Treatment of childhood hematologic malignancies requires multidisciplinary care and reliable infrastructural support; creating a this structure in resource-poor settings remains challenging. Ideally therapy would be tailored to each region and disease. The development of research initiatives is essential. Acute lymphoblastic leukemia (ALL) and lymphomas are common in low- and middle-income countries; treatment is often resource intense but likely cost effective. Outcomes currently are worse than those reported in high-income countries. Chronic myeloid leukemia can be treated effectively with imatinib. Strategies to decrease the burden of therapy and robust palliative care programs are essential for optimal treatment of all afflicted children.
Key points
- •
Pediatric hematologic malignancies are challenging to treat in low- and middle-resource settings owing to the complex, multidisciplinary, and longitudinal care required.
- •
Although outcomes are generally inferior to those reported by high-income countries, progress has been achieved particularly for acute lymphoblastic leukemia, Hodgkin lymphoma, and Burkitt lymphoma (BL).
- •
Capacity building to improve care includes pathology expertise, advances in supportive care and family support systems, and accessibility of palliative care.
- •
Developing an infrastructures that allows for collection of reliable data and supports clinical research is an essential component of strategies to improve outcomes for children globally.
Global approach to pediatric hematologic malignancies
The treatment of childhood cancer requires complex, longitudinal, multidisciplinary care delivered by a dedicated team of providers in addition to reliable infrastructural support. There is marked variability in the intensity and duration of therapy as well as in the multidisciplinary expertise needed for the treatment of solid tumors in comparison with hematologic malignancies and also within different types of hematologic malignancies. As a result, creating a structure that can provide effective and safe therapy for this group of childhood diseases in resource-poor settings remains challenging. Therapy, ideally, would be tailored to the region, country, and specific medical center to ensure optimal matching of therapy intensity and resources. As an example, Hunger and colleagues suggested a tiered hierarchy with treatments of increasing intensity for acute lymphoblastic leukemia (ALL); a program would move to the next higher level of therapy once treatment-related mortality had been demonstrated to be acceptable at the current level. Another approach was taken in Asia, where a national summit meeting in 2013 was convened to generated guidelines for care delivery in both pediatric and adult ALL. Recommendations concerning diagnosis, risk stratification, and supportive care measures were made and a model was proposed that intensified therapy based on both disease factors and the resource level of the treating facility. Guidelines for essential supportive care provisions have been generated by the International Society of Pediatric Oncology and recommend hand washing hygiene, nutritional assessment and support, access to pain medications and antiemetics, as well as suggested therapy for febrile neutropenia.
Palliative care should be a component of all programs offering treatment to children with cancer and ideally programs would use a multifaceted approach of government-supported policy, education, and accessibility to pain medications and have a focus on home-based care. Unfortunately, of the 192 member countries of the United Nations, almost two-thirds have no reported programs in pediatric palliative care ; in Africa, analysis of peer-reviewed and non–peer-reviewed literature found that fewer than 20% of 53 countries had any resources for pediatric palliative care identified. It is crucial that initiatives in this arena are developed in parallel with advances in the scope and intensity of available oncologic therapies. There are sparse data on either the cost or cost effectiveness of treating childhood hematologic malignancies. In China it was estimated that it cost 11,000 USD per child treated for ALL. The cost per patient treated was estimated to be 17,000 USD for ALL in Brazil and 50 USD for BL treated in Malawi; both met criteria for cost effectiveness according to the standard World Health Organization (WHO) definition of ratio of cost to disability-adjusted life-years prevented. It would be enormously helpful to have similar data across the spectrum of low- and middle-income countries (LMICs).
Undertaking quality research is an essential exercise, not a luxury, in LMICs, in which resources by definition are limited. Understandably, priorities are in the areas of health services and outcomes, with “scaling up” of research a necessary goal. Particular challenges in conducting research in LMICs have been described.
The importance of good data acquisition and management cannot be overemphasized; with proper training and a well-defined career trajectory as a priority. Such investment has borne sound return, as exemplified by an audit of data quality in Honduras. More recently, building on this foundation, regional pediatric cancer registries have been in operation in Central America since 2013. It will be impossible to design appropriate treatment strategies for children from LMICs without robust data reporting on outcomes and toxicities.
Global approach to pediatric hematologic malignancies
The treatment of childhood cancer requires complex, longitudinal, multidisciplinary care delivered by a dedicated team of providers in addition to reliable infrastructural support. There is marked variability in the intensity and duration of therapy as well as in the multidisciplinary expertise needed for the treatment of solid tumors in comparison with hematologic malignancies and also within different types of hematologic malignancies. As a result, creating a structure that can provide effective and safe therapy for this group of childhood diseases in resource-poor settings remains challenging. Therapy, ideally, would be tailored to the region, country, and specific medical center to ensure optimal matching of therapy intensity and resources. As an example, Hunger and colleagues suggested a tiered hierarchy with treatments of increasing intensity for acute lymphoblastic leukemia (ALL); a program would move to the next higher level of therapy once treatment-related mortality had been demonstrated to be acceptable at the current level. Another approach was taken in Asia, where a national summit meeting in 2013 was convened to generated guidelines for care delivery in both pediatric and adult ALL. Recommendations concerning diagnosis, risk stratification, and supportive care measures were made and a model was proposed that intensified therapy based on both disease factors and the resource level of the treating facility. Guidelines for essential supportive care provisions have been generated by the International Society of Pediatric Oncology and recommend hand washing hygiene, nutritional assessment and support, access to pain medications and antiemetics, as well as suggested therapy for febrile neutropenia.
Palliative care should be a component of all programs offering treatment to children with cancer and ideally programs would use a multifaceted approach of government-supported policy, education, and accessibility to pain medications and have a focus on home-based care. Unfortunately, of the 192 member countries of the United Nations, almost two-thirds have no reported programs in pediatric palliative care ; in Africa, analysis of peer-reviewed and non–peer-reviewed literature found that fewer than 20% of 53 countries had any resources for pediatric palliative care identified. It is crucial that initiatives in this arena are developed in parallel with advances in the scope and intensity of available oncologic therapies. There are sparse data on either the cost or cost effectiveness of treating childhood hematologic malignancies. In China it was estimated that it cost 11,000 USD per child treated for ALL. The cost per patient treated was estimated to be 17,000 USD for ALL in Brazil and 50 USD for BL treated in Malawi; both met criteria for cost effectiveness according to the standard World Health Organization (WHO) definition of ratio of cost to disability-adjusted life-years prevented. It would be enormously helpful to have similar data across the spectrum of low- and middle-income countries (LMICs).
Undertaking quality research is an essential exercise, not a luxury, in LMICs, in which resources by definition are limited. Understandably, priorities are in the areas of health services and outcomes, with “scaling up” of research a necessary goal. Particular challenges in conducting research in LMICs have been described.
The importance of good data acquisition and management cannot be overemphasized; with proper training and a well-defined career trajectory as a priority. Such investment has borne sound return, as exemplified by an audit of data quality in Honduras. More recently, building on this foundation, regional pediatric cancer registries have been in operation in Central America since 2013. It will be impossible to design appropriate treatment strategies for children from LMICs without robust data reporting on outcomes and toxicities.
The role of essential medicines
The high cost of drugs overall, and the marked disparities among LMICs and even within individual countries, is an enormous barrier to care. Bulk purchasing provides some relief and it is worthy of note that the Pan-American Health Organization Strategic Fund includes important drugs for noncommunicable diseases, including cancers in children. It has been estimated that the annual cost of all medicines for the treatment of incident cases of ALL in children in LMICs is less than US$150 million. Arguably the biggest challenge to improving the care of children with cancer in LMICs is access to affordable, safe, and effective chemotherapy. At the World Health Assembly in 2014, Resolution 67.22 requested that the WHO “support members states in sharing best practices in the selection of essential medicines and in developing processes for the selection of medicines for national essential medicines lists.” The WHO had established a Model List of Essential Medicines in 1977 and created a separate list (EMLc) for children in 2007. These lists are reviewed by an Expert Committee every 2 years and are used by national governments to guide drug procurement.
In 2011, using a disease-based approach, the Expert Committee endorsed the inclusion in the List of Essential Medicines for children for the treatment of ALL, BL, and Wilms tumor; these diseases were selected as priorities based on incidence and curability. This prompted the International Society of Pediatric Oncology’s Working Group on Essential Medicines to propose a more comprehensive list of drugs that served as a basis for recommendations to the Expert Committee for additions to the original list. The committee accepted all of these and 6 more cytotoxic agents were added in May 2015 to the List of Essential Medicines for children for the treatment of 6 more diseases, including Hodgkin lymphoma ( Table 1 ). Further additions will be limited to steps 1 and 2 of the 5-level step ladder approach to the selection of essential medicines; that is, those used in common regimens for all children with a given disease and those used additionally for high-risk patients. Decision makers continue to wrestle with the balance between magnitude of clinical benefit and cost effectiveness. Aiming to provide policymakers with evidence for deciding on interventions and programs that maximize health for the available resources, WHO has developed the WHO-CHOICE tool ( CHO osing I nterventions that are C ost- E ffective).
| Disease | Medicine |
|---|---|
| Acute lymphoblastic leukemia | Asparaginase Cyclophosphamide Cytarabine Daunorubicin Dexamethasone Doxorubicin Etoposide Hydrocortisone Mercaptopurine Methotrexate Methylprednisolone Prednisolone Thioguanine Vincristine |
| Wilms tumor | Dactinomycin Doxorubicin Vincristine |
| Burkitt lymphoma | Cyclophosphamide Cytarabine Doxorubicin Etoposide Prednisolone Vincristine |
| Adjuvant medicines | Allopurinol Mesna |
| Ewing sarcoma | Cyclophosphamide Doxorubicin Etoposide Ifosfamide and mesna Vincristine |
| Hodgkin lymphoma | Cyclophosphamide Dacarbazine Doxorubicin Etoposide Prednisolone Vincristine |
Building capacity
The vehicle most commonly associated with capacity building is twinning: establishing a sustainable program of cooperation between 1 or more institutions in an LMIC and partners in a high income country. The first example seems to have been an association that began almost 30 years ago between the Pediatric Clinic of the University of Milano-Bicocca in Monza, Italy, and Manuel de Jesus, ‘La Mascota,’ Hospital in Managua, Nicaragua. This experience led to the establishment at the Monza International School of Pediatric Hematology Oncology that in turn spawned multiple twinning programs between children’s hospitals in Italy and partner institutions in Central and South America. These endeavors contributed to the formation of regional groups that have sustained and expanded the building of capacity, namely, Asociación de Hemato-Oncología Pediátrica de Centro América in Central America and GALOP (Latin American Pediatric Oncology Group) in South America, the latter having a strong association with the US-based Children’s Oncology Group. The sharing of resources within institutions in LMICs represents a different version of twinning, as in the use of flow cytometry serving several countries in Central America. Recent initiatives have also developed North–South links and oncology facilities in Africa, for example, in Rwanda ( Fig. 1 ). These developments are not only cost effective, but provide a basis and stimulus for mutual advancement and shared research opportunities.
Fundamental to the success of twinning is a strong focus on education. This was the primary purpose of Monza International School of Pediatric Hematology Oncology and is the basis of programs in Singapore, Marrakesh, and Guatemala City, among others. Initially, such programs were limited to physicians, but important and measurable educational advances have also taken place for nurses, clinical pharmacists, and data managers.
Acute Lymphoblastic Leukemia
Incidence
ALL is the most common hematologic malignancy of childhood. The majority of incidence data are generated by high-income countries (HICs); in the United States, there are approximately 42 cases of ALL per 1 million children. However, less than 15% of the population in Africa and Southeast Asia is captured by established cancer registries and it is thus very difficult to know if these numbers are accurate on a global scale. Historically, the incidence has seemed to be lower in less-developed countries with a mean annual incidence of 16.5 cases per million population. However, the incidence does seem to be steadily increasing at a greater rate than in HICs, likely owing to a combination of improved awareness, better reporting, and decreases in other contributors to childhood mortality.
Treatment and outcomes
ALL can be cured in almost 90% of children in HICs using multiagent systemic and intrathecal chemotherapy for a total duration of therapy of 2 to 3 years. Induction, the first phase of treatment, consists of more intensive therapy and patients often require prolonged hospitalization and systemic antimicrobials. Repeat examination of the marrow occurs at the end of induction to assess for early response and provide intensification of therapy in patients not in remission. High-risk patients receive a second induction course and a minority of children, primarily those with central nervous system involvement, will require cranial radiation therapy. Maintenance therapy is of much less intensity and occurs primarily in the outpatient setting. However, the care remains complex. Maintenance involves a rotating combination of oral, intravenous, and possibly intramuscular drugs, of which some are administered daily, some weekly, and some monthly. Repetitive visits to the cancer center are required.
Approaches to treatment and outcome have been quite variable in the LMIC setting; in general, as the intensity of therapy increases the number of relapses has decreased, but treatment-related mortality has increased. Thus, attempts have been made to match therapy intensity to the level of supportive care available, as well as to use risk stratification to deliver the most intense therapy to the patients with the worst prognosis based on presenting features and early response to therapy. All approaches have used an induction phase and a maintenance phase with intermittent intrathecal chemotherapy administration.
Given that there are still reported differences in outcomes related to disparities in socioeconomic status in HICs, the challenges of improving outcomes in the LMICs is enormous. There is, unsurprisingly, a wide range reported for disease-free survival (DFS), from as low as 15% to greater than 60%, depending on the patient population and resources available. Standard factors used for risk stratification—namely, age, initial white blood count, and prednisone response—have been assumed to apply globally, although a large study from India found that age had no impact on outcome and that risk factors were center specific even with the use of one standardized protocol within 1 country. There are many potential factors contributing to inferior survival with some more amenable to intervention than others:
- 1.
Innate biological differences: TEL-AML1 is the most common acquired genetic abnormality in pediatric B precursor ALL, occurring in 20% to 30% of patients in the United States. Patients harboring this transcript are known to have an improved DFS. Although the impact on prognosis seems to be immutable, the proportion of TEL-AML1–positive patients may vary by region and occur less frequently in some areas of the world, such as south Asia. Similarly, a higher percentage of patients are reported to have T-cell versus precursor B ALL in Egypt and rural India. This biologic variability results in an increased incidence of high-risk features in some populations and thus would contribute to poorer outcomes for the group as a whole.
- 2.
Delay in diagnosis: Delay between development of symptoms and initiation of therapy can impact survival from solid tumors at risk for metastasis. This may not be as problematic in hematologic malignancies, which are systemic at the time of presentation. In addition ALL may be recognized and therapy sought more quickly than in other childhood malignancies such as Hodgkin lymphoma (HL), even in resource-poor settings. A separate issue is that some children with ALL may receive pretreatment with steroids for symptoms thought to reflect other diagnoses, such as arthritis, idiopathic thrombocytopenic purpura, or simply failure to thrive. Monotherapy with prednisone could negatively impact DFS owing the development of steroid-resistant clones before the initiation of ALL-directed therapy.
- 3.
Undernutrition is prevalent among children in LMICs, and especially so in children with cancer at diagnosis. In a large sample in Central America approximately two-thirds of such children were classified as severely malnourished and had a notably lower survival than those who were not so deprived nutritionally. However. It was demonstrated subsequently, in a cohort with ALL in Guatemala, that restoration of normal nutritional status within 6 months of the initiation of treatment was associated with a survival rate similar to that in children who had maintained a normal nutritional status throughout.
- 4.
Inadequate supportive care measures: In the United States, treatment-related mortality is less than 5% in children with ALL. This number is significantly higher in resource-poor settings and can account for up to one-fourth of deaths. The main causes of mortality are infection and bleeding. Provision of better antibiotic therapy and more rapid access to transfusion support are thus needed. However, improved education of providers, written supportive care guidelines, and the identification and treatment of malnutrition and concurrent infection may also decrease the proportion of deaths owing to treatment-related complications.
- 5.
Delays in therapy: There are many reasons for delays in therapy, including missed appointments, patient-specific medical complications (fever, prolonged neutropenia), and drug unavailability. One study of ALL in Colombia found that delays between starting induction and beginning maintenance therapy (a 24-week period according to protocol), regardless of whether owing to medical issues or other reasons, was associated with a significantly inferior DFS.
- 6.
Abandonment: There have been many attempts to address the intertwined issues of refusal (refusing treatment), noncompliance (lack of cooperation with recommended therapy), and abandonment (termination of therapy prematurely). Key components of successful intervention strategies include family education about therapy duration, side effects, and the potential curability of cancer in addition to increased social support systems including housing, transportation, and stipends to cover loss of income.
Core resources required to treat acute lymphoblastic leukemia in low- and middle-income countries
- •
Adequate pathology capacity that allows for rapid diagnosis, as well as determination of immunophenotype (B- vs T-cell disease) and other features necessary for risk stratification at diagnosis and at the end of induction therapy.
- •
Access to a safe and reliable supply of red cells and platelets for transfusional support, particularly during induction.
- •
Ability to adequately diagnose and treat bacterial, fungal, and viral infections during periods of prolonged neutropenia.
- •
Adequate family supports (transportation, outpatient housing near the hospital, community health worker involvement) so that maintenance chemotherapy can be administered consistently.
Future directions
Changes in care delivery
Safety initiatives: The delivery of oncologic care is a complex, high-risk, multidisciplinary endeavor. In LMICs, there are often no systems in place to support this type of care delivery. Standardization of protocols and supportive care interventions can help prevent errors across centers and providers. A safety checklist has been shown to decrease surgical morbidity and mortality in a diverse group of hospitals around the world. A similar approach could be particularly effective in the oncology setting where teamwork is similarly critical to improving outcomes.
Risk stratification: Much of the progress in ALL in HICs has been the result of adjusting the intensity of therapy based on prognostic factors determined at the time of presentation (age, initial white cell blood count, for example) or based on response to induction therapy. Ideally, patients determined to be at the lowest risk of treatment failure could receive therapy that is not only less intense, but also of shorter duration given the hardships of protracted frequent care in LMICs. However, a recent Japanese study showed that shortening the duration of maintenance therapy from 2 years to 6 months decreased DFS in standard risk ALL patients despite the addition of early intensification and thus any truncation of therapy would need to be studied carefully before being implemented. To successfully treat patients who are designated as high risk, a broader array of chemotherapeutic agents, radiation therapy, and more advanced supportive care needs to be available than currently exists in the majority of LMICs.
Minimal residual disease assessment: Failure to attain morphologic remission (<5% lymphoblasts in the marrow) is known to confer a poor prognosis but the presence of even minimal residual disease has been shown to be important as well. One interesting approach that may be applicable to middle income countries is the use of a simplified flow cytometry technique using a 4 marker assay for minimal residual disease detection. This would allow a broader definition of poor initial response and allow for appropriate upstaging of therapy.
Improved parent/child support systems
Parental and patient education regarding the importance of consistent delivery of outpatient medication and excellent compliance with medical visits will be crucial to improving outcomes in ALL. Advances in this area are challenging to operationalize and it is difficult to identify which interventions have a positive impact, given the many variables affecting DFS. A study in Indonesia where mothers of children with ALL were assigned randomly to receive a journal in which future appointments and medication times were outlined resulted in improved compliance in families from higher socioeconomic strata, but had no effect on outcome in the poorest families. Use of an educational video in Indonesia, however, decreased treatment refusal and increased DFS in the poorest families, highlighting the necessity of tailored approaches depending on the target audience.
Acute Myelogenous Leukemia
Incidence
Acute myelogenous leukemia (AML) accounts for approximately 15% of acute pediatric leukemia in HICs. In comparison with ALL, there seems to be no difference in the incidence between HICs and LMICs.
Treatment and outcomes
There is much less published data on treating AML versus ALL in LMICs. Compared with ALL, therapy is of much shorter duration but of correspondingly greater intensity. The overall duration of therapy is 4 to 6 months, and the majority of that time is spent in the hospital receiving systemic and intrathecal chemotherapy and intensive blood product and antimicrobial support and use of granulocyte colony-stimulating factor is routine. Radiation therapy is not used routinely. Reports are scarce from LMIC settings, although it seems that between 0% and 40% of children are long-term survivors. Treatment related deaths are reported to occur in more than 20% of patients, reflecting the problems encountered in HICs before the routine use of antimicrobial and antifungal prophylaxis. Predicting those at greatest risk of treatment-related mortality remains problematic, although it is assumed that comorbidities such as malnutrition are important and this remains an area requiring more investigation. Bone marrow transplantation is the therapy of choice for refractory or recurrent AML in HICs; in the resource-limited setting, treatment may be best directed toward palliation. Children with late relapses (>18 months from diagnosis) are a possible exception because they can experience a prolonged period of remission with salvage chemotherapy; cure, however, remains very unlikely.
Core resources required to treat acute myelogenous leukemia in low- and middle-income countries
- •
Adequate pathology capacity that allows for rapid diagnosis, as well as identification of other features (FLT3 positivity, monosomy 7) necessary for risk stratification at diagnosis and at the end of induction therapy.
- •
Ability to manage leukostasis, bleeding, and tumor lysis syndrome that can occur at presentation and during induction therapy.
- •
Access to a safe and reliable supply of red cells and platelets for transfusional support.
- •
Availability of growth factors as well as broad spectrum antimicrobials for prophylaxis and treatment of infection with Gram-positive organisms and fungus.
Chronic Myelogenous Leukemia
The incidence of chronic myelogenous leukemia (CML) is relatively rare in children, accounting for less than 5% of pediatric leukemias. For the vast majority of patients who present in chronic phase, daily and likely life-long therapy with the oral tyrosine kinase inhibitor (TKI) imatinib (Gleevac) can provide normalization of blood counts and very good quality of life with tolerable side effects, although younger patients seem to experience both more medical and emotional consequences of therapy. This treatment is expensive, however, with a 1-year supply costing almost 100,000 USD. In many resource-restricted countries, imatinib is provided free of charge through the Glivac International Patient Assistance Program. Access to medication requires only physician oversight and confirmation of the diagnosis of CML; the latter is most commonly accomplished through molecular testing for the presence of the bcr-abl protein product arising from translocation between chromosomes 9 and 11. Testing can be done relatively easily, even in low-resource settings, using an automated technology initially developed to test for multidrug-resistant tuberculosis and yields results comparable with the polymerase chain reaction testing done in HICs. There are minimal data on outcomes using imatinib in LMICs. The most extensive experience is in 3188 pediatric patients with CML treated through the Glivac International Patient Assistance Program. Outcomes are comparable with those reported in the United States with a 3-year overall survival of almost 90%. Increased time between diagnosis and commencement of imatinib therapy was associated with an increased risk of death. However, the frequency of acquisition of mutations leading to imatinib resistance is not known and this is of particular concern in children who will require decades of therapy. The biggest challenge—regardless of resource level—is ensuring continued compliance with a daily medication in patients often having no obvious signs of illness. A recent study in the United States identified medication noncompliance as the most important contributor to imatinib failure. Use of a community health worker model as first described with antiretroviral therapy may be a useful approach to this pervasive issue. If drug resistance does develop, few LMICs have access to second- and third-generation TKI or stem cell transplantation for salvage therapy.
Future directions
Standard therapy for CML treated with TKIs involves routine assessment of quantitative levels of bcr-abl from the peripheral blood throughout the course of treatment. Patients who have evidence of early disease progression are switched to another TKI. Currently, few countries have the infrastructure to monitor patients consistently in this fashion and even fewer have access to the expensive subsequent generation TKIs.
Hodgkin Lymphoma
Incidence
HL seems to occur more commonly in LMICs perhaps owing to the high incidence of Epstein–Barr virus (EBV) infection in the population. Latent EBV can be found in Reed–Sternberg cells, the malignant cell type in HL, in 50% of patients in LMICs, although it does not seem to impact on prognosis. HL also occurs at a younger age in this setting with a peak incidence of 5 to 9 years, which also may be related to the role of EBV infection in this disease.
Treatment and outcome
Accurate staging is critical because it directs both the components and duration of therapy. Evaluation of chest, neck, abdomen and pelvis with computed tomography is the minimum assessment needed. It remains difficult to distinguish normal from pathologic nodes without functional imaging such as F-labeled 2-deoxyglucose PET. This imaging modality is rarely available in resource-poor settings and as a result patients are at risk for being assigned a stage that is either higher or lower than that reflected by the actual burden of disease. Most children present with stage III or IV disease in LMICs. Treatment has been adapted from HICs and most often involves 4 to 6 cycles of combined chemotherapy that can usually be administered in the outpatient setting. Most approaches include radiation therapy to sites of previous disease. Radiation almost always occurs at a different facility and often in a different city or country. Difficulties in coordination of care across settings is always a challenge and can negatively impact outcome as a result of many factors, including treatment delays, loss of disease control, and abandonment of therapy. However, in general, HL is a very treatable malignancy and using a variety of standard published approaches reported DFS is between 60% and 90%, in many settings approaching that reported in HICs.
Non-Hodgkin Lymphoma
The non-Hodgkin lymphomas include lymphoblastic lymphoma, BL, and large cell lymphoma.
Incidence
Lymphoblastic lymphoma can be of either a pre-B or T-cell phenotype and is treated identically to ALL.
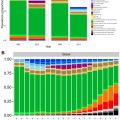
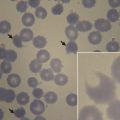
BL is the most common subtype of pediatric non-Hodgkin lymphoma and is particularly prevalent in sub-Saharan Africa, where it accounts for almost 50% of all childhood cancers. This is thought to be related to endemic EBV infection because more than 90% of cases contain the ebv genome in tumor tissue. Malaria transmission may be an additional factor. T-cell control of EBV is impaired during attacks of malaria and Plasmodium falciparum may also interact directly with B-cell receptors stimulating proliferation of EBV-infected lymphocytes. The incidence varies by region but can be as high as 22 per 100,000 children and account for up to 70% of all new childhood cancers in parts of Tanzania. It does not seem that human immunodeficiency virus has made an impact on the incidence of the disease, although patients with BL coinfected with human immunodeficiency virus seem to have a worse survival. In the African setting, the disease presents most often as a jaw mass, although a recent report suggests that obtaining abdominal ultrasound in addition to a physical examination improves staging accuracy and the incidence of abdominal involvement then becomes similar to that in HIC. The incidence of B-cell large cell lymphoma is not described in LMICs and can be difficult to distinguish clinically and pathologically from BL; these patients can be treated effectively on BL protocols.
Treatment and outcomes
In HICs, B-cell lymphomas can be cured in 90% of children but therapy is very myelosuppressive and requires a prolonged hospital stay and availability of a broad range of antimicrobial agents. Historically, oral cytoxan (cyclophosphamide) alone has been reported to cure a small number of cases of BL and low-dose combination chemotherapy regimens up to one-third of children. Currently in LMICs, risk stratification has improved survival to greater than 50%. The least intense approach for those with low risk disease, as assessed by stage and clinical response to initial therapy, consists only of cytoxan and intrathecal (IT) therapy. Intravenous methotrexate is added for higher risk patients and total duration of therapy is less than 3 months for all groups. Unfortunately, the time to diagnosis is often delayed in resource-poor settings, particularly when children present with findings such as cervical adenopathy, which usually reflects a benign self-limited process. Thus, the vast majority present with nonlocalized disease and require the more aggressive regimen. A consortium of 8 African countries have adopted modified protocols used in HIC by lowering the dosages of drugs most associated with profound myelosuppression. This resulted in an overall survival of 84%, including a 76% overall survival for stage II patients. Of import, treatment-related mortality decreased by 50% (from 26% to 12%) over the 3-year study period, likely related to quality improvement initiatives including regular meetings and review of adverse events. Relapsed/resistant disease remains problematic, although in a small series of patients, retreatment with cytoxan and IT therapy and the addition of vincristine provided disease control in more than one-third of those treated. Patients whose relapse occurred after more than 6 months off therapy and who presented with limited disease were most likely to respond.
Core resources required to treat B-cell lymphoma in low- and middle income countries
Management of tumor lysis syndrome: Tumor lysis syndrome is a frequent problem in patients with advanced stage BL and can lead to severe electrolyte abnormalities, renal failure, and death. Frequent clinical and laboratory monitoring is essential but difficult to ensure in the setting of limited staffing. The use of allopurinol, intravenous hydration, and involvement of caretakers in monitoring urine output has been suggested as a feasible approach to the management of this complication.
Future directions
Improvements in supportive care are key to better survival. Currently almost one-third of those on protocols of moderate intensity succumb to treatment related complications. As in AML, broad spectrum antibiotics and antifungal drugs must be available in addition to growth factor support.
Rituximab, a monoclonal antibody directed against the CD20 antigen found on mature B cells, has been incorporated into many B-cell lymphoma regimens in HICs. It has been shown repeatedly to improve survival in adults but definitive evidence assessing its role in pediatric B-cell lymphomas is lacking. It is expensive and requires close monitoring during administration but may allow for incremental improvement in DFS when combined with the less intense regimens often used in LMICs for these diseases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree