed to be better in the transplanted group. Moreover, investigators at NIH, using a cohort of more than 200 patients, correlated outcomes with the percentage of oxidase production, showing a significant increase in mortality with lower oxidase production. This finding suggests that patients with lower oxidase production would benefit from transplantation and the PIDTC is now implementing a multicenter study to investigate the role of transplantation in the management of patients with CGD compared with standard medical therapy in cohorts with the same level of oxidase production.
DNA Repair Disorders
Several disorders result from mutations in DNA double-strand break repair genes. The disorders give rise to a combination of immunodeficiency and a predisposition to leukemia or lymphoma; HSCT abolishes this risk, but coexistent multisystemic abnormalities including microcephaly and learning disability remain. The underlying DNA repair defect results in exquisite sensitivity to alkylating agents and radiotherapy, similar to patients with Fanconi anemia.
In particular, patients with double-strand break repair disorders are generally intolerant of myeloablative or TBI-containing conditioning regimens. Patients with Nijmegen breakage syndrome have been successfully transplanted with RIC regimens and there are a few reports of successful transplant for patients with DNA ligase 4 or cernunnos-XLF deficiency, with best results achieved when using RIC. Outcome from transplant for dyskeratosis congenital was reported for a cohort of 34 patients. A range of donors, stem cell sources, and conditioning regimens was used, and there was a high incidence of GvHD and other transplant-related complications, with a 10-year survival of only 30%. Conditioning regimen intensity and transplants from mismatched related or unrelated donors were associated with early mortality. A smaller cohort with shorter follow-up showed survival of 78% following HSCT using HLA-matched unrelated donors and RIC. Similar to patients with Artemis-SCID, careful follow-up is required to determine whether problems are seen in the radiosensitive patient cohorts.
Hemophagocytic Syndromes
The familial hemophagocytic syndromes include diseases of disordered cytotoxicity, X-linked lymphoproliferative (XLP) disease, and X-linked inhibitor of apoptosis protein (XIAP) deficiency. Hemophagocytic lymphohistiocytosis (HLH) is characterized by multisystem inflammation resulting from prolonged and excessive activation of antigen-presenting cells (macrophages, histiocytes) and CD8+T lymphocytes. Initial treatment of HLH should be antiinflammatory, usually with steroids, etoposide, or ATG and cyclosporine, with prompt transition to HSCT once the disease is controlled. Poor outcome is particularly associated with the use of T-depleted haploidentical grafts, and active disease at the time of transplantation but successful outcome leads to long-term remission, even with less than 50% donor chimerism. In one single-center study, an RIC was associated with a better outcome with less acute GvHD experienced. Patients who had RIC required donor lymphocyte infusions more often than those receiving myeloablative chemotherapy, but 3-year survival was better at 92% versus 43%. Forty-three patients transplanted for XLP showed a survival of 80%, but only 50% for those presenting with HLH, with no difference in survival between those receiving a myeloablative or RIC regimen in this study. Patients with XIAP have poor outcomes after transplantation, particularly those receiving myeloablative conditioning, with most deaths caused by transplant-related toxicities. Best results are seen for those patients whose HLH was controlled and transplanted using RIC. Antibody-based conditioning regimens may improve the outcome in these patients, even when HLH is uncontrolled. Patients transplanted for HLH secondary to Griscelli syndrome type 2 or Chédiak-Higashi syndrome can be immunologically cured but neurologic disease may develop or progress, even with full donor chimerism.
FOXP3
Mutations in the FOXP3 gene result in a rare disorder known as IPEX (immune, polyendocrinopathy, X-linked). FOXP3 is necessary for the generation of regulatory T-cells and their lack leads to multiorgan autoimmunity. Severe enteropathy is the predominant feature, although the manifestations can vary. Although symptoms can be ameliorated by immunosuppression, transplantation is curative and can prevent progression of the endocrinopathies. Transplant has an overall survival of 80% with either related or unrelated donors, including the use of cord blood and using myeloablative as well as nonmyeloablative regimens. The preferred donor source and conditioning regimen are undetermined given the small numbers to date.
Dedicator of Cytokinesis-8
Mutations in the dedicator of cytokinesis-8 (DOCK8) were first described in 2009 by NIH investigators. Although the exact role of this gene is unknown, patients have low absolute T-cell counts and often a decreased number of NK cells, along with a mild to moderate eosinophilia and high IgE levels. Patients with DOCK8 mutations are characterized by cutaneous and sinopulmonary infection with bacterial organisms as well as extensive cutaneous viral infections. Patients often die of squamous cell carcinomas or hematological malignancies as well as of infections.
To date, there are at least 9 reported patients who have undergone transplantation. Two patients were transplanted using a CD66 yttrium labeled antibody with fludarabine, melphalan, and ATG. Both are doing well 2 years or more after transplantation. In Boston, an 8-year-old girl received a sibling HLA-matched product after a myeloablative conditioning regimen but died of Klebsiella pneumoniae sepsis. Another patient underwent a fludarabine/busulfan-based transplant with 200 cGy radiation and has a normal posttransplant phenotype, but at 6 years has only 6% donor myeloid chimerism despite 98% lymphoid engraftment. Further, both haploidentical and unrelated donor transplants have been performed successfully for this disease.
Investigators at the NIH have also performed several transplants using both related and unrelated HLA-matched donors and a nonmyeloablative conditioning regimen with promising results (Dennis Hickstein, personal communication, 2014). They are now looking to expand their transplant program, using haploidentical transplants with posttransplant cyclophosphamide immunotherapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree