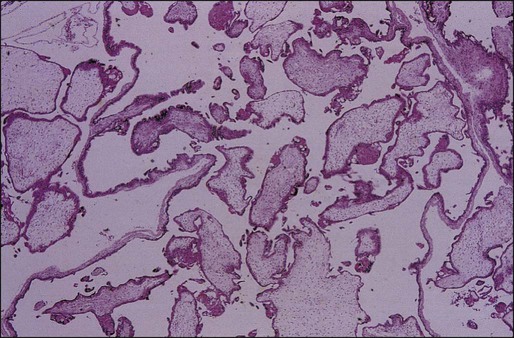
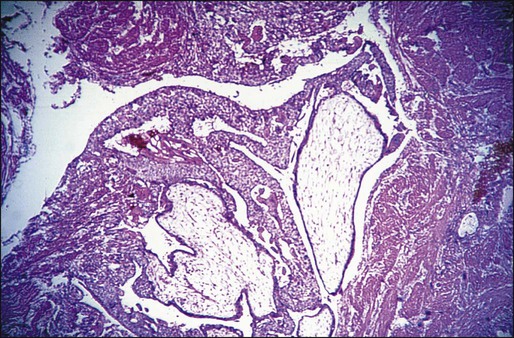
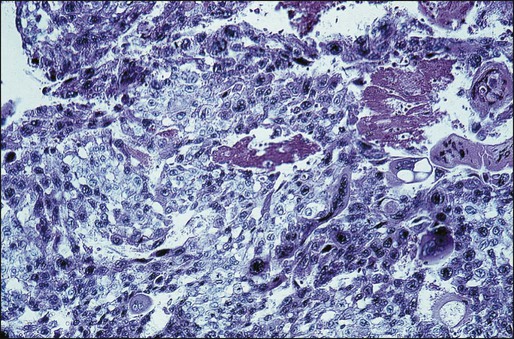
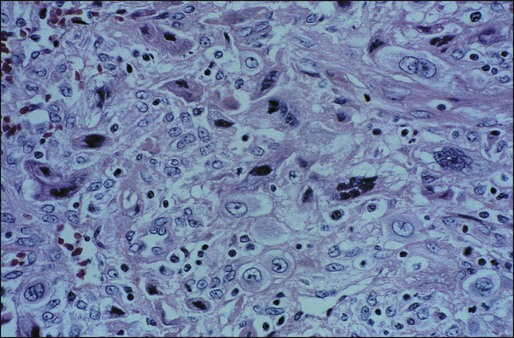
Donald Peter Goldstein and Ross Stuart Berkowitz • The incidence of complete hydatidiform mole is approximately 1 in 1200 pregnancies in the United States. • The incidence of partial hydatidiform mole is approximately 1 in 650 pregnancies. • Repeat moles occur in approximately 1 in 125 pregnancies, and third moles occur in approximately 1 in 5 pregnancies. • Complete hydatidiform mole is usually due to an androgenetic diploid conception, in which a haploid sperm fertilizes an egg that lacks female chromosomes. • A partial hydatidiform mole develops when dispermy occurs, and the resulting conceptus is triploid. • Earlier diagnosis of complete hydatidiform mole due to improved ultrasound and human chorionic gonadotropin (hCG) assays has made the pathological diagnosis of complete hydatidiform mole more difficult because of its resemblance to partial hydatidiform mole and nonmolar abortions. • Hydatidiform mole is characterized by hydropic villi with trophoblastic hyperplasia. • Invasive mole is characterized by invasion of myometrium by hydropic villi surrounded by hyperplastic trophoblasts. • Choriocarcinoma is characterized by sheets of neoplastic cytotrophoblasts and syncytiotrophoblasts invading tissue and is associated with necrosis and hemorrhage. Hematogenous spread occurs early. • Placental site and epithelioid trophoblastic tumors are rare forms of choriocarcinoma made up of mononuclear cells from intermediate trophoblast at the implantation site that invade the myometrium. Both placental site and epithelioid trophoblastic tumors metastasize late and are relatively resistant to chemotherapy. • Hydatidiform mole commonly presents in the first trimester with vaginal bleeding. • Complete hydatidiform mole is usually diagnosed by ultrasound because of the abnormal appearance of the placenta and the absence of a fetus. • Partial hydatidiform mole can be difficult to diagnose by ultrasound and is usually confirmed pathologically. • Persistent postmolar gestational trophoblastic neoplasia is usually nonmetastatic and is characterized by a rising hCG level and persistent bleeding due to residual molar tissue. • Metastatic postmolar gestational trophoblastic neoplasia (GTN) usually involves the lungs and, rarely, the brain, liver, and other distant sites. • The diagnosis of gestational trophoblastic neoplasia after a miscarriage or term pregnancy is frequently delayed and commonly presents with significant disease. • The 2002 International Federation of Gynecologists and Obstetricians Staging System combines an anatomic description of the disease (i.e., stages I, II, III, and IV) with a prognostic scoring system. • Single-agent therapy is usually curative in patients with stage I, II, and III disease who have low prognostic scores (<7). There is evidence that patients with low-risk GTN (scores of 5 and 6) but a large tumor burden (hCG >100,000 mIU/mL) commonly require multiagent chemotherapy to achieve cure. • Patients with stage II, III, and IV disease who have high-risk scores (≥7) require combination chemotherapy for optimal outcome. • Survival rates of 100% in patients with stage I, II, and III disease and 80% in patients with stage IV disease should be achieved. • Response to therapy and remission are determined by hCG levels, which should be tested weekly during chemotherapy. • Patients with high-risk disease should be treated with three or four consolidation courses after the hCG titer normalizes. • Toxicity from the chemotherapeutic agents is the most common early complication. • Other complications relate to the disease and are usually due to internal bleeding. • Most women are cured, are able to achieve subsequent pregnancy, and are able to return to normal activity soon after attaining a normal hCG titer. • It elaborates a reliable and specific tumor marker, human chorionic gonadotropin (hCG). • It is exquisitely sensitive to chemotherapy. • It has a unique immunobiological relationship with its host, because it arises from fetal rather than maternal tissue. Several histologically distinct entities make up GTD: • Hydatidiform mole: partial (PHM) and complete (CHM) • Persistent or invasive gestational trophoblastic neoplasia (GTN) • Placental site trophoblastic tumor (PSTT) An important milestone in the history of GTD occurred in 1928, when Ascheim and Zondek first described a reliable pregnancy test, which became the basis for the early measurements of hCG. In 1963, MacVicor and Donald first used ultrasound in the diagnosis of molar pregnancy. In 1977, Kajii and Ohama1 elucidated the androgenetic origin of hydatidiform moles. Finally, in 1978, Szulman and Surti2 described the genetic basis for PHM as a triploid gestation. Prior to the introduction of chemotherapy, survival with GTN remained limited and precarious because the only form of treatment consisted of hysterectomy or local excision of metastatic sites where possible. In 1959, Brewer3 reviewed survival with CCA at the Albert Mathieu Chorioepithelioma Registry at Northwestern University. Only 6 of 103 patients with metastatic CCA were free of disease at 5 years after their diagnosis. Brewer’s group also analyzed the 5-year survival rates in patients with nonmetastatic CCA treated by hysterectomy. Only 29 of 70 patients (41%) with presumably localized tumor survived, despite prompt hysterectomy. Metastases developed in the remaining patients after the operative procedure and they died of widely disseminated disease. A new era in the management of GTN was inaugurated in 1956, when Li and colleagues4 reported the complete regression of metastatic CCA in three women treated with methotrexate. In 1961, Hertz and coworkers5 reported the initial 5-year experience with chemotherapy for metastatic GTN at the National Cancer Institute. Complete remission was achieved with methotrexate in 28 of 63 (47%) patients with metastatic disease. After obtaining dramatic results with chemotherapy in disseminated disease, Hertz and associates6 successfully used chemotherapy for patients with nonmetastatic tumors. It soon became apparent that certain patients with metastatic GTN became resistant to single-agent chemotherapy and experienced a high mortality rate. In 1965, Ross and colleagues7 reported that delay in diagnosis, high hCG levels, and liver and/or brain metastases predisposed patients to a high risk of drug resistance. The subsequent introduction of multiagent chemotherapy for these patients has resulted in substantial improvement in survival. The incidence and etiologic risk factors that contribute to the development of GTD have been difficult to characterize because of problems in accumulating reliable data, bias, and interpretation and differing methods of expressing incidence in terms of hospital-based versus population-based data. Despite these problems, there are sufficient data to indicate that there are wide regional variations in the incidence of CHM. Estimates from North America, Australia, New Zealand and Europe have shown the incidence of CHM to range from 0.57 to 1.1 per 1000 pregnancies, whereas studies from Southeast Asia and Japan report an incidence approaching 2.0 per 1000 pregnancies.8–12 The incidence of hydatidiform mole in Taiwan is reported to be one in 125 pregnancies.9 In Ireland, the incidence of CHM and PHM has been determined to be 1 in 1945 and 1 in 695 pregnancies, respectively.13 In the United States, molar pregnancy is encountered in 1 in 600 therapeutic abortions and in 1 in 1000 pregnancies. There are data that show an increased incidence of CHM among American Indians, Eskimos, Hispanics, and African Americans.14,15 There is no conclusive evidence that genetic traits, cultural factors, or differences in reporting account for this increase. The etiologic factors that have been linked to the development of CHM are advanced maternal age (>40 years) and prior molar pregnancy.16,17 Familial clusters of biparental CHM have been associated with the NLRP7 gene mutation on chromosome 19q.18 In addition, well-documented nutritional studies have shown an inverse relationship between beta-carotene and animal dietary fat intake and the incidence of CHM.19,20 In this regard, it is of interest that the documented decrease in the incidence of CHM in South Korea has been associated with a gradual Westernization of the Korean diet.21 The epidemiological features of CHM and PHM differ markedly. Parazzini and coworkers16 reported that the risk for partial mole was not associated with maternal age. Additionally, the risk for partial mole has been reported to be associated with the use of oral contraceptives and a history of irregular menstruation but not with dietary factors.22 Therefore, the risk of partial mole appears to be associated with reproductive history rather than dietary factors.23 The overall incidence of invasive mole (IM) has been estimated at 1 in 15,000 pregnancies. Approximately 15% to 29% of hydatidiform moles will result in invasive mole.9 Determining the incidence rate of CCA is even more problematic because of the rarity of this condition and the difficulty in clinically distinguishing postmolar CCA from metastatic mole. In Europe and North America, CCA affects approximately 1 per 40,000 pregnancies, whereas in Southeast Asia and Japan the rates of CCA are 9.2 and 3.3 per 40,000 pregnancies, respectively.24 The gradual decline in the incidence of both CHM and CCA in developing countries over the past 40 years presumably is due in part to improved socioeconomic conditions, earlier completion of childbearing, and improved nutrition. Risk factors of CCA include prior CHM, ethnicity, and advanced maternal age. CCA is 1000 times more likely to occur after CHM than after another type of pregnancy. The risk is also increased in women of Asian, American Indian, and African descent.24 PHM are characterized by a triploid karyotype (69 chromosomes) derived from two paternal and one maternal haploid sets of chromosomes.27–27 Most have a 69,XXX or 69,XXY genotype derived from a haploid ovum with dispermic fertilization. The fetus present in a PHM generally exhibits the stigmata of triploidy, including growth retardation and multiple congenital anomalies such as syndactyly, hydrocephaly, omphalocele, and hare lip. CHM, in contrast, usually have a 46,XX genotype totally derived from duplication of the haploid genome of one sperm. A small percentage of CHM have 46,XY karyotype, consistent with dispermic fertilization. It appears that molar disease, both partial and complete, is associated with excess male genetic composition due to an abnormality of the egg, which is either devoid of maternal chromosomal material or allows for dispermy.28 Several growth factors and oncogenes have been studied in molar tissues and CCA. Increased expression of p53 and c-fms has been observed in CHM, and increased ras and c-myc RNAs have been measured in CCA.31–31 Fulop and associates32,33 have investigated the expression of various growth factors and oncogenes in normal placenta, complete and partial mole, and CCA. CHM and CCA were characterized by overexpression of c-myc, c-erbB-2, and bcl-2, and these oncoproteins could be important in the pathogenesis of GTN. Expression of c-fms protein did not differ between normal placenta and GTN. CHM and CCA were also characterized by increased expression of p53, p21, Rb, and MdM2. The p53 gene was studied to detect any mutation in 22 complete moles and 11 CCAs that had increased expression of p53. Because only one nonsense mutation in p53 was detected by polymerase chain reaction analysis, it is likely that the overexpressed p53 protein was the wild type. Although studies have identified increased expression of several growth factors in GTN, the precise molecular pathogenesis has not been determined. It was observed that the level of expression of epidermal growth factor receptor (EGFR) in CCA and the syncytiotrophoblast and cytotrophoblast of complete mole was significantly greater than the expression of EGFR in syncytiotrophoblast and cytotrophoblast of placenta and partial mole.29 This observation was consistent in both immunohistochemical and in situ hybridization studies. In complete mole, strong expression of EGFR and c-erbB-3 in the extravillous trophoblasts was significantly associated with the development of postmolar tumor. The EGFR-related family of oncogenes might be important in the pathogenesis of GTN. Extracellular proteinases such as matrix metalloproteinases (MMPs) are thought to be important in modulating both cell-matrix interactions and the degradation of the basement membrane necessary for invasion and metastases. CCA exhibits significantly stronger expression of MMP-1 and MMP-2 and decreased expression of tissue inhibitor of MMP-1 (TIMP-1) than are seen in the syncytiotrophoblast of complete and partial mole and normal placenta.34 The increased expression of MMP-1 and MMP-2 and decreased expression of TIMP-1 in CCA could contribute to the invasiveness of CCA cells. Certain genes are expressed normally on either the maternal or paternal allele, and this occurrence is described as parental imprinting. Modification of parental imprinting has been associated with tumor formation; both complete moles and CCA have relaxation of parental imprinting.35 Relaxation of parental imprinting could be important in the pathogenesis of GTN. Hydatidiform moles can be categorized as either complete or partial on the basis of gross morphology, histopathology, and karyotype (Table 90-1). Table 90-1 Features of Complete and Partial Hydatidiform Moles CHM is characterized by the following pathological features: • Vesicular swelling of placental villi. • Proliferation of trophoblastic cells (both cytotrophoblasts and syncytiotrophoblasts) with varying degrees of hyperplasia and dysplasia (Figure 90-1). • Fluid-filled and distended chorionic villi with scant or absent blood vessels. However, the pathological features of CHM have changed significantly over the past two decades owing to earlier diagnosis.36 Whereas cavitation and circumferential trophoblastic proliferation were present in three quarters of complete moles in the past, these findings are now present in fewer than half the cases. Mosher and coworkers37 compared pathological findings of 23 current complete moles (1994 to 1997; mean gestational age: 8.5 weeks) with 20 past complete moles (1969 to 1975; mean gestational age: 17 weeks). Histologically, complete moles that are now encountered have smaller mean maximal villous diameter (5.7 vs. 8.2 mm), less circumferential trophoblastic hyperplasia (39% vs. 75%), more primitive villous stroma (70% vs. 10%), and less global necrosis (22% vs. 54%). Keep and coworkers38 observed that early complete moles were characterized by focal trophoblastic hyperplasia, minimal villous cavitation, and hypercellular primitive stroma. Complete moles are now often characterized by subtle morphologic alterations that could result in their misclassification as partial moles or nonmolar hydropic abortions. DNA ploidy studies or karyotyping are useful adjuncts in these circumstances.26,27 Immunohistochemical tests for maternally expressed genes can also differentiate complete mole from partial mole and hydropic abortion.39,40 PHM is characterized by the following pathological features: IM is a tumor arising from a molar pregnancy that invades the myometrium by direct extension or by venous channels. Metastases to distant sites occur in about 15% of cases, most commonly to the lungs and vagina.28 The tumor is characterized by swollen placental villi and accompanying hyperplastic trophoblastic tissue, which is usually dysplastic when located in sites outside the uterine cavity (Figure 90-3). CCA is a highly malignant tumor characterized by abnormal trophoblastic cell hyperplasia and anaplasia, absence of chorionic villi, hemorrhage, and necrosis that invades the uterine wall directly or metastasizes hematogenously to distant sites, most commonly the lungs, vagina, brain, liver, spleen, kidneys, and intestines (Figure 90-4). PSTT and ETT are extremely rare, monocellular tumors that arise from the intermediate trophoblast of the implantation site. In the case of PSTT, tumor cells infiltrate the myometrium and grow between smooth muscle cells with vascular invasion (Figure 90-5). ETT characteristically tends to form nodular masses that invade the myometrium. Hemorrhage and necrosis are less evident. Placental villi are absent in both of these tumors. With the use of immunoperoxidase stains, human placental lactogen can be identified prominently in PSTT, whereas hCG is present only sparsely. In both these tumors, serum hCG levels are low, but relatively high levels of free beta subunit of hCG are detectable in patients with PSTT compared with other forms of GTN.41 There appears to be a direct correlation between the mitotic activity of PSTT and outcome.42 The remarkable curability of GTN might be attributable partly to a host immunologic response to paternal antigens expressed on trophoblastic cells.43 The prognosis of patients with gestational CCA has been related to the intensity of lymphocytic and monocytic infiltration at the tumor-host interface.44 Because the lymphocytes and macrophages that infiltrate gestational CCA are probably exposed to paternal antigens and oncoproteins, the immune cells could become activated. Immunologically active cells might promote the regression of GTN through their release of cytokines. Cytokines have been reported to inhibit the proliferation of CCA cells in vitro and to increase the human leukocyte antigen (HLA) expression of CCA cells in vitro, thereby increasing immunogenicity.45 It has been theorized that the development and progression of GTN could be favored by histocompatibility between the patient and her partner. If the patient and her partner are histocompatible, the trophoblastic tumor that bears paternal antigens might not be immunogenic in the maternal host. The intensity of the host’s immunologic response might depend on the immunogenicity of the trophoblastic tumor. On the other hand, histocompatibility between the patient and her partner does not appear to be a prerequisite for the development of persistent GTN.46 HLA systems could, however, influence the clinical course of rapidly progressive and fatal GTN. Tomoda and colleagues47 reported that drug-resistant CCA was associated with increased histocompatibility between the patient and her partner. Similarly, Morgenson and coworkers observed that histocompatibility between patients and partners was associated with a greater risk of metastatic disease.48 Because all chromosomes in a CHM are paternal in origin, a CHM is a complete allograft and could stimulate a vigorous immune response by the maternal host. There is evidence for both a cellular and a humoral response to CHM. When compared with normal placentas, molar implantation sites have fivefold increased infiltration by helper T cells.49 Circulating immune complexes have also been measured in patients with CHM and have been noted to increase as the patient entered remission.50 Circulating immune complexes in patients with CHM have been demonstrated to contain paternal HLA antigens.51 The maternal host with a CHM is therefore sensitized to paternal HLA antigens. The distribution of HLA antigens in molar chorionic villi has been determined by immunofluorescent assays.52 HLA A, B, and C antigens were detected on the stromal cells of molar chorionic villi but not on the villous trophoblast; however, the molar villous fluid that bathes the stromal cells does not contain soluble HLA antigen.43 The maternal host could therefore be sensitized to paternal HLA antigen when the villous trophoblastic layer is disrupted and HLA-positive villous stromal cells are released into the circulation. The clinical presentation of CHM has changed dramatically over the past two decades in the wake of the widespread use of ultrasound and improved methods for hCG measurement. Prior to 1980 CHM was usually diagnosed in the second trimester, whereas the diagnosis is now usually made in the first trimester, before the classic clinical signs and symptoms appear. Table 90-2 summarizes the signs and symptoms of classic CHM and PHM. When patients with CHM present with these classic signs and symptoms, they are at higher risk of developing GTN. Soto-Wright and associates36 compared the clinical presentation and outcome of patients with CHM at the New England Trophoblastic Disease Center (NETDC) between 1988 and 1993 with those of patients between 1965 and 1975 and noted that despite the change in presentation, there was no change in the incidence of GTN. Table 90-2 Presenting Signs and Symptoms of Classic Complete and Partial Hydatidiform Moles Patients with PHM typically present with symptoms that are indistinguishable from those of a threatened or spontaneous miscarriage, rather than with the classic symptoms of CHM, unless diagnosis is delayed until the second trimester. The diagnosis of PHM is usually suggested by ultrasonography and confirmed by pathological review of curettage material. hCG levels in patients with PHM are usually not as elevated as in patients with CHM. When PHM progresses into the second trimester, the ultrasound diagnosis becomes more accurate because of obvious fetal malformations associated with triploidy and the extent of vesicular change of the placenta. Patients with PHM whose diagnosis is delayed until the second trimester will, in many instances, recapitulate the classical signs and symptoms associated with CHM with regard to the incidence of preeclampsia, hyperthyroidism, trophoblastic embolization, and other complications.55–55 Although patients with CHM are now diagnosed earlier, patients with PHM have not been diagnosed substantially earlier and their clinical symptoms have not changed.22 • A plateau in the level of hCG over more than 3 consecutive weeks • 10% or greater rise in hCG for 3 or more values over at least 2 weeks • Persistence of hCG 6 months after molar evacuation Nonmetastatic or locally invasive GTN (NMGTN) develops in about 15% of patients after evacuation of CHM, 1% to 6% after PHM, and infrequently following other pregnancies.22,28,56 Patients with NMGTN present with irregular vaginal bleeding, ovarian theca lutein cysts if hCG levels are markedly elevated, and uterine subinvolution or asymmetrical enlargement due to the presence of tumor. Invasive tumor can erode through the uterine vessels causing vaginal bleeding, or perforate through the myometrium causing intraperitoneal hemorrhage. The presence of bulky necrotic tumor, characteristic of CCA, can serve as a nidus for sepsis, particularly Clostridium welchii. The presence of deep myometrial invasion can be confirmed by ultrasound or imaging studies such as magnetic resonance imaging (MRI). Metastatic GTN (MGTN) occurs in approximately 5% of patients after molar evacuation and infrequently after other gestations. Although IM infrequently metastasizes to distant sites, most MGTN is due to CCA, which characteristically disseminates widely hematogenously. Because trophoblastic tumors are highly vascular, metastatic lesions often present with signs and symptoms of spontaneous bleeding. The most common metastatic sites are the lung (80%), vagina (30%), brain (10%), and liver (10%).9 As a general rule, cerebral and hepatic metastases are uncommon unless there is concurrent involvement of the lungs and/or vagina. 1. Solitary or multiple discrete rounded densities 2. “Snowstorm” or alveolar pattern 3. Embolic pattern resulting from pulmonary artery occlusion Patients can develop pulmonary hypertension in the absence of substantial parenchymal involvement because of vascular obstruction with tumor. Because the respiratory symptoms and radiographic findings can be striking, patients may be thought to have a primary pulmonary disease, thus delaying the diagnosis. Therefore, it is important to obtain an hCG level in any woman of reproductive age who presents with evidence of metastatic disease without a known primary. Gynecologic symptoms may be minimal or absent in patients with extensive pulmonary involvement. In fact, the reproductive organs are frequently free of disease in patients with widespread metastases. Early respiratory failure requiring mechanical ventilation can develop in patients with extensive pulmonary involvement and can cause death before effective chemotherapy can be started.59–59 Risk factors for early respiratory failure within 1 month of presentation include greater than 50% lung opacification, dyspnea, anemia, cyanosis, and pulmonary hypertension. With chemotherapy, patients could develop bleeding into metastatic sites and potentially worsen pulmonary symptoms and radiologic findings. Kelly and associates57 observed that reducing the initial dose of chemotherapy did not protect against early respiratory failure and recommended administering intensive chemotherapy at the outset. Thirty percent of patients with MGTN have vaginal involvement. Vaginal metastases are most commonly located in the suburethral area or fornices and are due to venous embolization of either IM or CCA. They usually present with either a purulent discharge or irregular bleeding (Figure 90-6). Surgical excision of a vaginal metastasis should be avoided (except in unusual circumstances) because the hemorrhage that results is frequently difficult to control. After chemotherapy is instituted, and tumor shrinkage has occurred, the vaginal lesion can be excised with less risk, if necessary. However, the optimal treatment for bleeding from a vaginal metastasis is arterial embolization.60 Cerebral lesions also occur in approximately 10% of patients with MGTN. Similar to hepatic metastases, cerebral involvement is usually seen in postterm patients with advanced disease due to delayed diagnosis. Involvement of the central nervous system (CNS) is usually associated with headache, vomiting, seizures, and focal neurologic signs such as slurred speech, hemiparesis, visual disturbances, or signs of a spinal cord lesion. Neurologic symptoms usually result from increased intracranial pressure or bleeding.64–64 Bagshawe and Harland65 reported that the plasma-to-CSF hCG ratio was <60 in patients with CNS disease. However, a single plasma-to-CSF hCG ratio can be misleading because rapid changes in serum hCG levels due to the effects of treatment on the tumor output of hCG might not be reflected promptly in the CSF.66 Occult asymptomatic CNS metastases are now being detected because of improved imaging techniques (particularly MRI), which allows for earlier therapeutic intervention before neurologic sequelae develop. Gastrointestinal, renal, and splenic metastases usually occur in patients with advanced disease in which the diagnosis has been delayed. Abdominal computed tomography (CT) scanning is the best imaging technique for detecting these metastatic sites, although the use of whole-body 18F FDG-PET scanning is being used more commonly.67 PSTT and ETT are rare tumors that are derived from intermediate implantation site cytotrophoblasts. They can develop from any antecedent pregnancy, but most commonly arise from a term pregnancy or miscarriage and generally present months to years after the antecedent pregnancy with irregular vaginal bleeding or amenorrhea, enlarged uterus, and, rarely, nephrotic syndrome. The serum hCG level is relatively low in relation to tumor volume in comparison to other types of GTN. More than 30% of patients already have metastases at diagnosis.68,69 A reliable assay for hCG is central to the management of patients with trophoblastic disease. Most kits now used in commercial and hospital-based laboratories accurately measure all portions of the hCG molecule.70,71 Physicians treating patients with GTN, however, must recognize the limitations of the assay they are using and base clinical decisions on the clinical, morphologic, and radiologic findings as well as on hormonal results. Patients with CHM commonly have markedly elevated preevacuation hCG levels. Genest and coworkers72 noted that 46% of 153 patients with CHM who were managed at the NETDC between 1980 and 1990 had preevacuation hCG levels above 100,000 mIU/mL, whereas the preevacuation hCG levels in patients with PHM tend to be lower. Review of the data from the NETDC noted that only 2 of 30 patients with PHM presented with levels greater than 100,000 mIU/mL.73 False-positive hCG test results can occur because of a substance in the blood that interferes with the hCG assay. Although this is a rare occurrence (estimated at 1 in 10,000 to 1 in 100,000 tests), false-positive tests can be confusing to clinicians when they are attempting to diagnose disorders of pregnancy, including GTN. The misinterpretation of a false-positive test has led to inappropriate surgery and chemotherapy based only on persistently elevated serum hCG levels. False-positive hCG tests should be suspected if the clinical picture and the laboratory results are discordant, if there is no identifiable antecedent pregnancy, or if patients under treatment with low levels of hCG do not respond to treatment appropriately. Heterophile antibodies are thought to be responsible for this problem by interfering in the immunoassay systems used. These patients are also at risk of other false-positive serum test results. To avoid the pitfalls of a false-positive hCG test, it is important for the clinician to remember that the patient’s clinical presentation should correlate with the laboratory results. If there is a discrepancy, then a repeat hCG assay using a different immunoassay and a sensitive urine hCG test should be performed.71 Most commercially available kits have now been corrected for this problem. Quiescent GTN is another rare entity that is associated with persistent low levels of hCG, which can lead to inappropriate treatment. This entity is thought to be due to the presence of highly differentiated, noninvasive syncytiotrophoblastic cells. Characteristically, foci of disease are not otherwise demonstrable clinically, nor do hCG levels fall with therapy, presumably because the growth cycle of these cells is long and comparable to that of normal cells. Close observation of these patients is indicated because 6% to 10% will eventually develop overt GTN, requiring therapy. The hCG of patients with quiescent GTN is not hyperglycosylated, which is useful in correctly identifying these patients.74,75 The ultrasound appearance of CHM does not vary considerably between the first and second trimesters. At either stage, complex, echogenic masses with multiple small cystic spaces are visible within the uterus, and no fetus is identifiable (Figure 90-7). Two sonographic features have been described that are characteristic of PHM: focal cystic changes in the placenta and a ratio of the transverse-to-anteroposterior dimension of the gestational sac greater than 1.5.76 Changes in the shape of the gestational sac could be part of the embryopathy of triploidy. On rare occasions, particularly when PHM has progressed into the late first or early second trimester, the sonogram will show the presence of a fetus with multiple congenital abnormalities, focal hydropic changes in the placenta, oligohydramnios, and abnormal placental Doppler flow pattern. These changes might not be visible in the first trimester.
Gestational Trophoblastic Disease
Introduction
Terminology
Relevant Historical Issues
Incidence and Epidemiology
Etiology and Pathogenesis
Pathology
Feature
Complete Mole
Partial Mole
Fetal or embryonic tissue
Absent
Present
Hydropic villi
Diffuse
Focal
Trophoblast hyperplasia
Diffuse
Focal
Scalloping of chorionic villi
Absent
Present
Trophoblastic stromal inclusions
Absent
Present
Karyotype
46,XX; 46,XY
69,XXY; 69,XXX
Complete Hydatidiform Mole
Partial Hydatidiform Mole
Invasive Mole
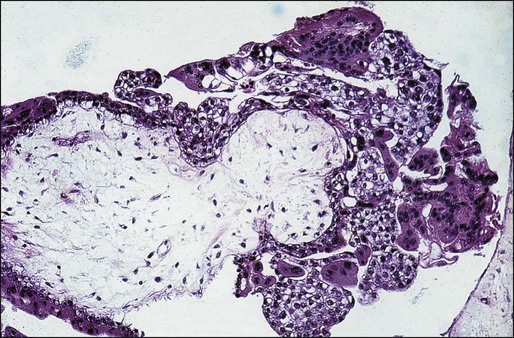
Choriocarcinoma
Placental Site and Epithelioid Trophoblastic Tumors
Immunobiology
Clinical Presentation
Complete Molar Pregnancy
Sign or Symptom
Complete Mole (%) (N = 306)
Partial Mole (%) (N = 81)
Vaginal bleeding
97
73
Excessive uterine size
51
4
Theca lutein cysts >6 cm
50
0
Preeclampsia
27
3
Hyperemesis
26
0
Hyperthyroidism
7
0
Trophoblastic emboli
2
0
Partial Molar Pregnancy
Gestational Trophoblastic Neoplasia
Nonmetastatic Gestational Trophoblastic Neoplasia
Metastatic Gestational Trophoblastic Neoplasia
Pulmonary Metastasis
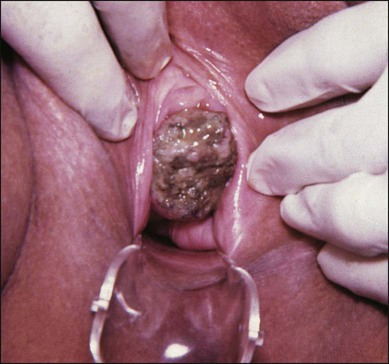
Vaginal Metastases
Brain Metastases
Other Metastatic Sites
Placental Site and Epithelioid Trophoblastic Tumors
Laboratory and Imaging Studies
hCG Measurement
False-Positive hCG Tests
Quiescent Gestational Trophoblastic Neoplasia
Ultrasound
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Gestational Trophoblastic Disease