Chapter 14
Head injury
Introduction
Head injury is a common presentation to the emergency department in the older adult and may be isolated or occur in association with other traumatic injuries. There are 155,000 cases of head injury in the older adult annually in the United States, resulting in 12,000 deaths (1). More than two-thirds (81%) of head injuries in adults aged 65 and older are caused by falls, mostly from ground level (2). Ten percent of cases result from motor vehicle accidents, with the patient either as driver, passenger or pedestrian (3).
Traumatic brain injury results from both the initial focal injury to the brain, such as contusion or haemorrhage, and from the secondary insult due to poor cerebral circulation, hypoxia or oedema. Initial management of head injury is focused on preventing or limiting secondary brain injury.
Changes in the structure of the brain and skull with ageing (Figure 14.1) make intracerebral bleeding more common following a head injury. Comorbidities and medication such as anticoagulants and antiplatelet agents further increase the likelihood of complications and worsen prognosis.
| Cerebral atrophy Brain weight decreases by 10–20% by age 80 causing increased distance between the brain and the skull, resulting in:
| Cerebral blood flow is reduced by 20%, with impaired cerebrovascular autoregulation, increasing the risk of secondary brain injury The dura becomes tightly adherent to the skull, so epidural haematomas are less common  Figure 14.1 Structural changes in the ageing brain. |
Evidence for a head injury must be carefully sought when assessing a patient following a fall. Intracerebral bleeding may occur after a seemingly trivial injury and present with non-specific or delayed symptoms and signs. A low threshold for CT imaging should be adopted.
Initial assessment
The approach to an older patient with a traumatic injury should begin with a primary survey according to Advanced Trauma Life Support® (ATLS®) principles, covered in depth in Chapter 11. Serious head injuries may require urgent intervention.
Airway and cervical spine immobilisation
The airway should be rapidly assessed. Patients who have sustained a significant head injury may develop an obstructed or unprotected airway due to reduced consciousness. Basic airway opening manoeuvres and delivery of high flow oxygen are required. The patient may need airway adjuncts or endotracheal intubation following rapid sequence induction.
The neck should be triple immobilised (collar, blocks and tape; or other three-point system) if any of the factors in Box 14.1 are present. Immobilisation should be maintained until a cervical spine injury can be excluded. Imaging is usually required for this purpose in older patients in whom clinical examination can be insensitive. In patients with agitation or degenerative cervical spine disease, immobilisation may actually worsen outcome. Chapter 11 covers cervical spine injuries in more detail.
Breathing
Significant head injuries may cause a reduced conscious level with respiratory insufficiency. Hypercapnoea causes vasodilatation of cerebral blood vessels, contributing to raised intracranial pressure (ICP) and secondary brain injury. Mechanical ventilation may be required to ensure adequate oxygenation.
Circulation with haemorrhage control
Cerebral blood flow decreases with age and an adequate mean arterial pressure is necessary to ensure cerebral perfusion. Prompt management of other injuries causing haemorrhage, including intravenous fluids, blood products or vasopressor support may be required to prevent secondary brain injury.
Disability
A brief neurological examination should take place during the primary survey and should include assessment of Glasgow Coma Scale (GCS), and pupillary size, equality and reactions. Ocular pathology such as glaucoma, cataract surgery and previous iritis may result in longstanding unequal pupils and may cause confusion when assessing the older patient.
Signs of critically raised ICP such as unequal pupils, hypertension or bradycardia necessitate immediate neurosurgical consultation and imaging. Temporary measures to reduce ICP include intravenous mannitol or hypertonic saline, mechanical ventilation and head elevation. Bedside INR measurement, if available, may indicate an urgent need for reversal of anticoagulants if there are signs consistent with intracerebral bleeding.
Exposure and environmental control
Inspect the patient for other life-threatening injuries. Hypothermia should be prevented with external warming devices.
History
Once the primary survey has been completed and any urgent issues arising from this addressed, a history of the head injury should be taken to guide examination and further investigation. Box 14.2 summarises the relevant aspects.
Many head injuries are consequences of falls related to a syncopal event and these will require further work-up to elucidate the underlying cause (Chapter 8).
Patients on anticoagulants such as warfarin are up to three times more likely to suffer from intracranial haemorrhage following head injury, with increasing likelihood as the INR rises above therapeutic levels (7). Patients receiving clopidogrel may have a higher prevalence of immediate traumatic intracranial haemorrhage compared with patients receiving warfarin (8). Antiplatelets as well as anticoagulants are associated with unfavourable outcome after head injury (9) and increased mortality following intracerebral haemorrhage (10–12). Dabigatran (a direct thrombin inhibitor) appears to be associated with a lower absolute risk of subdural haematoma than warfarin for patients with atrial fibrillation (13).
Excess use of alcohol increases the risk of serious head injury due to increased risk of falls and chronic liver disease resulting in coagulopathy. A low GCS should not be attributed to alcohol intoxification without first excluding other serious pathology.
Any head injury in an older adult should prompt consideration of elder abuse (Chapter 4).
Examination
Examination in the head-injured patient should include the points covered in Box 14.3.
| Eyes Examine pupillary responses, visual acuity, visual fields and eye movements | Scalp Inspect for a haematoma or laceration, and palpate for tenderness | Fundi Look for papilloedema or retinal haemorrhages Note any subconjunctival haemorrhages |
| Nose Look for evidence of epistaxis or CSF (cerebrospinal fluid) rhinorrhoea | 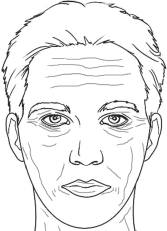 Figure 14.2 Examination of the head and face in the head injured patient. | Ears Examine the external ear and auditory canal. Look for CSF otorrhoea, haemotympanum or mastoid bruising |
| Face Look for facial lacerations or bruising. Palpate for tenderness over the facial bones. Check sensation and examine the cranial nerves | Cervical spine examination Followed by imaging if required | Mouth Check for missing teeth, mouth opening and mandibular tenderness |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







