Fig. 1.1
Hematopoietic system cancers: incidence and mortality in the aged 70 years and more vs. the less than 70 years ones by site and gender (proportion per 100). HL Hodgkin’s Lymphoma, MM Multiple Myeloma, NHL Non – Hodgkin Lymphomas, HEMO Hematological Tumours
The percentages of haematopoietic tumours increased strikingly in the elderly moving to mortality: 42 % of deaths occurred in younger men, 58 % in elderly men, while 33 % in younger women and even 67 % in elderly ones. In older men the single entities accounted for 25, 20, 12 and 1 % in leukaemia, NHL, MM and HL respectively, while in women the same values were 26, 25, 15 and 1 % [1].
Aetiology
Development of Hematological Tumours Is Favoured by Aging Process
Aetiology of hematological tumours is up to now largely unknown. Several risk factors have been found in epidemiological studies and some associations have been identified and assessed, even if the etiologic factors do not account for a great number of incident cases. Moreover, it must be remind to distinguish the natural history of hematological tumours occurring during childhood, adulthood, especially in the elderly. At this regard it is important to consider the latency time between the exposure to carcinogen, or more generally to the risk, and the cancer development. In any case, for most cases of hematological tumours it is impossible to find a precise genetic or environmental cause. In fact, several genetic disorders or environmental situations have been identified as risk factors, but they constitute only a small proportion of all hematological cases in the elderly [2, 3].
Leukaemia and lymphomas, like other cancers, start to grow up owing to the combination of environmental risk factors acting along with genetic susceptibilities. The most general mechanism which lead to the development of hematopoietic tumours is the lack of the equilibrium between the renewal and death of blood cells. During the lifespan, after the early development of hematological system, a balance between the renewal and death of blood cells begins. However, even if bone marrow is the tissue with the highest frequency of proliferation of stem cells, as other tissues, it must undergo ageing and its negative effects.
The balance between cell progenitors and differentiated elements has the tendency to go off during aging, because, B lymphocytes in particular decrease their production [4, 5]. It is probably that the mechanism of senescence lead to a decline in B cell production, as a phenomenon already fixed in blood cells progenitors. In addition, hematopoietic cells begin to age and lose their physiological functions, with the alterations of the expression of some genes devoted to check the healthy status of DNA. Summarising, bone marrow and hematological system lose their capability to check for homeostasis and to repair DNA damages owing to ageing [6]. The impairment of progenitors involves principally the lymphoid compartment and, to a lesser extent, the proliferation of the myeloid cell line.
In addition to the lost ability of cells to differentiate, some authors have found that also the environment of bone marrow, where the progenitors develop, changes its physiological conditions. Owing to the close relationship between haematic cells and the support tissue where they proliferate and differentiate, the physiological status is completely dependent by the stromal elements of bone marrow. All these hematological shortcomings lead to a decline in adaptive immunity and are strongly related with the individual’s age [7–9].
Immunosuppression
Both quantitative (the decrease of differentiated lymphocytes) and qualitative (compromised quality of stromal functions) defects cause a decline of all immune system [10, 11]. Such immunosuppression has been confirmed by some analyses which have studied in wide cohort of patients the correlation between immunodeficiency (congenital or acquired) and the probability to develop hematological cancers. At this proposal, is of particular interest a study which has shown that about 25 % of patients suffering from congenital immunodeficiency will develop cancers, particularly non Hodgkin lymphoma (50 % of the tumours in excess) [12]. Furthermore, in literature it is well known that transplants, through immunosuppression, cause especially hematological tumours of myeloid cells such as acute myeloid leukaemia (AML) [13].
These marked alterations, principally affecting the lymphocytic line, influence both the development of lymphomas and leukaemia in elderly patients. More precisely, the main occurrence of hematological malignancies is made up by lymphatic cells in childhood and myeloid cells in adulthood, especially in old people. Another evidence is provided by a Dutch population-based study. It is an innovative investigation based on the relationships between autoimmune disorders and lymphoproliferative tumours. The authors found that the prevalence of autoimmune and chronic inflammation was significantly associated with newly diagnosed lymphoproliferative malignancies. In particular, the positive correlation with some lymphoma subtypes was striking [14].
Viral Infections
The aforementioned analysis showed as, in addition to the immune system impairment, related to aging, also the infections directly could be considered an important risk factor for hematological tumours, particularly in the elderly. De va schans determined that infective agents can cause mainly lymphomas through three action mechanisms. First, virus interacts directly with lymphocytes, as for Epstein-Barr virus. Second, other viruses, such as HIV, give rise to an acquired immunosuppression syndrome [14]. It is well known that the NHL is closely linked to HIV positive infection and now is decreasing in incidence also thanks to the introduction in the mid-1990s of antiretroviral therapy. A third mechanism concerns some viruses and autoimmune diseases, like rheumatoid arthritis: the lymphomas could be caused by a chronic immune stimulation which leads to a too much intense and deregulated cell lymphatic proliferation [15].
The viral hypothesis was confirmed by a meta-analysis dealing with NHL and HCV-positive persons that found a pooled relative risk very high (around 2.0–2.5) [16]. As regards HBV, a recent study performed in South Korea showed that there was an association between chronic hepatitis B virus infection and higher risk of developing NHL: HBsAg-positive subjects developed easier NHL than general population [17]. It is difficult to assess the existence of an association between HCV and HBV and other hematological tumours, due to the small number of cases enrolled in the studies, however, weaker associations were found also with Hodgkin’s lymphoma (HL) and multiple myeloma (MM) [16].
The EBV is a viral risk factor that produces tumours principally in two ways. In a first case EBV acts as a cofactor together with immunosuppression (HIV infection, transplants). Second, EBV is present in the total cases of Burkitt’s lymphomas and, outside the endemic areas, it is detected in some sporadic lymphomas [18].
Focusing the attention on the single types of leukaemia, it is difficult to individuate specific viral agents able to influence the incidence of such tumours. Nevertheless, it would seem that could exist an association between AML and parvovirus B19 [19]. Another virus affecting the haematic system is an endemic retrovirus (HTLV type-1, type-2) spread in Japan, Caribbean and South-Eastern US, which causes some rare forms of hematological malignancies, such as T-cell leukaemia/lymphoma [20]. The low incidence and the long latency period suggest the participation of a multistep pattern with multiple genetic mutations to observe the onset of the disease, which occurs more frequently in adults and elderly people [21].
Overweight and Obesity
The prevalence of an elevated BMI, higher than the values of World Health Organisation (> = 30.0 kg/m2), of overweight (BMI = 25–29.9 kg/m2) and obesity is dramatically increasing and it has been estimated that more than 1.6 thousand million people are overweight. Obviously there are striking differences among the different areas of the world, but also in Africa and Asia the obesity has increased. It must to be taken in mind that the relatively long latency period observed between the onset of obesity and a subsequent increase in cancer incidence, can explain the incidence in adult patients, particularly elderly of hematological malignancies.
As seen above, such tumours are associated to autoimmune and chronic inflammatory diseases. On the other hand, obesity alters the immune system and is related to chronic inflammatory conditions, having the capacity to constitute a risk factor especially for HL and NHL. In adulthood, and particularly in the elderly, the effect of obesity can be divided into two categories: the result of a greater mass of fat which directly affects the organ functioning and the result of an expansion of endocrine compartment, owing to the enlarged number of fat cells and the effect on target tissues. The increase of several hormones related to adiposity accounts for the cancer development [22].
A recent meta-analysis found that a 5 kg/m2 increment in BMI was associated with a 7 % increased risk of NHL. Only few studies were performed on HL and have observed that obesity was statistically correlated with HL, especially the risk tended to be higher in the older rather than younger patients [23, 24]. A higher number of studies has observed a close association between the excess of body weight and development of MM. A very large prospective study, developed in US on 900,000 adults, has found that for lymphomas, leukaemia and MM the mortality relative risk (RR) was significantly higher and increased with aging [25].
Large cohort studies have assessed that obesity influences incidence and mortality of hematological cancers [26, 27]. However, the most investigations have not analysed the risk for each type of leukaemia or subtypes of lymphomas, presumably because of the relative small number of available cases. Notwithstanding, a meta-analysis has been carried out investigating, through cohort studies, the relationships between the excess of BMI and the incidence of leukaemia as a whole and each major subtypes [28]. They have found higher RRs for overweight in all four types of leukaemia. As regards lymphoma subtypes, the diffuse large B-cell lymphoma showed a stronger correlation, more frequent in the elderly [27].
Ionising Radiation
The close correlation between exposure to ionising radiation and the development of haematopoietic tumours has been largely assessed. Unfortunately, the atomic bomb and the nuclear weapon tests have provided enough evidence, substituting experimental essays. The radiations, after a latency of 5–7 years, cause the developing of acute leukaemia and CML. The response to the risk factor is different according to the specific cellular type and the linkage with CCL is weaker [21]. In addition to the tragic experience of war survivors, scientific evidence has been provided by those authors investigating the role played by the exposure to low dose radiation for people working or living near nuclear power stations [29]. Therefore, the leukaemia as a whole are the type of tumour most frequently induced by ionising radiation. On the contrary, lymphomas are very rarely associated to this kind of exposure and the risk is practically similar to that of general population [21].
Chemicals Compounds
A higher risk of leukaemia has been identified for occupational exposure to benzene, formaldehyde and dioxins. Also organic solvents, agriculture pesticides have been associated to an increased risk. Benzene deserves a particular attention because it is a chemical among the most studied in the last century, with a clear evidence of a negative effect of acute and chronic exposure on blood system both in animal and humans. In particular, chronic and heavy exposures are a powerful risk factor especially for acute myeloid leukaemia. Other tumours and different workplaces have been investigated, but the results have not been supported by evocal epidemiological studies. Some authors have suggested that a chronic exposure to high level of airborne benzene may cause a risk excess for lymphomas, multiple myeloma and other haematopoietic malignancies [30].
Numerous epidemiological analyses have confirmed the association of lymphomas with different chemicals such as herbicides, insecticides and fertilisers compounds. Farmers are an occupational category very exposed because agriculture chemicals could be all potentially carcinogenic and lead to a chronic immunological stimulation [31]. Some studies have demonstrated very high risks of NHL for a frequent usage of herbicides, highlighting a correlation between exposure time and lymphomas risk. However, some authors have hypothesise that the striking increase of incidence occurred in the last two decades could be due to the widespread use of herbicides, in particular 2, 4-dichlorophenoxyacetic acid [32, 33].
Finally, it is important to mention the role played by anti-tumour treatment in co-operation to the development of haematic cancers. There is the possibility that some chemotherapeutic regimens and radiotherapy can induce AML. A second AML is more frequently associated to treatment for HL and MM,
In all with a latency of 5–10 years, accounting for 10–20 % of all the leukaemia of this type [34].
Ultraviolet Radiations (UVR) and Sun Exposure
A possible association between UVR and growth of incidence of lymphomas has been carefully studied. In 1990s some analyses found a risk increase of NHL correlated with the intensity of UVR [35]. The radiations would have an immunosuppressive effect and thus they would be able to favour cancerogenesis of lymphatic system. Nevertheless, several authors have not confirmed completely this hypothesis and have found no or only a weak correlation [21, 36, 37]. A more recent study of 2004 has reported that sun exposure was linked to a decreased risk of NHL, confirming the lack of any association with UVR [38].
Socio-Economic Status (SES)
Cancer is a chronic disease whose occurrence is closely related to SES. It is possible to assess that it is a real “social disease” and that the elderly are the individuals most affected by a poor SES [39, 40]. NHL is not an exception and some studies have found that mortality and survival are correlated to the deprivation level of patients. A Danish population-based study observed that mortality was 40 % higher in patients suffering from NHL with a lower attained educational level. In addition, mortality grows in unemployed individuals, with low income and singles. This prognostic disadvantage could be due to difficulties of access to health care, with a consequent more advanced disease stage at diagnosis [41].
A recent study has found that also AML is correlated with SES. Particularly, in UK mortality was nearly 50 % higher for the most deprived group. Moreover, a gradient was observed for HD, differing in accordance of the patient’s age. A protective social environment (in young adults) or an overcrowded social context (in children and in the elderly) was related to an excess of risk. The study did not found any linear association for leukaemia [42]. The same authors in a very large population-based study have found that the most deprived individual were less likely to undergo bone marrow transplant even after adjusting for confounding factors. These results are in accordance with a further investigation demonstrating an association between low survival and blue-collar workers both in AML and MM [43].
Descriptive Epidemiology
Age Distribution
Figure 1.2 displays age curves by sex of incidence and mortality for each hematological tumour site in more developed regions. For NHL the age curve showed an increase quite stable both in incidence and mortality up to older individuals. Rates of women were lower than those of men. Rates in both sexes did not exceed 9 cases per 100,000 and 2 per 100,000 until 40 years of age, for incidence and mortality respectively. Afterwards at 75 years incidence reached 83 cases per 100,000 in men and 56 in women, while mortality 50 in men and 33 in women. The initial gap between mortality and incidence decreased progressively with age and after 70 years the two indexes were very similar. Out of total NHL new cases, those occurring over 70 years were 42 and 51 % in men and women respectively, while deaths achieved 58 and 69 %. Practically more than half of newly diagnosed tumours and more than 2/3 of deaths were diagnosed in elderly women [1, 44].
Fig. 1.2
Haematopoietic system cancers: age curves of incidence and mortality in the more developed countries by site and gender (rates per 100,000)
Leukaemia showed incidence curves different from others considered haematopoietic neoplasm. In fact, there was a first incidence peak within the first year of age (5 and 4 incident cases per 100,000 in men and women respectively), followed by a successive decline up to 15 years old adolescents; finally incidence rates started to increase very quickly reaching a second peak at 75 and more years (77 and 41 cases per 100,000 in men and women respectively). As for mortality, the curve did not have the early decline, but the rates began to increase since birth in both sexes. Mortality grew up at a quicker pace than incidence and, over 75 years, the beginning gap between incidence and mortality disappeared (65 and 35 deaths per 100,000 in men and women respectively). Out of the total leukaemia, in the elderly the percentages of new cases (45 and 50 % in men and women respectively) and deaths (58 and 64 %) were very high and similar to those of NHL.
These curves were in accordance with a tumour hitting in paediatric age. For example, acute lymphoid leukaemia (ALL) is a subtype typical of children, not frequent in adulthood. Nevertheless most cases of leukaemia occurred in middle aged adults and in elderly. In particular, AML presents a median age at diagnosis of 64 years and therefore is mainly an adults’ disease. Also CML arises seldom in children or adolescents, while many cases occur in older people. In a similar way, CLL is a disease of the elderly, with a median age of 70 years. For this reason it is the more common leukaemia subtype in more developed countries.
Among hematological malignancies MM was the tumour decidedly most characteristic of older age, with a median age of onset of about 65–70 years. Until 40 years incidence and mortality remained lower than 2 cases per 100,000, afterwards new cases grew exponentially, reaching values of 39 (in men) and 24 (in women) cases per 100,000 in the aged 75 or more years. Also mortality rates increased strikingly and reached 31 and 20 deaths. The new cases of MM occurring over 70 years were 52 and 58 % in men and women respectively, while deaths reached the highest values of 64 and 71 %, confirming that this is the cancer more common in the elderly among all hematological types.
HL is not a tumour of old age. It presents two peaks in childhood and adulthood, primarily hitting young adults usually between 25 and 30 years and then older adults after 50. The age curve in Figure 1.2a shows in fact a first increase of incidence and mortality rates in both sexes in children, reaching a peak at 15 years. Then rates almost levelled off and increased, only slightly, with a successive peak over 75 years. The rates were a little bit higher in men than women. Only 13 % in men and 15 % in women of newly cases was diagnosed in elderly over 70 years, while 31 % and 41 % of deaths occurred in the elderly, confirming that this tumour affects prevalently young people.
Apart HL, these data confirmed that hematological tumours constituted a very high burden and, due to the ageing of population, they will be a major challenge which health systems must to cope with.
Geographic Distribution
Each broad hematological entity comprehends subtypes with different genetic profiles and immunophenotype. Each subtype has different histopathology, clinical procedures and epidemiological picture. These patterns correspond to different epidemiological profile which have a particular distribution across countries. Moreover, the distribution by area is partly caused by various etiological factors according to their prevalence in a specific geographical region. Notwithstanding, owing to the not clear knowledge of aetiology, it is difficult to explain exhaustively the different distribution according to the spread of determined risk factors confounded also by the huge differences in socio-economic status of people resident in the different macro-areas.
Substantial variations in incidence and mortality across the world have been observed, like shown in Figure 1.3 and Tables 1.1, 1.2, 1.3, 1.4, 1.5, 1.6, 1.7 and 1.8. Figure 1.3 shows how the macro-regions have been defined (according to sub-continental areas assessed by WHO) and on the right side of the figure the macro-regions differently coloured on the basis of the considered continent. In Tables 1.7 and 1.8 the incidence and mortality age standardised rates (ASR, world standard per 100,000), the crude rates and the yearly numbers of cancers estimated in 2008, by sex and two age groups (0–69 and 70 or more years) are listed [1].
Fig. 1.3
WORLD MACROAREAS. Source: American Cancer Society – Global Cancer Facts & Figures 2007
As regards developing countries, the rates were low, but the data from Asia and Africa in particular, have to be taken with caution owing to the low percentage of population observed by cancer registries, which must afford a hard challenge to provide complete and reliable data.
Considering all hematological tumours, and comparing the incidence and mortality rates in developing and developed countries, it is possible to individuate two specific patterns; in contrast to incidence which was always higher in Europe, Australia and Northern America both in younger and older age groups and in both sexes, mortality under 70 years had a less clear worldwide distribution, with developing countries showing often the highest rates. Only in the elderly, the developed countries showed the highest mortality values.
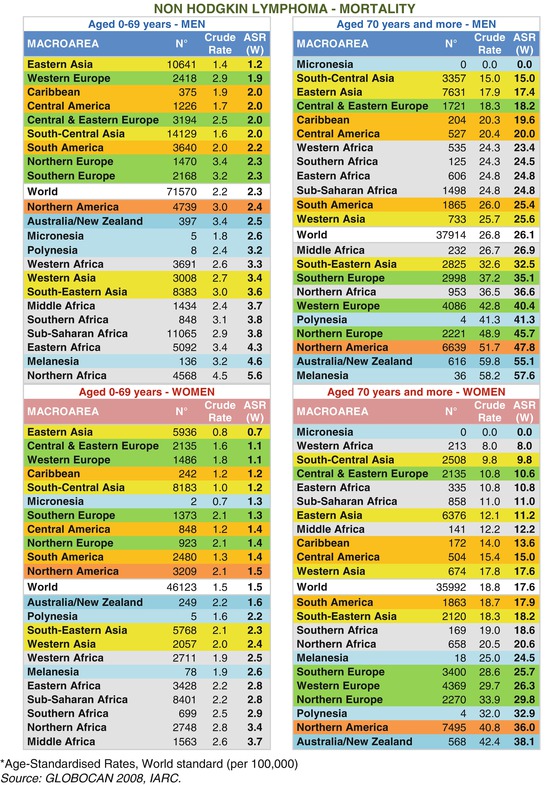
Non Hodgkin’s Lymphomas
For NHL all more developed countries have higher incidence rates than developing ones (Table 1.1): in men aged from 0 to 69 years, the values of men ranged from 2.5 in Eastern Asia to 11.9 in Northern America and those of women from 1.6 in Eastern Asia to 8.3 in Northern America. In the elderly the rank of considered countries did not change but rates strikingly higher with respect younger patients were recorded; in men rates ranged from 16.3 in South-Central Asia to 119.5 in Northern America and in women from 8.9 in Western Africa to 88.1. A very huge gap was observed between older and younger age groups: in more developed countries the elderly showed rates 10 times higher than in younger people, both in women and men.

Table 1.1
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)

For mortality the rank of countries was less definite than for incidence (Table 1.2). In younger age groups both in men and women the lowest rates (under the mean of the world) were registered not only in developing countries but also in some developed areas. Not surprisingly the highest values were observed in African macro-areas, probably due to a more diffuse exposure to infectious agent risks. A different situation was reported in the elderly, with higher mortality rates registered in more developed macro-areas, exception made for Central-Eastern Europe, while those lower in countries of the third world. This model was very similar to that observed for incidence, and a very wide difference between the elderly and younger people was observed also for mortality (rates were about 10 times higher in older compared to younger age group, in both sexes). Intriguing was the exception of Melanesia and Polynesia which followed the Australian rates and the very low rates of Central and Eastern Europe occurring for incidence and mortality in both sexes.
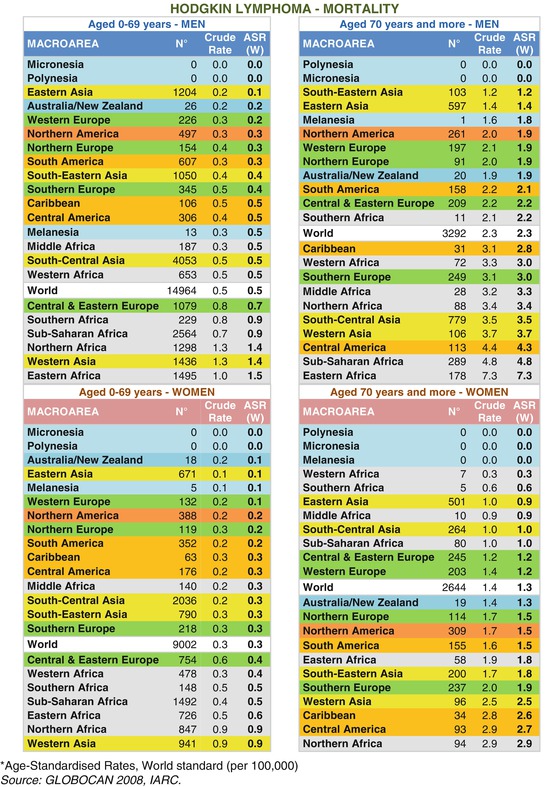
Table 1.2
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)
Among more developed countries, US had the tendency to show always rates higher than those reported in European areas. In these countries and in North America the most frequent histological types are nodal and follicular disease which account for 30 % of NHL in US and 20 % in Europe; such types are rare in developing world [45, 46]. Asiatic countries more frequently show intermediate-grade, high-grade diffuse aggressive [47] or peripheral T-cell NHL, extranodal disease, strongly associated with EBV and human T-cell leukaemia/lymphoma virus type 1 (HTLV-1) infection [48], whereas follicular lymphomas are rare. In Africa an excess of high-grade NHL has been observed, while the follicular subtype is rare. Burkitt’s lymphoma is very common, accounting for 25–44 % of all NHL [49] and occurring more frequently in children with a peak around seven years and involving more rarely older individuals.
Leukaemia
Like for NHL, also leukaemia incidence showed a clear pattern, similar in younger and older age groups (Table 1.3). Both in young and elderly people, all developed countries had the highest rates, followed by Central America, Asian countries and lastly Africans. The mortality pattern was partially different (Table 1.4). For the young group in both sexes Asian macro-areas had the highest rates followed by Central America, Europe and Northern America and Africa ones. Considering elderly patients the pattern was again similar to that of incidence with all developed countries showing the highest rates followed by Central America, Asia and Africa. The differences between the two age groups were striking, and in the developed countries the elderly had rates 15 and 10 times higher than younger people in men and women respectively. It is interesting to underline that many of the single countries at higher incidence (data not shown) often are those were in the recent past the inhabitants could be exposed to radiations (depleted uranium bullets) or chemical agents (defoliants as the orange agent) during the conflicts that bathed in blood these for many years.
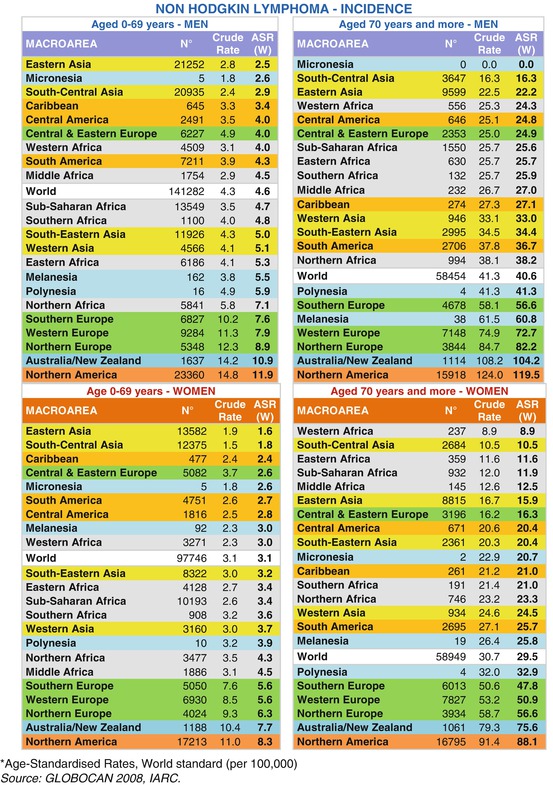
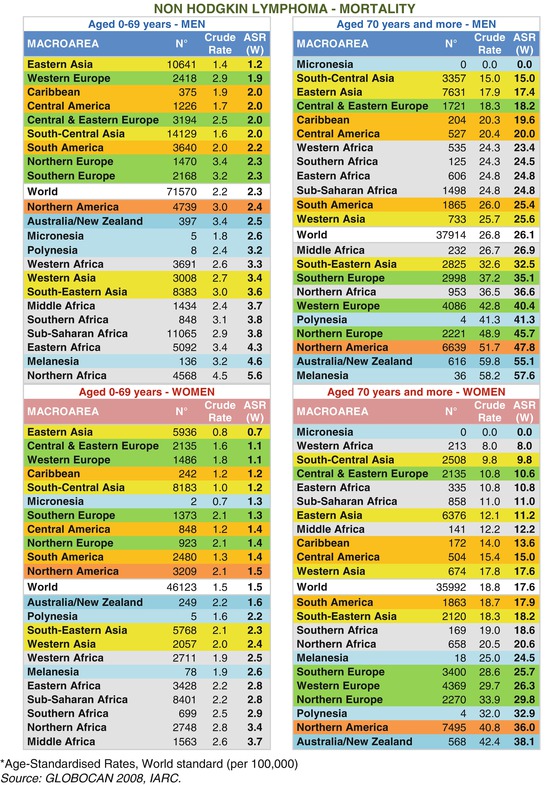
Table 1.3
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)
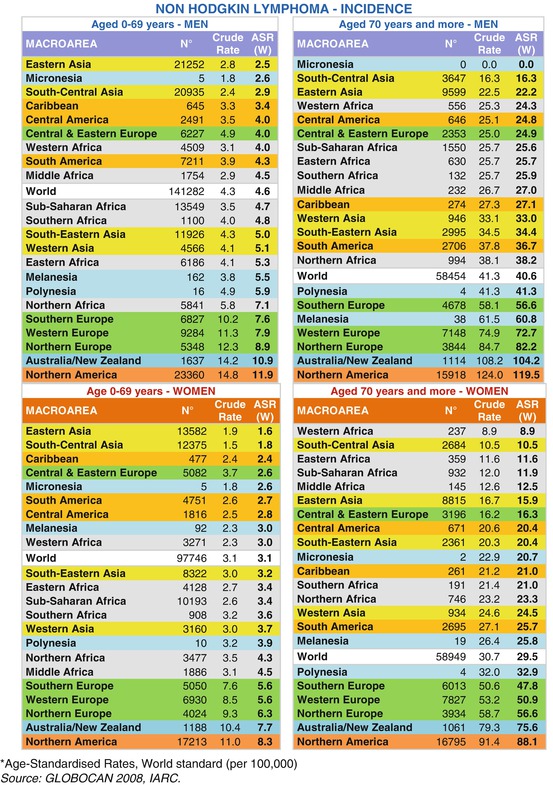
Table 1.4
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)
Multiple Myeloma
The country rank, reported for incidence of NHL and leukaemia, still recurred for MM (Table 1.5). In fact, both in the two age groups and in both sexes the highest rates were observed for developed countries followed by Central and South America and African macro-regions. Central and Eastern Europe represented, as already seen above, an exception within the European continent, showing much lower rates, almost at level of developing countries.
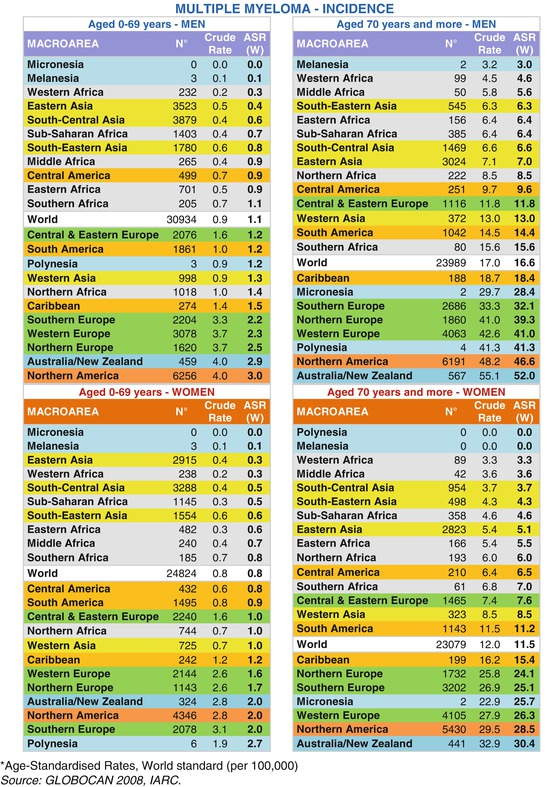
Table 1.5
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)
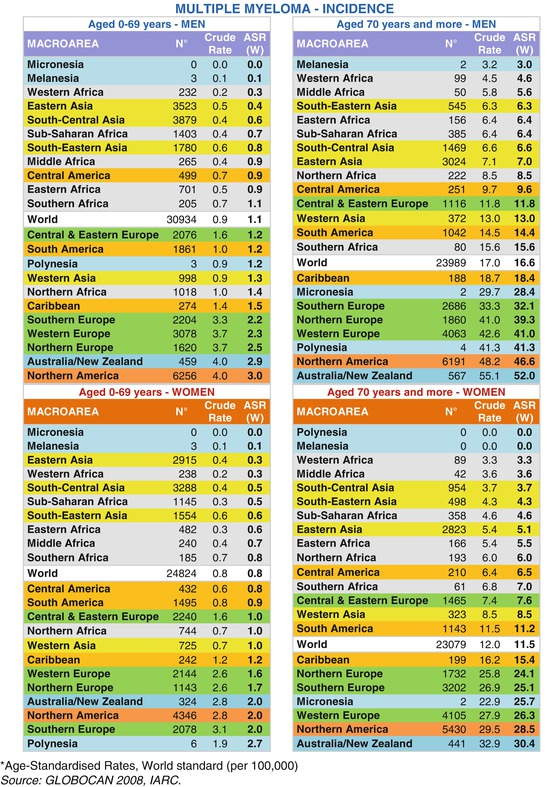
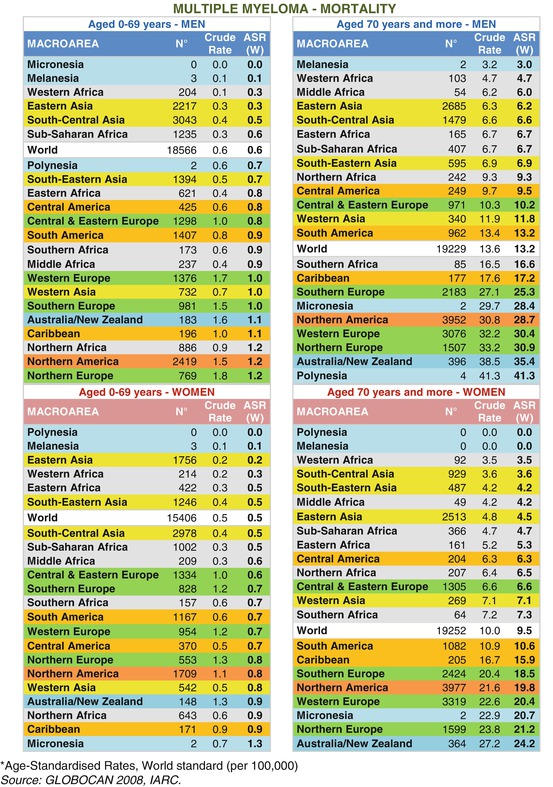
The pattern observed for leukaemia mortality recurred also for MM (Table 1.6). For the young group the highest rates were registered not only in the developed countries, but also in some unexpected developing regions of Africa, Central America and Asia. With respect to the elderly, the distribution returned to be “classic”, with more affluent countries having the highest rates, followed by macro-regions with decreasing affluence. The exception of the low rates in Central and Eastern Europe still remained as well as the bizarre behaviour of insular areas of Oceania. The differences in incidence rates by age group were highest in affluent areas with rates 17 and 11 times higher in the elderly than in younger people, for men and women respectively. For mortality the same ratios increased to 34 and 19.
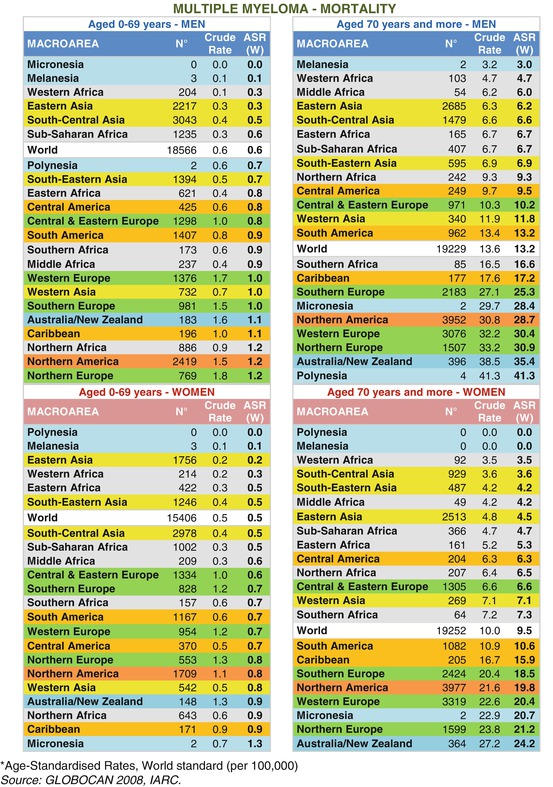
Table 1.6
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)
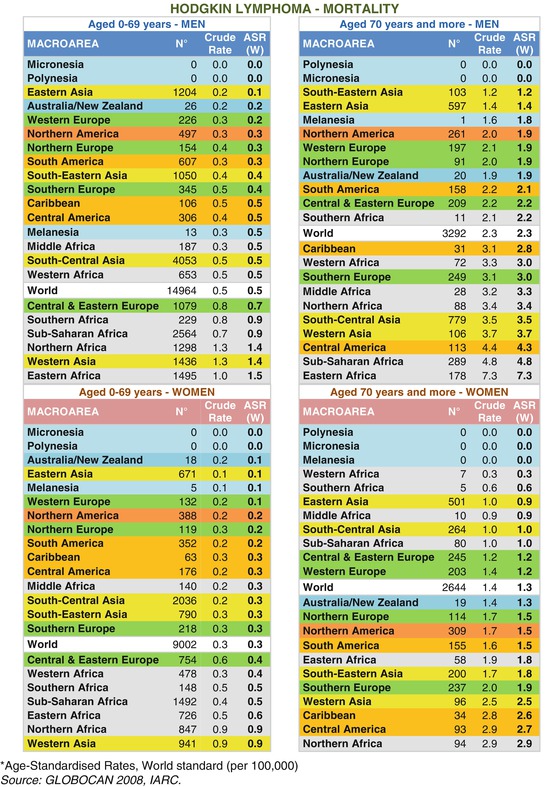
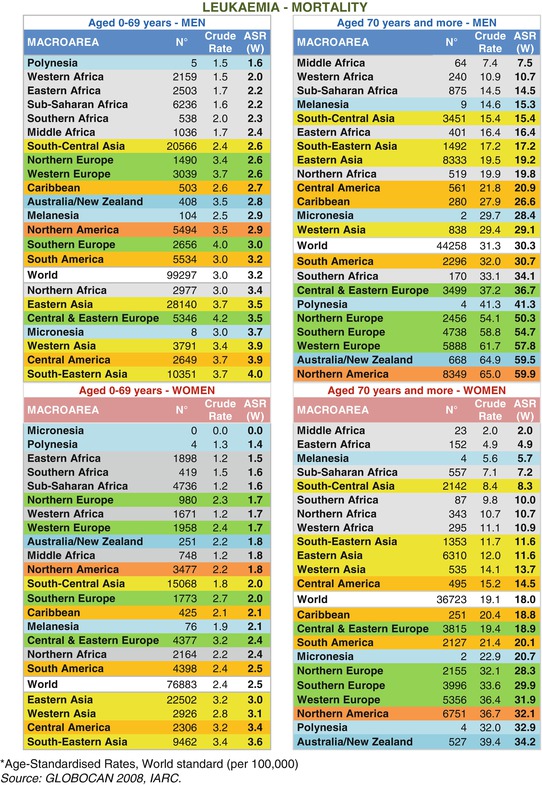
Hodgkin’s Lymphoma
This hematological malignancy is typical of children and adolescents, representing in the elderly only a very small part of all combined cancers. The incidence rates for both sexes did not overcome 2.6 in the young group and 6.1 in the elderly, while mortality rates did not exceed 1.5 in younger people and 7.3 in the elderly (Table 1.7). In the younger group incidence pattern showed the “classic”, already observed, gradient: developed countries had the highest rates followed, as usual, by the poorer populations, in both sexes and age groups. Less definite was the rank for the elderly with some African areas having rates among the highest in the world. The older individuals of Northern America and Southern Europe had rates around 2 times higher than the younger ones and in women this ratio was even lower, demonstrating that this tumour is prevalently a paediatric tumour.
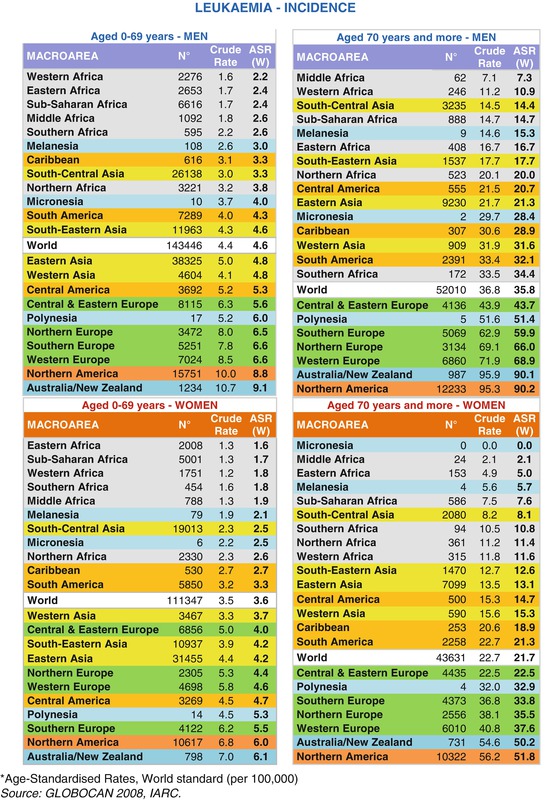
Table 1.7
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)
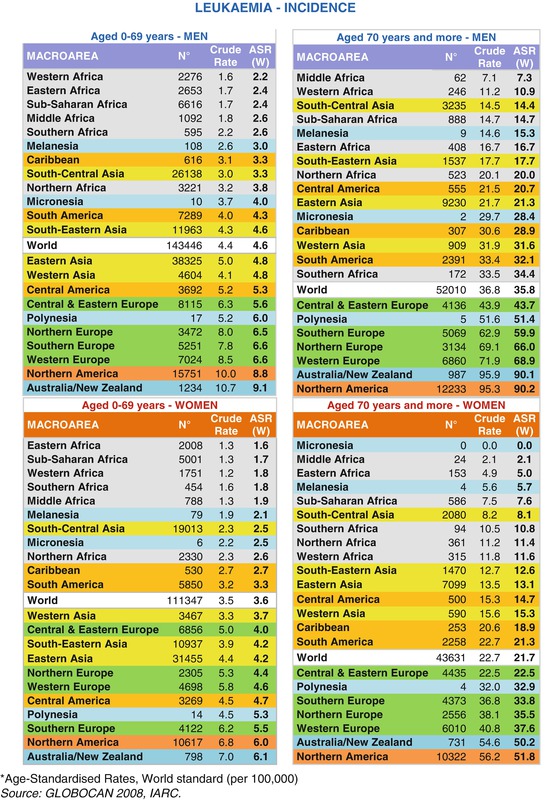
This gradient was completely inverted for mortality (Table 1.8). The highest rates were observed for African and Asian areas, followed by Central and South America and, finally, by the affluent Western macro-areas. However, the rates were so low that any comment is probably unreliable and it must be taken with caution.
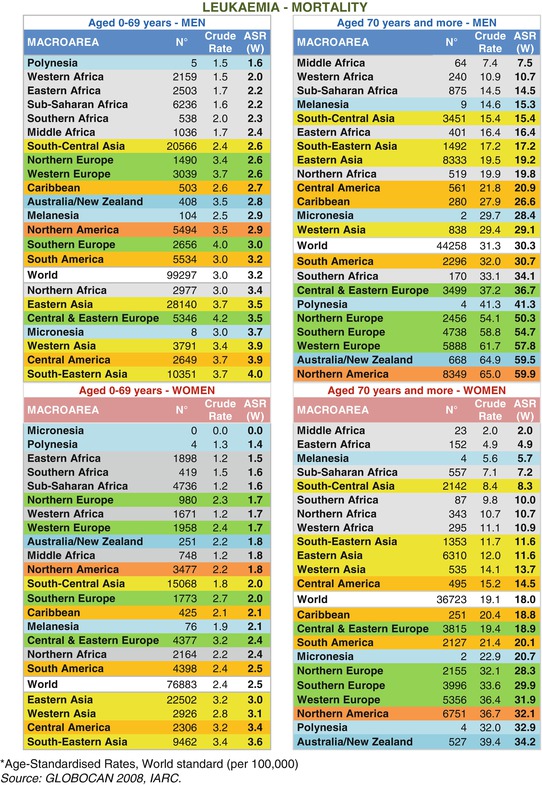
Table 1.8
Incidence and mortality by world macro-areas, site and gender. Numbers, crude rates and ASR(W)
Time Trends
Figure 1.7 for men and Fig. 1.8 for women give incidence and mortality time trends (age standardised rates according to world standard population) from 1988 to 2008 for NHL, leukaemia and MM, comparing middle aged adults (55–69 years) with the elderly aged 70 or more years. The HL trends are not reported due to the low numbers and their instability in time.
We choose three examples of developed countries, having a high occurrence of hematological malignancies, such as Italy and UK for Southern and Northern Europe as well as US.
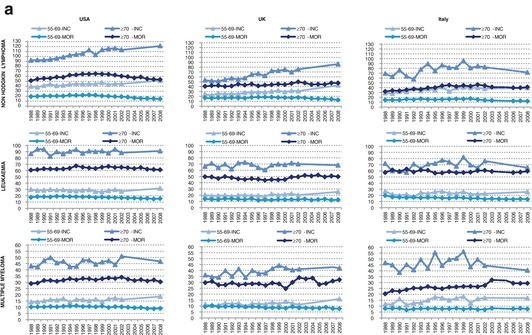
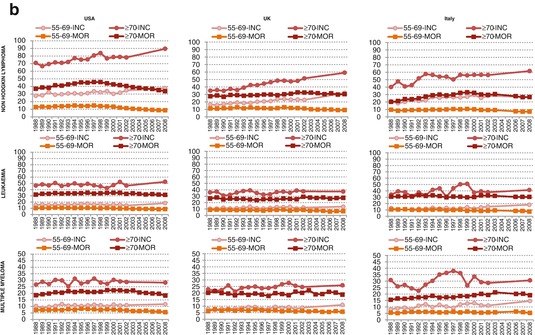
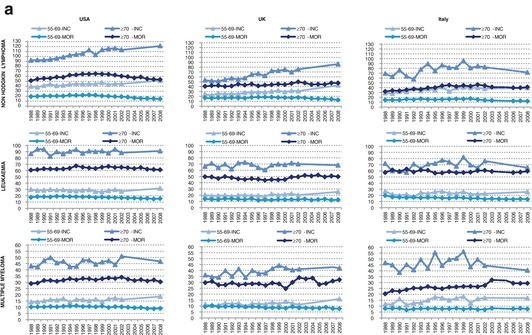
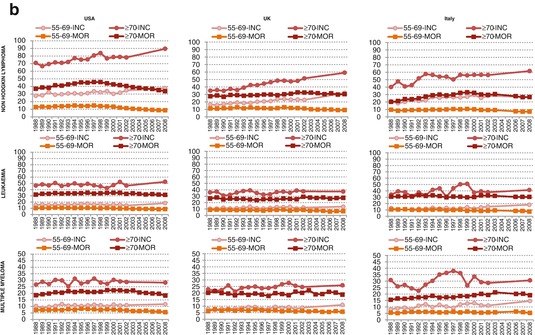
Fig. 1.4
(a) Incidence and mortality trend of Non-Hodgkin Lymphomas, Multiple Myeloma and Leukemia in USA, UK (England & Wales) and Italy. MEN – Aged ≥70 years vs. the 55–69 ones (ASR-W). (b) Incidence and mortality trend of Non-Hodgkin Lymphomas, Multiple Myeloma and Leukemia in USA, UK (England & Wales) and Italy. WOMEN – Aged ≥70 years vs. the 55–69 ones (ASR-W)
Incidence rates from 1988 to 2002 came from the IARC publication of Cancer Incidence in five Continents, therefore directly observed by cancer registries (9 for US, 5 for UK and 6 for Italy) [44], while the expected rates of 2008 were drawn from the database of Globocan estimates [1], that came from modelling procedures, and data for the 2003–2007 intermediate period were interpolated. For this reason the more recent estimated part of trend should be interpreted cautiously.
Death certification data derived by WHO databank [50]. Italian mortality data for 2004 and 2005 not produced by ISTAT (the Italian national institute of statistics) were interpolated [51].
Incidence and mortality trends were analysed by means of Join point regression models, using the Joinpoint Regression Program in order to obtain the Annual Percent Changes (APCs) and the Joinpoints years (JPs). The time-trend is divided into segments and the number of segments depends on the number of JPs. The JP year is the point in time when we estimate a variation in time trend [52].
Non Hodgkin’s Lymphomas
NHL incidence rates increased in all the three countries, both sexes and age groups. The largest variations were observed for UK, where all the rates grew about 3 % yearly, with younger people showing a faster pace since 2003–2004. Over the whole period in the elderly rates increased from 53 to 86 new cases per 100,000 in men and from 35 to 59 in women. The rise was marked also in US with a significant upward trend in younger individuals of both sexes (APC around 1.1–1.4), while in the elderly women showed an increase from 71 to 89 new cases and in men, after a quick rise, a levelling from 2000 (rates from 92 to 121 over the whole period). In Italy the picture was a little better. In middle aged adults of both sexes an early growth until 1994 was observed, followed by a levelling leading to an overall rise of 1.4 and 1.7 % in men and women respectively. In elderly men the rates increased quickly until 2000 thereafter decreased from 81 to 72, in women increased from 40 to 62 during the entire period.
Summarising, the epidemic growth of NHL observed during the second half of twentieth century was not finished in 2008, especially in UK and US. However, we found an encouraging levelling or a slight decline from the early 2000s in Italian elderly of both sexes and in older American men.
As regards mortality, trends were more favourable. Downward trends were noted in the three countries for almost every age or sex. After a strike increase until the end of 1990s a reversal of trend was reported, particularly in Italy and US; in contrast, in UK the rates of the elderly still increased. In younger Italian people of both sexes mortality fell since 1999 (APC about −4 %), while the corresponding value of older patients were slightly lower (about −1.5 %). A similar picture appeared in US where the APCs were equal to those reported in Italy. The rates declined since 1998 from 65 to 54 and since 1997 from 46 to 34 in men and women respectively. The trends were good also in English younger groups, with decreasing rates since the end of 1990s (−5 and −3.4 % in men and women). On the contrary the rates of the elderly continued to increase over the entire period from 41 to 47 in men and from 28 to 30 in women.
Summarising, NHL showed a very clear and definite pattern: an early rise followed by decreasing rates, very quick in younger adults and little bit slower in older ones; the older group had not encouraging trends in UK.
NHL are one of the few tumours whose incidence and mortality have been increasing in Europe and North America over the last decades. Unlike incidence, still rising, mortality rates have started to level off or even to declined during the most recent years [53]. Some authors affirm that the striking incidence growth could be related with improved diagnostic procedures over time [54]. Moreover, a role at least partial could be played by changes in classification and registration [55, 56]. However, it is probable that these two phenomena have not caused a so large and generalised increase and it is conceivable that the overall growth of newly diagnosed cases is real, although a plausible causal hypothesis has not been found.
Leukaemia
Unlike NHL, leukaemia incidence trends did not present a definite pattern. The rates were very often stable or weakly growing, without any tendency to decrease. In Italy the rates of both sexes and age groups were quite stable, exception made for an upward trend in younger women (APC 2.6 %). In UK trends were slightly poorer: rates increased steadily and significantly over the whole period for each considered group (APC ranging from 0.5 to 1.2 %), except for elderly men who had a stable trend. Also American trends were less favourable than those of Italy. In middle aged adults of both sexes after an early period of stability followed a rise from the early 2000s, while the trends of the older age groups were stable in both sexes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree