Anabolic steroids
Athletics
Female athlete triad
Injury
Overuse injuries
Performance-enhancing drugs
Physical fitness and conditioning
Preparticipation physical examination
Sports
Improve bone health
Improve cardiorespiratory and muscular fitness
Decrease levels of body fat
Reduce symptoms of depression
Early death
Coronary heart disease
Stroke
High blood pressure
Type 2 diabetes
Breast and colon cancer
Falls
Depression
Assessing the risks associated with athletic participation for individual AYAs
Prescribing exercise and advising on sports participation to improve fitness while minimizing athletic injury and illness
TABLE 19.1 Classification of Sports by Contact | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||
American Academy of Family Physicians (AAFP)
American Academy of Pediatrics (AAP)
American College of Sports Medicine (ACSM)
American Medical Society for Sports Medicine (ASSM)
American Orthopaedic Society for Sports Medicine (AOSSM)
American Osteopathic Academy of Sports Medicine (AOASM)
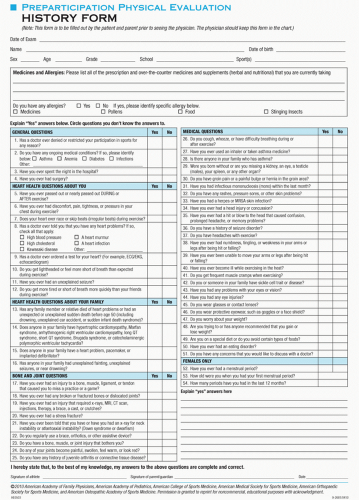
Screening for conditions that may be life-threatening or disabling
Screening for conditions that may predispose to injury or illness
Family history of premature death (sudden or otherwise).
Family history of heart disease in surviving relatives; significant disability from cardiovascular disease in close relatives younger than 50 years; or specific knowledge of the occurrence of certain conditions (hypertrophic cardiomyopathy [HCM], long-QT syndrome, Marfan syndrome, or clinically important arrhythmias).
Personal history of heart murmur.
Personal history of systemic hypertension.
Personal history of excessive fatigability.
Personal history of syncope, excessive or progressive shortness of breath, or chest pain or discomfort, particularly with exertion.
Past injuries that caused the athlete to miss a game or practice.
Any loss of consciousness or memory occurring after a head injury.
Previous exclusion from sports for any reason.
Allergies, asthma, or exercise-induced bronchospasm.
Medications and supplements, used currently or in the last 6 months.
The menstrual history in females.
A history of relatively rapid increase or decrease in body weight and the athlete’s perception of current body weight.
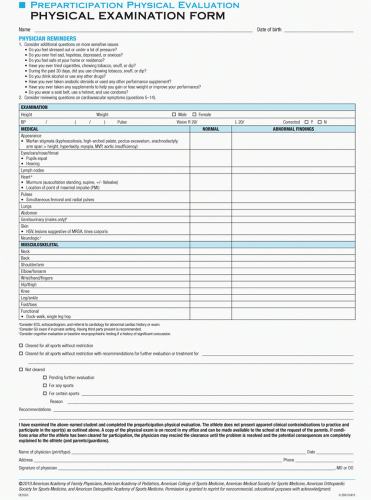
Height, weight, and body mass index (BMI): Obesity, by itself, is not a reason for exclusion. However, the increased risk of heat illness and how that risk might be reduced must be discussed with the athlete, parent, and coach.
Blood pressure and pulse: Blood pressure should be taken in the right arm with the athlete sitting. Athletes with hypertension should be evaluated but not excluded from participation unless the hypertension is severe. Bradycardia in the 40- to 50-bpm range occurs commonly in the highly conditioned athlete and does not need evaluation if the athlete is asymptomatic.
Visual acuity and pupil equality: AYAs with corrected visual acuity worse than 20/40 in one or both eyes should be referred for further evaluation but are not excluded from participation if protective eyewear is worn. It is important to document the presence of baseline anisocoria before any closed head injury occurs.
Skin: Infections that are highly contagious (e.g., varicella, impetigo) should be identified. Identified athletes should not be allowed to return to sports in which skin-to-skin contact is possible until they are determined to be noninfectious (Table 19.2).
Teeth and mouth: These are examined only if the history suggests an acute problem.
Cardiac examination: AHA recommendations for PPE cardiac examination include the following:
Perform precordial auscultation in supine and standing positions to identify heart murmurs consistent with dynamic left ventricular outflow obstruction.
Assess femoral artery or lower extremity pulses to exclude coarctation of the aorta.
Recognize the physical stigmata of Marfan syndrome; refer for further evaluation if a male is taller than 6 ft or a female taller than 5 ft 10 in and has
a family history of Marfan syndrome
or
two of the following:
Kyphosis
High-arched palate
Pectus excavatum
Arachnodactyly
Arm span > height
Murmur (mitral valve prolapse or aortic)
Myopia
Lens dislocation
Thumb or wrist signs
Assess brachial artery blood pressure in the sitting position.
Document the presence of murmurs, clicks, or rubs (see Chapter 16). Normal or physiologic murmurs are characteristically <4/6 systolic murmurs that decrease in intensity from supine to standing with no diastolic component and with a normal physiologic split second heart sound (S2). In contrast, the murmur of HCM (when a murmur is present) may sound like a normal murmur except that it increases in intensity when the patient moves from the supine to the standing position.
Abdomen: Organomegaly is a disqualifying condition for collision/contact or limited-contact sports until definitive evaluation and individual assessment for clearance has been completed.
Genitalia: An undescended testicle is not a contraindication to participation in contact sports; however, the athlete should wear a protective cup to protect the other, descended testis. An evaluation for the unidentified testis is necessary.
Sexual maturation stage: Sexual maturity rating assessment is part of the adolescent physical examination, but it has no role in determining whether the athlete should play a given sport.
Musculoskeletal screening: General musculoskeletal screening should include muscle strength, range-of-motion and joint-stability testing, and evaluation for structural abnormalities of major joints (e.g., ankle, knee, shoulder, elbow, back). An efficient musculoskeletal screening examination is demonstrated in Figures 19.2 to 19.11. A more in-depth examination of the specific body parts should be performed if there are concerns from the history or general screening examination (listed in parentheses are diagnoses to consider if the examination finding is abnormal):
Body symmetry (Figs. 19.2 to 19.11): Observe the adolescent or young adult standing with arms at the sides, dressed in shorts and a shirt that allows inspection of the distal quadriceps muscles and acromioclavicular joints, respectively. Look for the following:
Head tilted or turned to side (consider primary cervical spine injury, primary or secondary trapezius, or cervical muscle spasm)
Asymmetry of shoulder heights (trapezius spasm, shoulder injury, scoliosis)
Enlarged acromioclavicular joint (previous acromioclavicular joint sprain, shoulder separation)
Asymmetrical iliac crest heights (scoliosis or leg-length difference, back spasm)
Swollen knee; prominent tibial tuberosity (any knee injury, Osgood-Schlatter disease). Ask the athlete to contract (“tighten”) the quadriceps muscles, and look for atrophy of the vastus medialis obliquus, a characteristic of any knee or lower extremity injury in which the athlete avoids normal use of that leg.
Swollen ankle (ankle sprain that has not been rehabilitated)
Neck examination (Fig. 19.3): This is especially important in players with a previous history of neck injury and brachial plexopathy (referred to as stingers or burners).
Have the athlete perform the following maneuvers:
Look at the floor (cervical flexion).
Look at the ceiling (cervical extension).
Look over the left shoulder, then over the right shoulder (left and right rotation, respectively).
TABLE 19.2 Medical Conditions and Sports Participation
Condition
May Participate
Atlantoaxial instability (instability of the joint between cervical vertebrae 1 and 2)
Qualified yes
Explanation: Athlete (particularly if he or she has Down syndrome or juvenile rheumatoid arthritis with cervical involvement) needs evaluation to assess the risk of spinal cord injury during sports participation, especially when using a trampoline.
Bleeding disorder
Qualified yes
Explanation: Athlete needs evaluation.
Cardiovascular disease
Carditis (inflammation of the heart)
No
Explanation: Carditis may result in sudden death with exertion.
Hypertension (high blood pressure)
Qualified yes
Explanation: Those with hypertension >5 mm Hg above the 99th percentile for age, gender, and height should avoid heavy weight lifting and power lifting, bodybuilding, and high-static component sports. Those with sustained hypertension (>95th percentile for age, gender, and height) need evaluation. The National High Blood Pressure Education Program Working Group report defined prehypertension and stage 1 and stage 2 hypertension in children and adolescents younger than 18 years of age.
Congenital heart disease (structural heart defects present at birth)
Qualified yes
Explanation: Consultation with a cardiologist is recommended. Those who have mild forms may participate fully in most cases; those who have moderate or severe forms or who have undergone surgery need evaluation. The 36th Bethesda Conference defined mild, moderate, and severe disease for common cardiac lesions.
Dysrhythmia (irregular heart rhythm)
Qualified yes
Long-QT syndrome
Malignant ventricular arrhythmias
Symptomatic Wolff-Parkinson-White syndrome
Advanced heart block
Family history of sudden death or previous sudden cardiac event
Implantation of a cardioverter-defibrillator
Explanation: Consultation with a cardiologist is advised. Those with symptoms (chest pain, syncope, near-syncope, dizziness, shortness of breath, or other symptoms of possible dysrhythmia) or evidence of mitral regurgitation on physical examination need evaluation. All others may participate fully.
Heart murmur
Qualified yes
Explanation: If the murmur is innocent (does not indicate heart disease), full participation is permitted. Otherwise, athlete needs evaluation (see structural heart disease, especially HCM and mitral valve prolapse).
Structural/acquired heart disease
HCM
Qualified no
Coronary artery anomalies
Qualified no
Arrhythmogenic right ventricular cardiomyopathy
Qualified no
Acute rheumatic fever with carditis
Qualified no
Ehlers-Danlos syndrome, vascular form
Qualified no
Marfan syndrome
Qualified yes
Mitral valve prolapse
Qualified yes
Anthracycline use
Qualified yes
Explanation: Consultation with a cardiologist is recommended. The 36th Bethesda Conference provided detailed recommendations. Most of these conditions carry a significant risk of sudden cardiac death associated with intense physical exercise. HCM requires thorough and repeated evaluations, because disease may change manifestations during later adolescence. Marfan syndrome with an aortic aneurysm can also cause sudden death during intense physical exercise. Athlete who has ever received chemotherapy with anthracyclines may be at increased risk of cardiac problems because of the cardiotoxic effects of the medications, and resistance training in this population should be approached with caution; strength training that avoids isometric contractions may be permitted. Athlete needs evaluation.
Vasculitis/vascular disease
Qualified yes
Kawasaki disease (coronary artery vasculitis)
Pulmonary hypertension
Explanation: Consultation with a cardiologist is recommended. Athlete needs individual evaluation to assess risk on the basis of disease activity, pathologic changes, and medical regimen.
Cerebral palsy
Qualified yes
Explanation: Athlete needs evaluation to assess functional capacity to perform sports-specific activity.
Diabetes mellitus
Yes
Explanation: All sports can be played with proper attention and appropriate adjustments to diet (particularly carbohydrate intake), blood glucose concentrations, hydration, and insulin therapy. Blood glucose concentrations should be monitored before exercise, every 30 min during continuous exercise, 15 min after completion of exercise, and at bedtime.
Diarrhea, infectious
Qualified no
Explanation: Unless symptoms are mild and athlete is fully hydrated, no participation is permitted, because diarrhea may increase risk of dehydration and heat illness (see fever).
Eating disorders
Qualified yes
Explanation: Athlete with an eating disorder needs medical and psychiatric assessment before participation.
Eyes
Qualified yes
Functionally 1-eyed athlete
Loss of an eye
Detached retina or family history of retinal detachment at young age
High myopia
Connective tissue disorder, such as Marfan or Stickler syndrome
Previous intraocular eye surgery or serious eye injury
Explanation: A functionally 1-eyed athlete is defined as having best-corrected visual acuity worse than 20/40 in the poorer-seeing eye. Such an athlete would suffer significant disability if the better eye were seriously injured, as would an athlete with loss of an eye. Specifically, boxing and full-contact martial arts are not recommended for functionally 1-eyed athletes, because eye protection is impractical and/or not permitted. Some athletes who previously underwent intraocular eye surgery or had a serious eye injury may have increased risk of injury because of weakened eye tissue. Availability of eye guards approved by the American Society for Testing and Materials and other protective equipment may allow participation in most sports, but this must be judged on an individual basis.
Conjunctivitis, infectious
Qualified no
Explanation: Athlete with active infectious conjunctivitis should be excluded from swimming.
Fever
No
Explanation: Elevated core temperature may be indicative of a pathologic medical condition (infection or disease) that is often manifest by increased resting metabolism and heart rate. Accordingly, during athlete’s usual exercise regimen, the presence of fever can result in greater heat storage, decreased heat tolerance, increased risk of heat illness, increased cardiopulmonary effort, reduced maximal exercise capacity, and increased risk of hypotension because of altered vascular tone and dehydration. On rare occasions, fever may accompany myocarditis or other conditions that may make usual exercise dangerous.
Gastrointestinal
Qualified yes
Malabsorption syndromes (celiac disease or cystic fibrosis)
Explanation: Athlete needs individual assessment for general malnutrition or specific deficits resulting in coagulation or other defects; with appropriate treatment, these deficits can be treated adequately to permit normal activities.
Short-bowel syndrome or other disorders requiring specialized nutritional support, including parenteral or enteral nutrition
Explanation: Athlete needs individual assessment for collision, contact, or limited-contact sports. Presence of central or peripheral, indwelling, venous catheter may require special considerations for activities and emergency preparedness for unexpected trauma to the device(s).
Heat illness, history of
Qualified yes
Explanation: Because of the likelihood of recurrence, athlete needs individual assessment to determine the presence of predisposing conditions and behaviors and to develop a prevention strategy that includes sufficient acclimatization (to the environment and to exercise intensity and duration), conditioning, hydration, and salt intake, as well as other effective measures to improve heat tolerance and to reduce heat injury risk (such as protective equipment and uniform configurations).
Hepatitis, infectious (primarily hepatitis C)
Yes
Explanation: All athletes should receive hepatitis B vaccination before participation. Because of the apparent minimal risk to others, all sports may be played as athlete’s state of health allows. For all athletes, skin lesions should be covered properly, and athletic personnel should use universal precautions when handling blood or body fluids with visible blood.
HIV infection
Yes
Explanation: Because of the apparent minimal risk to others, all sports may be played as athlete’s state of health allows (especially if viral load is undetectable or very low). For all athletes, skin lesions should be covered properly, and athletic personnel should use universal precautions when handling blood or body fluids with visible blood. However, certain sports (such as wrestling and boxing) may create a situation that favors viral transmission (likely bleeding plus skin breaks). If viral load is detectable, then athletes should be advised to avoid such high-contact sports.
Kidney, absence of one
Qualified yes
Explanation: Athlete needs individual assessment for contact, collision, and limited-contact sports. Protective equipment may reduce risk of injury to the remaining kidney sufficiently to allow participation in most sports, providing such equipment remains in place during activity.
Liver, enlarged
Qualified yes
Explanation: If the liver is acutely enlarged, then participation should be avoided because of risk of rupture. If the liver is chronically enlarged, then individual assessment is needed before collision, contact, or limited-contact sports are played. Patients with chronic liver disease may have changes in liver function that affect stamina, mental status, coagulation, or nutritional status.
Malignant neoplasm
Qualified yes
Explanation: Athlete needs individual assessment.
Musculoskeletal disorders
Qualified yes
Explanation: Athlete needs individual assessment.
Neurologic disorders
History of serious head or spine trauma or abnormality, including craniotomy, epidural bleeding, subdural hematoma, intracerebral hemorrhage, second-impact syndrome, vascular malformation, and neck fracture
Qualified yes
Explanation: Athlete needs individual assessment for collision, contact, or limited-contact sports.
History of simple concussion (mild traumatic brain injury), multiple simple concussions, and/or complex concussion
Qualified yes
Explanation: Athlete needs individual assessment. Research supports a conservative approach to concussion management, including no athletic participation while symptomatic or when deficits in judgment or cognition are detected, followed by graduated return to full activity.
Myopathies
Qualified yes
Explanation: Athlete needs individual assessment.
Recurrent headaches
Yes
Explanation: Athlete needs individual assessment.
Recurrent plexopathy (burner or stinger) and cervical cord neuropraxia with persistent defects
Qualified yes
Explanation: Athlete needs individual assessment for collision, contact, or limited-contact sports; regaining normal strength is important benchmark for return to play.
Seizure disorder, well controlled
Yes
Explanation: Risk of seizure during participation is minimal.
Seizure disorder, poorly controlled
Qualified yes
Explanation: Athlete needs individual assessment for collision, contact, or limited-contact sports. The following noncontact sports should be avoided: archery, riflery, swimming, weightlifting, power lifting, strength training, and sports involving heights. In these sports, occurrence of a seizure during activity may pose a risk to self or others.
Obesity
Yes
Explanation: Because of the increased risk of heat illness and cardiovascular strain, obese athlete particularly needs careful acclimatization (to the environment and to exercise intensity and duration), sufficient hydration, and potential activity and recovery modifications during competition and training.
Organ transplant recipient (and those taking immunosuppressive medications)
Qualified yes
Explanation: Athlete needs individual assessment for contact, collision, and limited-contact sports. In addition to potential risk of infections, some medications (e.g., prednisone) may increase tendency for bruising.
Ovary, absence of one
Yes
Explanation: Risk of severe injury to remaining ovary is minimal.
Pregnancy/postpartum
Qualified yes
Explanation: Athlete needs individual assessment. As pregnancy progresses, modifications to usual exercise routines will become necessary. Activities with high risk of falling or abdominal trauma should be avoided. Scuba diving and activities posing risk of altitude sickness should also be avoided during pregnancy. After the birth, physiologic and morphologic changes of pregnancy take 4 to 6 weeks to return to baseline.
Respiratory conditions
Pulmonary compromise, including cystic fibrosis
Qualified yes
Explanation: Athlete needs individual assessment but, generally, all sports may be played if oxygenation remains satisfactory during graded exercise test. Athletes with cystic fibrosis need acclimatization and good hydration to reduce risk of heat illness.
Asthma
Yes
Explanation: With proper medication and education, only athletes with severe asthma need to modify their participation. For those using inhalers, recommend having a written action plan and using a peak flowmeter daily. Athletes with asthma may encounter risks when scuba diving.
Acute upper respiratory infection
Qualified yes
Explanation: Upper respiratory obstruction may affect pulmonary function. Athlete needs individual assessment for all except mild disease (see fever).
Rheumatologic diseases
Qualified yes
Juvenile rheumatoid arthritis
Explanation: Athletes with systemic or polyarticular juvenile rheumatoid arthritis and history of cervical spine involvement need radiographs of vertebrae C1 and C2 to assess risk of spinal cord injury. Athletes with systemic or HLA-B27-associated arthritis require cardiovascular assessment for possible cardiac complications during exercise. For those with micrognathia (open bite and exposed teeth), mouth guards are helpful. If uveitis is present, risk of eye damage from trauma is increased; ophthalmologic assessment is recommended. If visually impaired, guidelines for functionally 1-eyed athletes should be followed.
Juvenile dermatomyositis, idiopathic myositis
Systemic lupus erythematosis
Raynaud phenomenon
Explanation: Athlete with juvenile dermatomyositis or systemic lupus erythematosis with cardiac involvement requires cardiology assessment before participation. Athletes receiving systemic corticosteroid therapy are at higher risk of osteoporotic fractures and avascular necrosis, which should be assessed before clearance; those receiving immunosuppressive medications are at higher risk of serious infection. Sports activities should be avoided when myositis is active. Rhabdomyolysis during intensive exercise may cause renal injury in athletes with idiopathic myositis and other myopathies. Because of photosensitivity with juvenile dermatomyositis and systemic lupus erythematosis, sun protection is necessary during outdoor activities. With Raynaud phenomenon, exposure to the cold presents risk to hands and feet.
Sickle cell disease
Qualified yes
Explanation: Athlete needs individual assessment. In general, if illness status permits, all sports may be played; however, any sport or activity that entails overexertion, overheating, dehydration, or chilling should be avoided. Participation at high altitude, especially when not acclimatized, also poses risk of sickle cell crisis.
Sickle cell trait
Yes
Explanation: Athletes with sickle cell trait generally do not have increased risk of sudden death or other medical problems during athletic participation under normal environmental conditions. However, when high exertional activity is performed under extreme conditions of heat and humidity or increased altitude, such catastrophic complications have occurred rarely. Athletes with sickle cell trait, like all athletes, should be progressively acclimatized to the environment and to the intensity and duration of activities and should be sufficiently hydrated to reduce the risk of exertional heat illness and/or rhabdomyolysis. According to National Institutes of Health management guidelines, sickle cell trait is not a contraindication to participation in competitive athletics, and there is no requirement for screening before participation. More research is needed to assess fully potential risks and benefits of screening athletes for sickle cell trait.
Skin infections, including herpes simplex, molluscum contagiosum, verrucae (warts), staphylococcal and streptococcal infections (furuncles [boils], carbuncles, impetigo, methicillin-resistant Staphylococcus aureus [cellulitis and/or abscesses]), scabies, and tinea
Qualified yes
Explanation: During contagious periods, participation in gymnastics or cheerleading with mats, martial arts, wrestling, or other collision, contact, or limited-contact sports is not allowed.
Spleen, enlarged
Qualified yes
Explanation: If the spleen is acutely enlarged, then participation should be avoided because of risk of rupture. If the spleen is chronically enlarged, then individual assessment is needed before collision, contact, or limited-contact sports are played.
Testicle, undescended or absence of one
Yes
Explanation: Certain sports may require a protective cup.
This table is designed for use by medical and nonmedical personnel.
“Needs evaluation” means that a physician with appropriate knowledge and experience should assess the safety of a given sport for an athlete with the listed medical condition. Unless otherwise noted, this need for special consideration is because of variability in the severity of the disease, the risk of injury for the specific sports listed in Table 19.1
From Committee on Sports Medicine and Fitness. Medical conditions affecting sports participation. Pediatrics 2008;121:841.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree