© Springer-Verlag Berlin Heidelberg 2017
Sun-Whe Kim and Hiroki Yamaue (eds.)Pancreatic Cancer10.1007/978-3-662-47181-4_1313. Guideline for the Management of Pancreatic Neuroendocrine Tumor
Gabriele Spoletini1, Domenico Tamburrino1, Francesca Muffatti2, Stefano Crippa2, Valentina Andreasi2, Stefano Partelli2 and Massimo Falconi2
(1)
HPB and Liver Transplant Surgery, Royal Free Hospital, NHS Foundation Trust, London, UK
(2)
Pancreatic Surgery Unit, Pancreas Center, San Raffaele Hospital, “Vita-Salute” University, Via Olgettina, 60, 20132 Milan, Italy
13.1 Introduction
Pancreatic neuroendocrine neoplasms (PNENs) are divided in functional tumors, which cause syndromes deriving from the secretion of active hormones, and nonfunctional tumors, which commonly secrete hormones, not causing specific symptoms. A number of factors influence treatment and prognosis, which are discussed in this chapter.
13.2 Management of Functioning Pancreatic Neuroendocrine Neoplasms (F-PNENs)
13.2.1 Surgery for Gastrinoma
Gastrinomas are neuroendocrine neoplasms generally localized in the duodenum and pancreas that secrete gastrin hormone, causing Zollinger-Ellison syndrome (ZES), and are characterized by gastric acid hypersecretion and severe acid-related peptic disease and diarrhea [1].
Approximately 80% of gastrinomas are sporadic, while 20–30% are associated with multiple endocrine neoplasia type 1 (MEN1) [2].
Gastrinomas are the most frequent malignant, functional pancreatic neuroendocrine neoplasms (F-PNENs), but only around 25% of them are localized in the pancreas. In fact the majority of them is found in the “gastrinoma triangle” that comprises the head of the pancreas and the duodenal sweep.
Medical therapy is the mainstay in patients with ZES in order to control acid hypersecretion and to prevent peptic complications. Proton pump inhibitors (PPIs) are the current standard of care, and after their introduction, total gastrectomy for control of symptoms has become extremely rare [3].
There is general consensus that complete resection of the primary neoplasm and the involved lymph nodes should be offered to all patients with sporadic ZES and potentially resectable disease arising from the pancreas and/or the duodenum with no metastatic disease and who are fit for surgery [4].
Surgery decreases the rate of development of LM, which is the most important prognostic factor for long-term survival and to increase disease-related survival [5].
In both sporadic gastrinoma and MEN1-associated gastrinoma, duodenal lesions are frequently small, have positive lymph nodes in 40–60% of cases, and are often not seen on preoperative imaging including endoscopic ultrasound (EUS) [6].
Experienced surgeons are usually able to identify over 90% of sporadic gastrinomas with the combination of preoperative imaging techniques, while intraoperative transduodenal illumination and duodenotomy are essential in detecting very small gastrinomas within the duodenum wall [7].
For sporadic left-sided pancreatic gastrinoma, central or distal pancreatectomy (with or without splenectomy) can be proposed [8].
However, the type and extent of surgery to be offered remain a controversial issue for gastrinomas due to the morbidity associated with pancreatic surgery. Several groups have suggested that gastrinomas should be enucleated or removed by a formal pancreatic resection with lymphadenectomy. The most common operation for duodenal gastrinomas includes duodenotomy, enucleation of any head or uncinate tumors, and peripancreatic lymph node dissection with or without distal pancreatectomy. However, it was noted that more conservative approaches rather than formal resections are associated with higher recurrence rates [9]. Other groups favor more aggressive approaches such as pancreaticoduodenectomy (PD) as the first-line procedure both in sporadic and MEN1-associated gastrinoma [10].
Regional lymphadenectomy is recommended in sporadic gastrinomas, independently of the primary location, because lymph node involvement is almost the rule in this type of neoplasms [11]. A blind resection in non-radiologically seen lesions should not be recommended and must be carefully evaluated by a multidisciplinary setting. A recent study demonstrated that all sporadic gastrinomas may benefit from radical surgery regardless of a preoperative radiological proof of localization. In this study the disease-free rate after curative resection was higher among patients with no radiological proof compared with those with radiologically seen gastrinomas [12].
Gastrinomas in MEN1 occur frequently in the duodenum. Traditionally, MEN1-associated gastrinomas were considered virtually impossible to cure with surgery, which was aimed at symptom control and prolonging survival. More recent studies demonstrated that patients treated conservatively with medical therapy for ZES have a risk of developing liver metastases of 23–29% compared with the 3–5% in patients treated with surgical resection [13]. One study demonstrated that gastrinomas larger than 3 cm in size had a ten times higher risk of developing liver metastases than smaller tumors [14]. As the risk of LM is strictly related to the size of primary lesion, Bartsch et al. suggest to offer surgical resection if the biochemical diagnosis is unequivocal and in the presence of lesions >1 cm [15]. The most appropriate surgical treatment in MEN1-associated gastrinoma is still debated. The North American Neuroendocrine Tumor Society (NANETS) consensus guidelines highlight that PD is rarely indicated for gastrinomas in MEN1 [16].
Instead, some groups regard PD as the most effective procedure. Lopez et al. achieved significantly higher long-term cure rate of ZES in a group of patients undergoing PD (92%) than in a group receiving atypical resections (33%), although the disease-specific 10-year survival was not statistically different (PD group 100%, non-PD group 89%). Notably, the two groups had similar incidence of postoperative diabetes mellitus and pancreatic fistula rate [10]. Even total pancreaticoduodenectomy has been advocated as an adequate procedure in selected patients [17].
13.2.2 Surgery for Insulinoma
Insulinomas are the most common F-PNENs and cause a syndrome characterized by severe hypoglycemia due to unregulated insulin secretion.
The vast majority of insulinomas are benign, unifocal lesions, arising within the pancreatic gland. Around 5% of the insulinomas are diagnosed in the setting of a MEN1 syndrome [4].
Being intra-pancreatic, they can be detected by EUS which has greater sensitivity and specificity for lesions located inside the pancreas than those outside of it. EUS can also elucidate whether the tumor can be enucleated or requires a formal resection, by measuring the distance from the main pancreatic duct (MPD). Surgical treatment in most of the cases is curative, with 100% rates in some series [18]. Due to the unifocality and benign nature, a laparoscopic approach is feasible in most cases and has shown equivalent outcomes for cure and shorter hospital stay [19]. If the tumor is farer than 3 mm from the MPD, enucleations are commonly performed, after exploration of the whole pancreas including intraoperative ultrasound (IOUS). Tumors of larger size or close to the MPD should be treated with a standard resection. In case of unclear preoperative tumor location, a surgical exploration is recommended, and frozen section analysis and insulin sampling may be required intraoperatively [20]. Lymphadenectomy is not routinely required due to the most likely benign nature of insulinomas. The use of ablative techniques for insulinomas is controversial. Although firm evidences are still lacking, endoscopic or percutaneous ablative technique may be a valid option in patients who are unfit for surgery [18]. In those rare malignant cases, in recurrent or metastatic disease, a radical surgery aimed at treating locoregional or metastatic deposits has been performed and may be indicated. Peripancreatic lymph node dissection should be performed and resection of the primary tumor and accessible metastases is advocated. Tumor debulking is useful for reducing hypoglycemic symptoms and improving long-term survival [21]. Insulinomas occur in almost 20% of patient with MEN1 syndrome. They tend to have a more aggressive behavior comparing to sporadic cases. They are usually multiple and associated with an earlier age at onset. Since insulinomas in MEN1 are at higher risk for being malignant and multifocal, formal pancreatic resections have been advocated [22]. In MEN1-affected patients with insulinoma, other PNENs are often present. Preoperative localization to determine which PNENs are the insulinomas is mandatory. Instead, other small NF-PNENs may be left behind in order to minimize the amount of parenchyma excised. In these patients, preoperative intra-arterial calcium injections with hepatic venous insulin sampling as well as intraoperative insulin sampling may be required [23].
13.2.3 Surgery for Rare Functioning Neuroendocrine Neoplasms (RF-NENs)
Rare functioning neuroendocrine neoplasms (RF-NENs) can occur in the pancreas or in other locations [VIPomas, somatostatinomas, GRHomas, ACTHomas, PNENs causing carcinoid syndrome or hypercalcemia (PTHrp-omas)]. Each RF-NEN is associated with a particular syndrome that results from the excessive hormonal secretion [24]. Indications for surgery are based on symptom control, tumor morphology and extent, malignancy, and possible presence of metastases.
In patients who are fit for surgery, curative treatment should always be sought, especially if metastatic disease is only localized to the liver and is potentially resectable [25]. The type of surgery depends on the location of the primary – PDs, distal pancreatectomy, or other partial resections. A proper lymphadenectomy is required as RF-NENs are often of malignant nature [8].
In general laparoscopic surgery is not recommended because of the need for lymphadenectomy and careful inspection for invasion/metastases [4]. Cytoreductive surgery should be considered if most of the tumor load is thought to be resectable which may help to reduce the amount of hormones released and potentially extend survival, although this is not proven [26].
13.3 Management of NF-PNENs
13.3.1 Localized NF-PNENs
13.3.1.1 NF-PNETs
Most of PNET are incidentally discovered during imaging follow-up performed for other reasons, also due to the widespread use of high-resolution images [27]. The incidence of PNENs ≤2 cm increased by 710.4% (annual percentage change 12.8%) over the last 22 years [28]. As a consequence many of these tumors have small dimension and most of patients are totally asymptomatic. The incidental diagnosis represents a favorable predictor of overall survival for patients with PNENs. Crippa et al. published a series of 355 patients of which 124 (35%) incidentally diagnosed, and they showed that the 5-year progression-free survival (PFS) was 83% and 32% for incidental and symptomatic NF-PNENs, respectively [27]. Cheema et al. recently demonstrated that progression-free survival rates are significantly higher in patients with incidentally detected lesions [29]. The presence of symptoms occurs usually in patients with larger lesions or in the presence of advanced disease. Patients often present late in their course with symptoms of mass effect or with symptoms related to metastases including abdominal pain, weight loss, and jaundice [30, 31]. The small dimension of the tumor, in association with the incidental finding, is associated with a negligible risk of recurrence after radical surgery [32, 33]. Bettini et al. showed that only 6% of NF-PNENs ≤2 cm have an aggressive behavior after radical surgery when incidentally discovered [32]. The choice to treat these lesions with surgery or conservatively should be balanced with the risks and benefits of the surgery itself. Pancreatic resections are associated with a high risk of morbidity and mortality rate remains around 2% also in high-volume centers [34]. Recently, Ateema et al. published a comparison between resections for PNENs and resections for other lesions in terms of postoperative pancreatic fistula (POPF) rate. They showed that grade B and C POPF [35] have higher incidence after resection for PNENs compared with resection for other lesions (22.7% vs 17.2), and if compared only with PDAC, this difference is highly significant (22.7% vs 9%) [36]. In this setting, considering the less aggressive behavior of asymptomatic NF-PNENs ≤2 cm, conservative management has been proposed for these tumors. Recently, several experiences have demonstrated the safety of an active surveillance for small, asymptomatic PNETs [37, 38]. No disease progression among observed NF-PNEN ≤2 cm was reported in any of the published series, and surgery during follow-up was indicated for 4–20% of patients [37]. However surgery is still the treatment of choice for small NF-PNETs in selected cases. Main reasons for surgery are a rapid tumor size increasing, a dilatation of the MPD, a suspicious lymph node metastases, the presence of a Ki67 >2%, and an excessive anxiety experienced by the patient during follow-up. In these cases, surgery should be tailored on the patients’ characteristics and on the localization of the tumors. Conservative, parenchyma-preserving procedures should be avoided in the presence of suspicious signs for malignancy (i.e., lymph node involvement at imaging or dilatation of the MPD). In the remaining cases, middle pancreatectomy is indicated for small tumors of the pancreatic body, whereas an enucleation should be considered only if the main pancreatic duct can be preserved. The main advantage for atypical resections is the possibility to reduce as much as possible the risk of endocrine and/or exocrine insufficiency compared to standard resections although they are associated with a high rate of pancreatic fistulas [39, 40].
In both enucleation and middle pancreatectomy, a lymphadenectomy is not routinely performed, but a nodal sampling should be always recommended for final histological assessment. Atypical resection should be considered only for small lesions with benign or uncertain behavior. Surgical resections can be performed either open or laparoscopically. Both laparoscopic enucleation and distal pancreatectomy are safe and feasible in patients with PNETs [41].
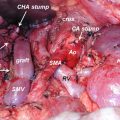
Lesions larger than 2 cm show different behavior: they are associated with a higher risk of malignancy and a poorer disease-free survival. The risk of nodal metastases is also higher and is up to 50% in case of lesions >4 cm [32]. In most series, NF-PNETs >2 cm are usually diagnosed at an advanced stage with 60–85% presenting with synchronous liver metastases [42, 43]. Considering the risk of malignancy all these lesions should be treated with a standard resection and adequate lymphadenectomy. In case of lesions localized in the head of the pancreas, PD is the treatment of choice, whereas in lesions of the body and tail of the pancreas, left pancreatectomy (LP) and splenectomy are indicated.
13.3.1.2 Neuroendocrine Carcinomas (NECs)
Neuroendocrine carcinomas (NECs) are defined as lesions with a mitotic count of >20 mitoses per 10 high-power fields and/or a Ki67 index of >20% (WHO 2010 G3) [44]. Pancreatic NECs are rare (only 2–3% of all PNENs) and are associated with a poor prognosis [45]. Most of patients with NECs are diagnosed at advanced stage with a high rate of nodal metastasis, higher than 90% in some series [46]. Median survival ranges from 11 to 21 months [47]. Curative (R0/R1) resection of pancreatic NEC is associated with improved survival, and in localized and resectable disease, surgical exploration for potentially curative resection should be considered. Resection of primary pancreatic neuroendocrine neoplasms in the presence of not resectable hepatic metastases is still controversial, but considering their poor outcomes, palliative resection of the primary pancreatic NEC in the setting of not resectable liver metastases cannot be recommended [48, 49].
13.3.1.3 MEN1-Associated NF-PNETs
MEN1 is characterized by the combined occurrence of primary hyperparathyroidism, duodeno-pancreatic neuroendocrine neoplasms, and tumors of the anterior pituitary gland. These tumors include nonfunctioning PNETs (NF-PNETs) (30–80%), gastrinomas (50%), and insulinomas (20%). The presence of malignant NF-PNEN represents one of the leading causes of disease-specific death in these patients [50]. Nowadays, the recommendation for surgical resection has been based on tumor size, because of a higher rate of metastases in patients with larger tumors [51]. Tumor size is significantly correlated with the presence of metastases and tumor size >30 mm is associated with a reduction in survival time. Patients with tumors between 11 and 30 mm have a risk of death slightly, but not significantly, higher than patients with tumors <10 mm [15]. Surgery represents the treatment of choice for NF-PNENs >2 cm associated with MEN1 [52]. Many controversies remain in the management of tumors ≤2 cm. No survival benefit is demonstrated for patients with NF-PNENs ≤2 cm who receive surgery compared with patients who had conservative management [53] [54]. PNENs in the context of MEN1 are often multifocal. In this setting, careful microdissection of the pancreas demonstrates multiple, small microadenomas. While only a minority of the microadenomas acquire the potential to grow unrestrictedly, larger lesions may be genetically unstable, develop secondary mutations, and will grow into clinically relevant lesions. Prophylactic surgery aims to remove these lesions before malignancy develops. However, while recent data show that early diagnosis and surgery improve survival [55], others suggest a more conservative approach, as their data indicate that only tumors >2 cm are associated with an increased risk of malignancy [56]. Pancreatic surgery is graved by a high rate of morbidity as well as a high rate of mortality particularly in non-referral centers. In these patients, the texture of the pancreatic remnant is usually soft. As a consequence there is an increased risk of failure for the pancreatic anastomoses or suturing of the resection margins. Thus, pancreatic surgery in patients with MEN1 syndrome is challenging and associated with high risk of postoperative complications.
13.3.2 Metastatic Disease
13.3.2.1 Surgery for Liver Metastases
Liver metastases (LM) develop commonly (up to 95% in some case series) in the natural history of NENs [57]. Hepatic involvement differs between primaries. Gastric, appendiceal, and rectal tumors rarely cause metastases, while pancreatic and small bowel have 28–78% and 67–91% incidence rates, respectively [58]. LM represent a strong prognostic factor, along with histologic differentiation and proliferative activity. Among patients with LM, the origin of the primary tumor influences prognosis. PNENs have the worst prognosis within all metastatic NENs, with 5-year survival rates of 40–60% [59]. Patients with gastrinoma and no metastatic disease have 95% survival at 20 years, while only a 10-year survival of 15% is reported when diffuse metastatic liver disease is present [60]. Most of the published series on the management of metastatic NENs are heterogeneously made from different primaries including gastro-entero-pancreatic and pulmonary NENs. Although most of these tumors share similar characteristics, long-term outcomes can change considerably among different forms. A recent study focused selectively on PNENs with LM and showed improved overall and progression-free survival in patients who underwent radical surgery comparing to those who underwent palliative surgery and those who had nonoperative treatments [61].
The decision to offer liver surgery is based on a multifactorial assessment taking into account tumor grading (only G1-G2 should undergo liver surgery; G3 cancers have overtly high recurrence rates and disseminated disease), the presence of extrahepatic disease, volume of liver remnant, and the presence of symptoms [62]. This latter is often developed with the onset of hepatic metastases, as the result of tumor-secreted hormones reaching the systemic circulation. Only 20–30% of patients with metastatic disease are suitable for radical intent at presentation [63]. Debulking surgery (R2) in incompletely resectable metastatic disease is not universally accepted, but particularly in symptomatic patients, it may improve the quality of life when medical treatment failed [62]. For surgery with curative intent, ENETS have proposed the following criteria: (i) resectable G1-G2 liver disease with acceptable morbidity and less than 5% mortality, (ii) absence of right heart insufficiency, (iii) absence of unresectable lymph node and extra-abdominal metastases, and (iv) absence of diffuse or unresectable peritoneal carcinomatosis [58]. The type of surgical resection depends on patient and liver conditions (i.e., performance status, number and location of hepatic deposits, complexity of the resection, and predicted future liver remnant). NEN LMs have been classified morphologically as type I (single metastasis), type II (isolated metastatic bulk accompanied by smaller deposits), or type III (disseminated metastatic spread) [64]. For otherwise unresectable disease, two-step approaches have been proposed including portal vein embolization and two-stage hepatectomies including associating liver partition to portal vein ligation (ALPPS) [65, 66]. The overall survival after hepatic resection is 46–86% at 5 years and 35–79% at 10 years [58]. In comparison, patients who do not receive resection of liver metastases show a survival rate of only 30–36% [61, 67]. Selection biases due to better performance status or less advanced disease are likely to have influenced such differences in favor of the outcomes associated with surgery. Nevertheless, resection shows low mortality rate (0–5%) and acceptable morbidity (30%). Interestingly, resections with microscopically invaded margins (R1) do not seem to affect the overall survival [68]. Analysis of histopathology specimens revealed that often the disease burden in the liver is underestimated, with almost half the number of LM from neuroendocrine tumors undetectable on preoperative imaging [69]. These results suggest that NEN LM are frequently more extensive than identified, even intraoperatively, and that a real curative R0/R1 resection is difficult to achieve. As a consequence, a high rate of recurrence is reported, after a median time of 16–20 months and the majority of patients experience recurrence at 5 years. Robust studies comparing nonsurgical against surgical treatments are lacking and those available are subject to relevant selection biases [70]. In the last 20 years, nonsurgical novel techniques have become available and gained popularity mainly as complementary treatment options. The lack of randomized data makes the comparison with a surgical approach in terms of survival benefit and symptomatic relief difficult.
13.3.2.2 Surgery of the Primary Tumor
In Locally Advanced PNENs
An aggressive surgical approach for PNENs in selected patients showed a survival benefit in the presence of nearby organ invasion or the invasion of vascular structures for G1-G2 neoplasms. In a recent retrospective analysis, for patients undergoing en bloc resections of adjacent organs, the 5-year DFS was 42% and did not differ from patients undergoing pancreatic resection alone [71]. Conversely, the results with NEC G3 were similar to those of pancreatic adenocarcinoma, and R0 resections did not lead to improved survival rates compared to R1 and R2 resections. However, any type of resection had better outcomes than exploration only [72]. Selected cases seem to benefit from alleviation of symptoms from debulking surgery, mainly as part of multimodal treatment.
In Metastatic Disease
At the time of presentation, 80% of patients have unresectable LMs. For most other malignancies, there is little rationale to resect the primary site when widespread, unresectable metastases are present. However, because a prolonged life expectancy is associated with slowly growing PNETs, resection of the primary tumor may be beneficial if the primary site is causing symptoms and to avoid local complications such as intestinal occlusion, mesenteric retraction, and hemorrhage [61]. Also, resection of the primary tumor allows focusing the treatment on liver metastases including liver transplantation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree