Research has solidified matched sibling marrow, cord blood, or mobilized peripheral blood as the best source for allogeneic hematopoietic stem cell transplantation for patients with sickle cell disease, with low graft rejection and graft-versus-host disease (GVHD) and high disease-free survival rates. Fully allelic matched unrelated donor is an option for transplant-eligible patients without HLA-matched sibling donors. Unrelated cord transplant studies reported high GVHD and low engraftment rates. Haploidentical transplants have less GVHD, but improvements are needed to increase the low engraftment rate. The decision to use unrelated cord blood units or haploidentical donors depends on institutional expertise.
Key points
- •
Progenitor cells (bone marrow, cord blood [CB], or peripheral blood stem cell) from matched sibling/related donors offer the best results of transplantation.
- •
Although there are insufficient data in sickle cell disease (SCD), fully matched unrelated marrow is likely the next best option. This donor source is rare for patients with SCD.
- •
No study directly compared fully with less well-matched unrelated CB transplants. The combined data showed 50% disease-free survival, 20% acute graft-versus-host disease (GVHD), and 15% mortality.
- •
The data from haploidentical (or mismatched related) transplants have 43% disease-free survival, 9% acute GVHD, and 9% mortality. The institutional expertise dictates whether haploidentical or unrelated CB is better suited; both should be performed in the context of clinical trials.
- •
Mismatched unrelated marrow (7/8 or less) in SCD is disappointing. This donor source should be studied only in the context of innovative clinical trials.
Introduction
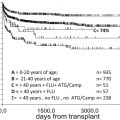
The first reported bone marrow (BM) transplant (BMT) for sickle cell disease (SCD) was published in 1984 in a child who had developed acute myeloid leukemia (AML). She was cured of both and remains alive almost 3 decades later. This proof-of-principle report paved the way for a series of pilot studies also showing that transplantation from HLA-matched sibling donors (MSD) could cure SCD. Later, the multicenter trial published by Walters and colleagues in 1996 was instrumental in validating transplant as a bona fide treatment. In this landmark trial, 22 children with very symptomatic SCD underwent MSD marrow transplantation; overall and disease-free survival (DFS) estimates at 4 years were 91% and 73%, respectively. Since then, the procedure has become safer and more effective. This success is shown by the 95% DFS in 44 patients undergoing refined transplant procedures after January, 2000, as described by the French group.
Traditionally, myeloablative conditioning was used in SCD transplants to maximize engraftment. Therefore, patients older than 16 years with significant sequelae of SCD, including considerable organ dysfunction, were often excluded. Less intense preparative regimens have made curative approaches available to adults. Increased rates of stable mixed chimerism are accepted as part of these less intense regimens, because the red cell compartment is replaced with normal donor red cells, and symptoms of SCD resolve with time. The largest report to date of such nonmyeloablative (NMA) transplantation was recently described, in which 30 adults safely underwent matched sibling transplant, with an 87% DFS.
Over the last 2 decades, there has been significant progress in transplantation using alternative sources such as umbilical cord blood (CB) units, haploidentical donors, and unrelated donors to make this curative procedure more accessible to those who are eligible.
Introduction
The first reported bone marrow (BM) transplant (BMT) for sickle cell disease (SCD) was published in 1984 in a child who had developed acute myeloid leukemia (AML). She was cured of both and remains alive almost 3 decades later. This proof-of-principle report paved the way for a series of pilot studies also showing that transplantation from HLA-matched sibling donors (MSD) could cure SCD. Later, the multicenter trial published by Walters and colleagues in 1996 was instrumental in validating transplant as a bona fide treatment. In this landmark trial, 22 children with very symptomatic SCD underwent MSD marrow transplantation; overall and disease-free survival (DFS) estimates at 4 years were 91% and 73%, respectively. Since then, the procedure has become safer and more effective. This success is shown by the 95% DFS in 44 patients undergoing refined transplant procedures after January, 2000, as described by the French group.
Traditionally, myeloablative conditioning was used in SCD transplants to maximize engraftment. Therefore, patients older than 16 years with significant sequelae of SCD, including considerable organ dysfunction, were often excluded. Less intense preparative regimens have made curative approaches available to adults. Increased rates of stable mixed chimerism are accepted as part of these less intense regimens, because the red cell compartment is replaced with normal donor red cells, and symptoms of SCD resolve with time. The largest report to date of such nonmyeloablative (NMA) transplantation was recently described, in which 30 adults safely underwent matched sibling transplant, with an 87% DFS.
Over the last 2 decades, there has been significant progress in transplantation using alternative sources such as umbilical cord blood (CB) units, haploidentical donors, and unrelated donors to make this curative procedure more accessible to those who are eligible.
Indications for transplantation
Indications for transplant are either directed to patients requiring lifelong transfusion because of an increased risk of recurrent or primary stroke (stroke and increased transcranial Doppler velocity), a significant impact on quality of life (recurrent vaso-occlusive crises, priapism, acute chest syndrome, osteonecrosis of multiple joints, and symptomatic silent infarct), difficulty maintaining transfusion therapy because of the lack compatible units (red cell alloimmunization), or an association with increased mortality (tricuspid regurgitant jet velocity line [TRV] >2.5 m/sec, sickle-related liver injury, iron overload, and sickle nephropathy). These indications are summarized in Table 1 .
| Established Indications | Potential Indications for Consideration |
|---|---|
|
|
Patient evaluation overview
SCD-related complications are important to identify before transplant. Not only do they drive the decision for transplant, but they also serve as a baseline for peritransplant and posttransplant care. Thus in addition to standard transplant-related blood (including renal/liver parameters and transfusion-related infectious pathogens), lung, and cardiac testing, evaluations for SCD-related end-organ injury should include the following:
- •
Brain MRI/MRA to establish the presence and extent of infarcts and vascular abnormalities
- •
Neurocognitive testing
- •
Echocardiographic estimate of pulmonary pressure (TRV)
- •
6-minute walk test
- •
Consider right heart catheterization for suspected pulmonary hypertension
- •
Quantitative iron assessment, including ferritin, liver biopsy (if possible) to assess the extent of inflammation, fibrosis, and quantitative iron, or cardiac or liver magnetic resonance imaging for T2* measurements
- •
Creatinine clearance estimation by nuclear glomerular filtration rate (typically in children)
- •
Twenty-four hour urine collection for creatinine clearance and protein for adults: because patients with SCD often have serum creatinine levels of 0.6 mg/dL or less, higher levels may indicate subtle or overt renal injury
- •
Red cell phenotyping of the recipients and donors; the transfusion medicine department should be given ample time to store blood for patients who require difficult to match packed red blood cell units; patients should be screened for donor-directed antibodies to minor red blood cell antigens, because of the risk of pure red cell aplasia after transplant, particularly in the NMA setting
- •
HLA-antibody testing of the recipients considering alternative donor transplantation; if donor-specific antibodies are detected, another donor may need to be identified because of the increased risk of graft rejection
HLA-matched hematopoietic stem cell transplantation
HLA-Matched Sibling Donor
Myeloablative
The first transplant for SCD used BM from a MSD for AML. The preparative regimen consisted of cyclophosphamide 120 mg/kg over 2 days and fractionated total body irradiation (TBI) of 11.5 Gy. Graft-versus-host disease (GVHD) prophylaxis was a short course of methotrexate (MTX) and 28 days of methylprednisolone. The patient was cured of both diseases. At about the same time, thalassemia major had been reported to be cured by MSD BMT, and myeloablation was achieved using the nonradiation-containing regimen of busulfan (Bu) and cyclophosphamide (Cy). In the late 1980s and early 1990s, a few case series of patients with SCD undergoing myeloablative BuCy MSD BMT were reported, prompted by the successful outcomes using this approach in patients with thalassemia. The multicenter study published by Walters and colleagues in 1996 showed that the myeloablative BuCy approach could reproducibly achieve good outcomes (73% DFS) in severe SCD. With better supportive care and in a larger cohort of patients, the addition of rabbit antithymocyte globulin (ATG) reduced the graft rejection rate from 23% (without ATG) to 3% (with ATG), as reported by Bernaudin and colleagues in 2007. Many studies have now published the MSD BuCy + ATG regimen, and overall survival and DFS ranges from 90% to 100% and 77% to 100%, respectively ( Table 2 ).
| References | Donor Source | Conditioning Regimen | HLA Match | Number of Patients (Age Range [y]) a | DFS (%) (Number of Patients) a | Acute GVHD (Grade 2–4) (%) a | Chronic GVHD (Extensive) (%) a | Number of Deaths (%) a |
|---|---|---|---|---|---|---|---|---|
| Matched sibling b | Myeloablative | 8/8 or 10/10 | 334 (1.2–27) | 87 (290) | 17 | 3 | 5 | |
| Matched sibling c | RTC and NMA | 8/8 or 10/10 | 65 (1.8–65) | 92 (60) | 5 | 0 | 2 | |
| Related cord | Mostly myeloablative | Mostly 6/6 | 89 (1.8–20) | 90 (80) | 8 | 0 | 9 | |
| Unrelated cord | RTC and myeloablative | Mostly 4/6 and 5/6 | 41 (1–22) | 49 (20) | 20 | 7 | 15 | |
| Haploidentical | Mixed | Haploidentical | 23 (4.2–42) | 43 (10) | 9 | 9 | 9 |
a DFS is an average of the total number of patients from all studies who were alive and without disease. The median follow-up time may be different across studies. Many references include patients with SCD and thalassemia, matched sibling and CB sources. Rates of GVHD and death were estimated, with the assumption that rates were the same for hemoglobin disorder type or graft source.
b Studies published after 2000.
A few important points of this standard approach should be highlighted. Intravenous Bu has largely replaced the oral route of administration to reduce the incidence of sinusoidal obstructive syndrome. Bu is usually given as a 0.8 mg/kg/dose for 16 doses over 4 days (or 3.2 mg/kg once daily dosing), targeting steady state concentrations of 600 to 700 ng/mL or area under the curve of 900 to 1100 μmol/min/L. Cy (50 mg/kg/dose) is given daily for 4 days. Equine ATG (30 mg/kg/dose for 3 days within the 4 days before transplant) or rabbit ATG (10–20 mg/kg divided over 4 days, typically days –6 to –3) is included. GVHD prophylaxis includes cyclosporine for 180 days after transplant and a short course of MTX. Central nervous system (CNS) protective measures include maintaining a platelet count greater than 50,000/uL, hemoglobin 9 to 11 g/dL, magnesium greater than 1.6 g/dL, aggressive antihypertensive management, and seizure prophylaxis while receiving Bu and calcineurin inhibition.
- •
Myeloablative transplants from MSD are mostly performed in children and young adults.
- •
Excellent DFS has been achieved through improvements in supportive care, conditioning regimen, and CNS protective measures in this standard transplant approach.
- •
Although the rates of graft rejection (5%) and mortality (5%) have reduced recently, further optimization to decrease the rate of GVHD can make this standard regimen even more successful.
HLA-Matched Sibling
Reduced toxicity and nonmyeloablative
Because outcomes have been excellent with the myeloablative approach, investigators have attempted to offer transplant to previously excluded adult patients with SCD by using reduced toxicity (RTC) or NMA conditioning. Part of the premise is that achieving complete donor chimerism is not necessary, because many patients have been reported to have SCD symptom resolution with a stable mixed chimeric state, an expected scenario with RTC and NMA regimens. In addition, patients undergoing transplant may benefit from less intense conditioning, potentially leading to decreased problems with fertility and other transplant-related organ dysfunction. However, earlier RTC and NMA experiences used transplant regimens from hematologic malignant transplants, and their results showed excessive GVHD leading to death in 1 series, and graft rejection in another. These initial discouraging results prompted redesign of the conditioning regimen in SCD.
One such regimen was tested in 30 adult patients undergoing MSD peripheral blood stem cell transplants, conditioned with alemtuzumab, low-dose TBI (300 cGy), and sirolimus. In this approach, alemtuzumab was chosen for in vivo T-cell depletion to prevent GVHD and rejection, TBI was increased to 300 cGy over the traditional 200 cGy to increase myelosuppression, and sirolimus was used for tolerance induction. Twenty-six of the 30 patients retained their graft, resulting in normalization of their hemoglobin level, and the approach was well tolerated without any GVHD. One patient died of intracranial hemorrhage after graft rejection. Although no patient achieved 100% donor chimerism in both T cells and myeloid cells, sirolimus was discontinued in 15 of 26 engrafted patients. Promising studies of HLA-matched RTC/NMA transplant for SCD are summarized in Table 2 . Alemtuzumab was commonly included in several recent studies, and may contribute to the almost absent GVHD, mortality, and rejection rates. High CD34 cell counts may help overcome the host versus graft barrier. The relatively small numbers and mixed chimeric state do warrant larger trials with extended follow-up. Longer follow-up would also allow exploration regarding whether RTC/NMA regimens are associated with less infertility and organ toxicity, compared with myeloablative transplants.
- •
Although the collective experience of RTC/NMA transplants is less robust than myeloablative transplants, their results have dramatically improved recently.
- •
RTC/NMA transplantation is gaining acceptance as a standard option for older adults or those with organ damage.
- •
As with MSD myeloablative transplants, T-cell depletion is an essential component of the RTC/NMA conditioning regimen.
Related Umbilical Cord Blood Transplantation
The largest CB transplant (CBT) study was reported by the Eurocord and European Blood and Marrow Transplantation group in 2013. Of 160 patients with SCD who underwent HLA-identical CBT or BMT, 30 received CBT. The 6-year DFS was 90% after CBT and 92% after BMT. Of all patients transplanted, those who received a CBT had significantly longer time to neutrophil and platelet engraftment compared with those who underwent BMT ( P <.005). However, no patients who received CBT developed grade IV acute GVHD compared with 8 (2%) who received BM cells, and none of the CBT recipients experienced chronic extensive GVHD compared with 5% of the patients who received BMT.
Studies have shown that MTX affected outcome in patients with SCD and thalassemia major who undergo related CBT. Patients who did not versus patients who did receive MTX had DFS of 90% versus 60%, respectively ( P <.001). Patients who received thiotepa also did better, although thiotepa did not influence outcome in multivariate analysis. The total nucleated cell (TNC) dose infused did not affect outcome in patients who received CBT, although median TNC count was adequate at 3.9 × 10 7 cells/kg.
Recent studies have reported a more robust neutrophil (17 vs 25 days, P = .013) and platelet (29 vs 48 days, P = .009) recovery in patients who received CB along with BM compared with CB alone. All 13 patients who received CB coinfused with BM remained engrafted, with a median follow-up greater than 5 years, with no acute grade 2 or greater GVHD or chronic GVHD. A second study showed long-term engraftment in all patients who received hydroxyurea before Bu, Cy, and ATG. Therefore, CB and BM coinfusion as well as hydroxyurea treatment before conditioning seem to be viable options to explore further in young patients with HLA-MSD.
- •
Related CBT with mostly 6/6 matched units resulted in similar overall survival and DFS but lower incidence of chronic GVHD, compared with HLA-MSD BMT (see Table 2 ).
- •
Specific pretransplant and peritransplant treatment used (eg, hydroxyurea or MTX) affects CBT outcome.
- •
Coinfusion of CB and BM may shorten duration of BM recovery and improve CBT outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree