LN levels
Boundaries of LN levels
Recommended margins
Superior
Inferior
Medial
Lateral
Anterior
Posterior
Internal iliac
Bifurcation of the CI (usually the L5–S1 interspace)
Superior portion of the coccygeal muscle
Bladder, mesocolon, and mesorectum
IIV, iliac bone, sacroiliac joint, and psoas muscle (cranially) Internal obturator and piriform muscles (caudally)
Bladder
Sacral wing (cranially) Piriform muscle (caudally)
7 mm around vessels extend lateral borders to the pelvic sidewall
External iliac
Bifurcation of the CI (usually the L5–S1 interspace)
Femoral ring (when you do not see the lateral muscles of the abdominal wall anymore and the artery gets lateral)
Ureter (cranially) Bladder (caudally)
Iliac muscle (cranially)
Iliac bone, iliopsoas muscle, and EIV (caudally)
Fat of small bowel, ductus deference
EIV (cranially) Pubic bone (caudally)
7 mm around vessels extend anterior border by an additional 10 mm anterolaterally along iliopsoas muscle to include lateral external iliac nodes
Obturator
Superior portion of the obturator muscle
Superior border of the inferior branch of the pubic bone
Bladder
Acetabulum (cranially) Internal obturator muscle (caudally)
EIV
Internal obturator muscle
Join external and internal iliac regions with 18-mm-wide strip along pelvic sidewall
Presacral
Aortic bifurcation
Superior portion of the coccygeal bone
Suprapubic fat
Piriform muscle
Posterior wall of the rectum
Anterior surface of the sacrum
10 mm strip over anterior sacrum
The ongoing Prostate and pelvIs Versus prOsTate Alone treatment for Locally advanced prostate cancer (PIVOTAL) study uses different delineation techniques than RTOG in certain points. For instance, they do not describe the superior border as “L5–S1 interspace” but as “inferior to L5 vertebra” because they claim that the interspace is not a straight line, and the latter definition is more consistent. Secondly, they recommend the inferior border not the “top of” but “1 cm above the top of the pubic symphysis” in order to eliminate the anatomical variations of individual patients. They add the term “bowel expansion volume (BEV)” which is bowel + 3 mm margin, and they switch it with “bowel” and add the rectum and muscle as critical organs that should not be included in the LN-CTV. They recommend giving a 12 mm margin anterior to the sacrum for presacral LNs. Finally, they claim that internal and external iliac volumes should be connected with an 18 mm strip, intravenous contrast should be used to help identification of vessels, an 18 mm strip should be given from the inner surface of bony pelvic sidewall in order to constitute obturator lymphatic region, and all small white dots which may be representing small blood vessels and associated LNs should be included.
Despite the recommendations of the RTOG guideline , there are studies claiming that these nodal regions do not entirely cover the areas under recurrence risk. Meijer et al. studied the distribution of LN metastases on magnetic resonance (MR) lymphography and found that more than half of the patients had ≥1 LN in areas which are not included in the RTOG guideline [26]. They showed that an important percentage of patients have metastases in the para-aortic, proximal common iliac, perirectal lymphatics, and even in the perivesical and inguinal regions.
They also stated that the risk of perirectal and proximal common iliac LN involvement was associated with GS and PSA level, respectively, concluding that the respective lymphatic areas should be included in the LN-CTV in patients with these high risk factors.
A recent study revealed that in approximately half of the patients, the superior border of the RTOG guideline does not cover the lymphatic area that shows recurrence [27]. The authors concluded that extending the field can cover these areas or adding androgen deprivation therapy can minimize the risk of more superior LN recurrence in high-risk patients. On the other hand, a study from the Massachusetts General Hospital reported that 95% of the LNs are in 1.5 cm proximity from large vessels and iliac vessels under high-risk of respective LN involvement should be given a radial margin of 2 cm for adequate coverage of the subclinical disease that cannot be shown by imaging techniques [28]. They recommended delineating the distal 2.5 cm portion of common iliac, proximal 9 cm portion of external iliac, and proximal 8.5 cm of internal iliac vessels starting from the iliac bifurcation. Based on these findings, the currently ongoing RTOG 0924 trial is evaluating the benefit of extending the superior border of RT portals.
Pelvic lymphatic delineation in a prostate cancer treated with definitive IGRT is depicted in Fig. 15.1.
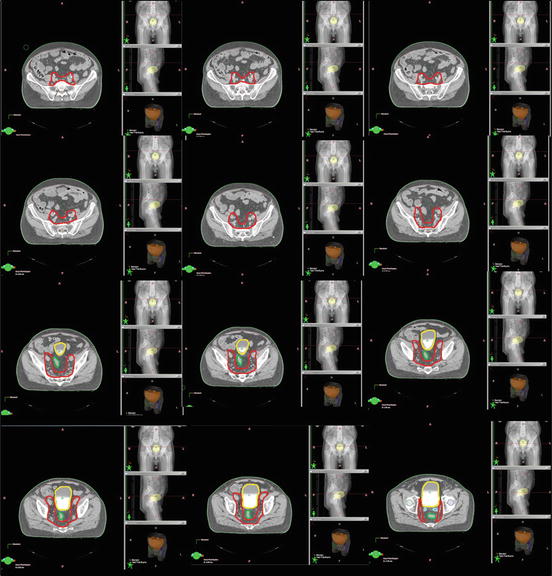
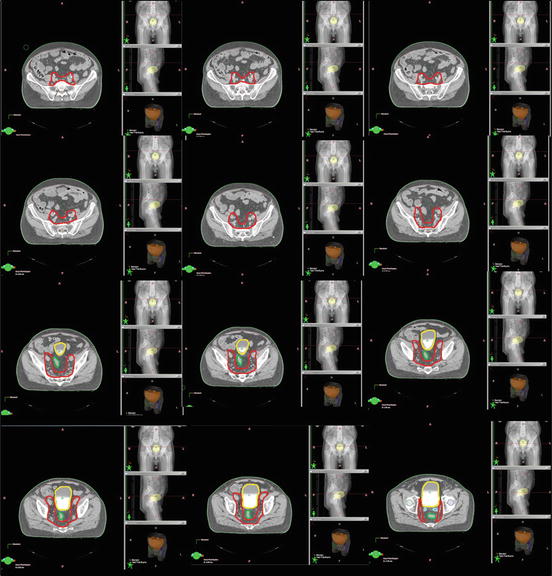
Fig. 15.1
Pelvic lymphatic delineation in a prostate cancer treated with definitive IGRT
Conclusion
Elective nodal irradiation is not a standard procedure in patients with N0 prostate cancer that undergo RT. However, irradiation of pelvic LNs can be performed in patients with a high risk of or that already have LN metastasis. The recommended delineation guideline of the pelvic LNs is given in detail in this chapter. Although there are studies reporting the insufficiency of the available guideline, the variations in contouring the LNs between the institutions can be minimized if these recommendations are applied in clinical practice.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree