“Classical-type” variants
Verrucous carcinoma
Basaloid squamous cell carcinoma
Spindle cell (sarcomatoid) squamous cell carcinoma
Papillary squamous cell carcinoma
Adenosquamous carcinoma
Lymphoepitheliomatous carcinoma
Sinonasal non-keratinizing carcinoma
Adenoid squamous (acantholytic) carcinoma
HPV-associated oropharyngeal squamous cell carcinoma
Fig. 1
Epidemiological distribution of HPV-positive cancers in head and neck region in Europe (according to Abogunrin et al. BMC Cancer, 2014; 14, 1)
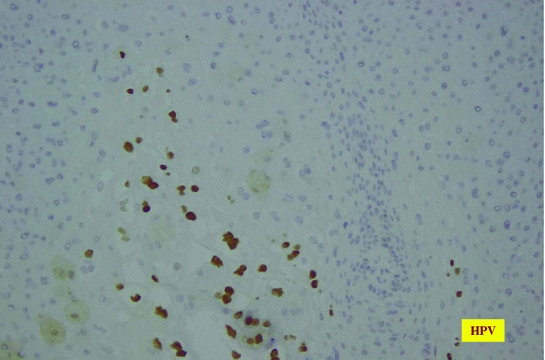
Fig. 2
Immunohistochemical visualization of HPV antigen expressed in squamous cell carcinoma
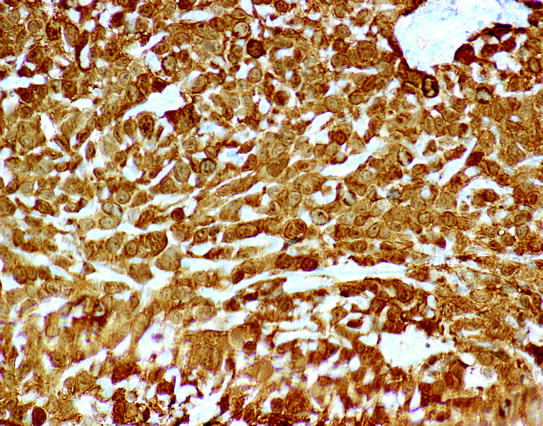
Fig. 3
Immunohistochemical visualization of overexpression of p16 in squamous cell carcinoma
2 Squamous Cell Carcinoma: “Classic” Type (“Classic” SCC)
The so-called classical type of SCC (with some histologically visible evidence of keratinization) of head and neck region consists of about 1 % of all malignancies in humans. However, it comprises more then 90 % of all malignancies in larynx. This type of tumor occurs usually in adults with peak from 6th to 7th decade. It is much more common in males, reaching incidence of 1/10,000 population, while among females, it is diagnosed as common as 1/100,000. But the most common male-to-female ratio is presented as 6:1. This classical type of tumor is attributed to the typical (in common sense) risk factors such as tobacco smoking (or exposure to tobacco smoke in environment) and alcohol abuse (Pai et al. 2009). In this “classical” variant, a very common alteration of p53 is found—especially in those associated with exposure to alcohol and tobacco. There are also correlations with long-standing gastroesophageal reflux, as well as radiation exposure. In some reports, there were indicated genetic risk factors, including Lynch syndrome, Bloom syndrome, and Li–Fraumeni syndrome. In classic SCC, an epidermal growth factor receptor (EGFR) overexpression is commonly found. It is related to more aggressive outcome. However, immunohistochemically estimated p16-positive cases along with low EGFR have better prognosis (Alexandrov et al. 2013). Morphologic examination reveals its occurrence in almost all anatomical areas. It could be supraglottic (this localization predominates in Europe), glottic (predominate in US patients), subglottic, and transglottic. Macroscopically, those tumors either could be ulcerative or might grow endophytically or as flat or even polypoid masses; verrucous and exophytic lesions are also described (Cardesa et al. 2011).
On microscopic examination, it could be keratinizing or non-keratinized SCC (Fig. 4).
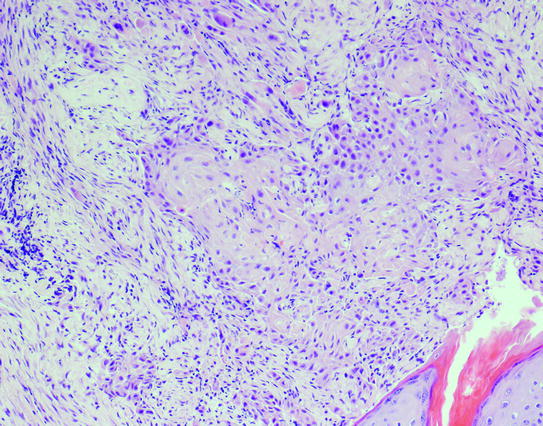
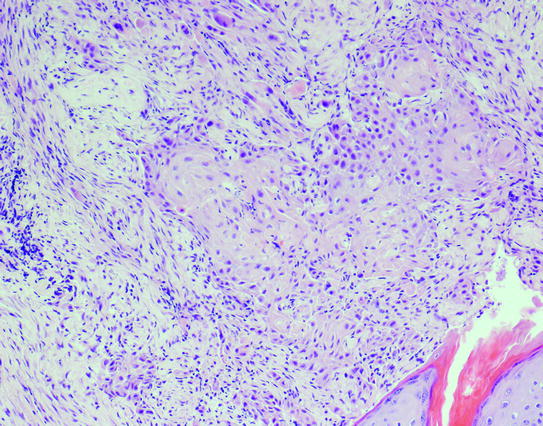
Fig. 4
Histological picture of classical squamous cell carcinoma
3 Squamous Cell Carcinoma: “Verrucous” Type (“Verrucous” SCC)
Verrucous type of SCC consists of about 3% of all SCC in head and neck region. This type of SCC is clearly correlated with HPV infection (Orvidas et al. 1998). It is most commonly found in oral cavity and then in larynx. In oral localization, it is found more common in females than in males, while in all other places male patients predominate (Orvidas et al. 1999). This tumor type has a distinct morphology. Macroscopically, it is described as broad-based warty mass that could be very large (even up to 10 cm of diameter). Microscopically, it also has distinct features such as clearly visible large club-shaped rete pegs (Fig. 5). In all tumors, there is abundant keratin. But usually, there is no pleomorphism of tumor cells. Additionally, usually there is no mitotic activity found. Those lately mentioned features are related to very good prognosis with a 5-year survival rate of about 75 % cases (Santoro et al. 2011; Teymoortash et al. 2014).
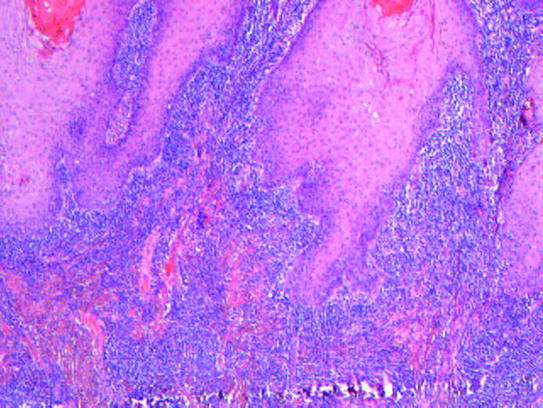
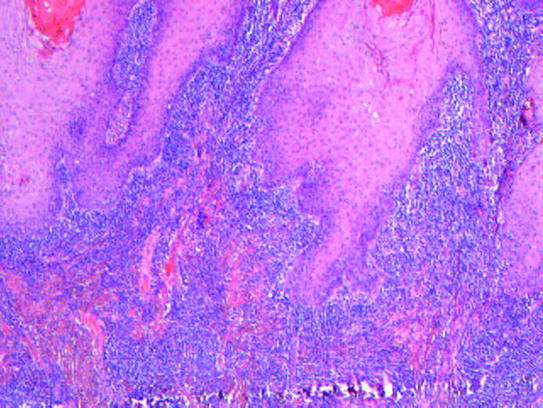
Fig. 5
Verrucous variant of squamous cell carcinoma
4 Squamous Cell Carcinoma: “Spindle Cell” (“Sarcomatoid”) Type (“Spindle Cell” SCC)
Sarcomatoid SCC according to its microscopic morphology resembling spindle cells of mesenchymal origin should be first differentially diagnosed with pleomorphic high-grade sarcoma. But primary sarcomas of this morphology in such localization are extremely rare. On the other hand, as in those tumors a coincidence of immunohistochemical markers for mesenchymal origin (positivity for vimentin) and ectodermal/epithelial origin (positive reactions with different types of cytokeratins) is found, and they could be called “collision” squamous cell carcinoma—highlighting their peculiar histology (Bishop et al. 2014). Sarcomatoid SCC consists of about 3 % of SCC in head and neck area. Some reports indicate radiation as their possible risk factor. Such tumors could be found in larynx. Next, in order of incidence is oral cavity, then nasal cavity (Stransky et al. 2011). According to gender differences, male cases are far more common than female. Macroscopically, they usually form polypoid mass of about 2 cm diameter. Microscopic pictures have some tips enabling its diagnosis include a biphasic morphology. There are areas of squamous cell carcinoma differentiation along with area of atypical spindle cells (resembling mesenchymal tumors, for instance fibrosarcoma or any other sarcoma). These tumors are usually hypercellular with prominent pleomorphism and high mitotic activity (Fig. 6). According to clinical data, the 5-year survival could reach 80 %.
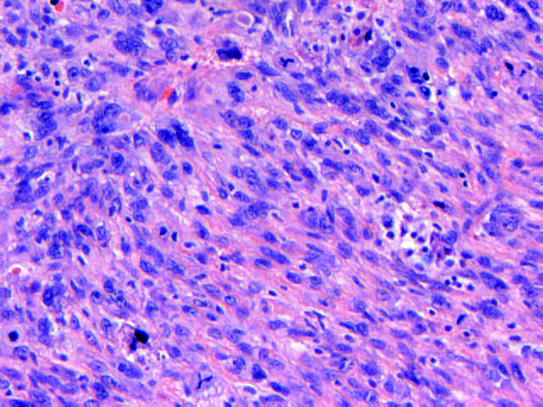
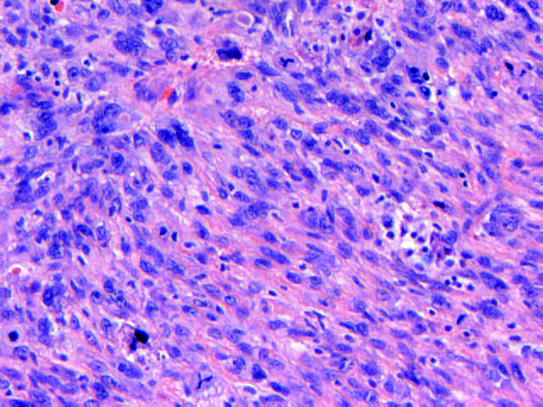
Fig. 6
Spindle cell variant of squamous cell carcinoma
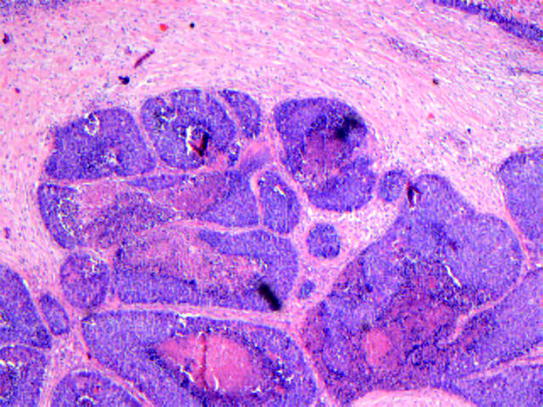
5 Basaloid Squamous Cell Carcinoma (BSCC)
BSCC is uncommon variant of “classic” SCC. It occurs in less than 1 % of squamous cell carcinoma in the head and neck region. BSCC is associated with conventional risk factors such as smoking and alcohol abuse (Marur et al. 2010). These lesions are typically aggressive variant of squamous cancer with early lymph node metastasis (68 % of patients have regional metastases at presentation) and poor prognosis with 2-year survival rates of less than 40 %. It has predilection for hypopharynx and larynx and less frequently oropharynx, but also occurs in other sites such as lung. Microscopically, BSCC has biphasic pattern which includes basaloid component and often areas with typical squamous differentiation (Fakhry et al. 2014). The basaloid cells are pleomorphic with minimal cytoplasm and hyperchromatic nuclei. They form demarcated nests of small basaloid cells with peripheral palisading and show numerous mitotic figures. Comedonecrosis is common (Fig. 7). Stromal hyalinization may be present. Pseudoglandular spaces resembling adenoid cystic carcinoma may occur. HPV-16 is detectable in majority (more than 75 % of cases) of oropharyngeal BSCC (El-Mofty 2012). The absence of HPV-16 in these tumors is associated with a decreased overall survival. HPV-positive tumors affected younger patients.