Hereditary cancer syndromes are responsible for 5% of endometrial cancers and 10% of ovarian cancers. Hereditary breast and ovarian cancer syndrome and Lynch syndrome account for most of these inherited cases. Significant advances have been made in the identification and management of women with these syndromes. In addition, recent advances have highlighted the prognostic and therapeutic implications for women with gynecologic cancers and inherited cancer syndromes.
Approximately 5% of endometrial cancers and 10% of ovarian cancers can be attributed to an inherited predisposition. Given the current incidence of these diseases in the United States, hereditary cancer syndromes will lead to approximately 2200 new cases of ovarian cancer and 2300 new cases of endometrial cancer in 2011. Hereditary breast and ovarian cancer (HBOC) syndrome and Lynch syndrome account for most inherited gynecologic cancers. Other syndromes associated with gynecologic malignancies, such as Cowden syndrome, Li-Fraumeni syndrome, and Peutz-Jeghers syndrome, are rare.
Since the identification of the BRCA1 and BRCA2 genes and Lynch syndrome genes almost 20 years ago, significant advances have been made in the management of individuals who carry these gene mutations. In addition, important discoveries related to prognosis and treatment of the patient who has ovarian cancer with a BRCA1 or BRCA2 gene mutation have highlighted the role of genetic testing in the care of gynecologic oncology patients. This article reviews the 2 main inherited cancer syndromes relevant to gynecologic cancers, HBOC syndrome and Lynch syndrome.
HBOC syndrome
HBOC syndrome is caused by mutations in the BRCA1 or BRCA2 genes, which were first identified and cloned in the early 1990s. The prevalence of mutations in BRCA1 and BRCA2 among the general population has been estimated to be as high as 1 in 400. However, this varies among different populations. In certain populations that have undergone a period of relative isolation, founder mutations in BRCA1 and BRCA2 have been identified. For example, Ashkenazi Jews have a prevalence of approximately 1 in 40.
BRCA1 is localized to chromosome 17q, whereas BRCA2 is localized to chromosome 13q. As tumor suppressor genes, the proteins coded for by BRCA1 and BRCA2 are involved in recognition and repair of DNA damage, specifically double-stranded DNA breaks. They are large genes, with BRCA1 having 24 exons and BRCA2 having 27 exons. More than 1200 inherited mutations have been found to occur throughout each gene. Approximately 80% of these mutations are either nonsense or frameshift mutations resulting in truncated, nonfunctioning protein.
Women with a BRCA1 mutation have a risk of ovarian cancer by age 70 years of 39% to 46% and a lifetime risk of breast cancer by age 70 years of 65% to 85%. Reported risks of ovarian and breast cancers in women by age 70 years among BRCA2 carriers are 10% to 27% and 45% to 85%, respectively. Germline BRCA1 and BRCA2 mutations express incomplete penetrance. Furthermore, penetrance can be highly variable within families with the same BRCA mutation.
BRCA mutation carriers are also at risk for several other cancers. Those rarer cancers reported to be associated with BRCA mutations are male breast, pancreatic, and prostate cancers, although lifetime risk of these cancers is low compared with female breast and ovarian cancer. Other malignancies, such as melanoma and biliary cancers, have also been reported to occur in BRCA carriers. Aside from malignancies, there are no known physical abnormalities or other conditions associated with BRCA mutations.
Pathology of BRCA-associated Ovarian Cancers
Multiple studies have noted that BRCA-associated ovarian cancers are more likely to be high-grade serous adenocarcinoma than sporadic ovarian cancers. Although only 44% to 59% of sporadic ovarian cancers are serous, up to 86% of BRCA-associated ovarian cancers have serous histology. In addition, endometrioid, mucinous, and low malignant potential tumors are rarely diagnosed in BRCA-positive women. Low-grade serous cancers are also unlikely to be part of the BRCA cancer spectrum. When comparing the histology of BRCA1 and BRCA2 patients, no difference has been found.
Theory of the Fallopian Tube as a Potential Origin of BRCA-associated Serous Cancers
Most pelvic serous carcinomas are classified as ovarian. These cancers have been presumed to arise from the ovarian surface epithelium. However, there has recently been increasing interest in the fallopian tube as the potential site of origin of many BRCA-associated serous malignancies, including cancers that are typically diagnosed as ovarian.
This hypothesis developed as BRCA carriers and other high-risk women began to undergo risk-reducing salpingo-oophorectomy (RRSO) in the 1990s. The pathologic examination of these patients revealed early-stage, asymptomatic malignancies, with many located in the distal tube or fimbria. Most of these tumors were microscopic. However, not all of the tumors diagnosed in these studies were found in the tube. According to a recent summary of the published cases of malignancies found in RRSO specimens in BRCA carriers, approximately 21% of occult cancers involved the ovary alone, bringing into question whether the fallopian tube is the sole site of origin for serous carcinomas. Nevertheless, that most of the tumors found on RRSO are tubal is in contrast with the fact that fallopian tube cancer is rarely diagnosed in patients who present with late-stage serous carcinomas, with an incidence rate of only 0.41 per 100,000 women.
To explain why fallopian tube carcinomas are diagnosed more frequently in early occult malignancies than in patients with large tumors or metastatic disease, it has been proposed that many BRCA-associated pelvic serous carcinomas originate in the fallopian tube and subsequently spread to the ovary and other peritoneal surfaces. A lesion called serous tubal intraepithelial carcinoma (STIC) has been hypothesized to be the origin of most pelvic serous carcinomas. STICs are distinguishable from the normal fallopian tube and seem to have the ability to shed malignant cells without invading the tube. Several investigators have reported the presence of STICs in patients with positive peritoneal cytology. This finding explains how patients may have a large volume of tumor on the ovary and peritoneum (and therefore diagnosed as ovarian or primary peritoneal carcinoma) but little tubal disease, although their cancer originated in the tube.
Prognosis and Novel Therapies for BRCA-associated Ovarian Cancer
Multiple studies have found a significant progression-free and overall survival advantage for patients who have ovarian cancer with a BRCA mutation compared with women who are BRCA mutation-negative. Earlier studies evaluated only patients with Ashkenazi Jewish BRCA founder mutations. However, more recent studies comparing survival in non-Jewish BRCA-positive patients who have ovarian cancer with BRCA-negative patients have also identified a survival advantage in BRCA mutation carriers. In the largest evaluation of non-Ashkenazi Jewish BRCA carriers to date, Lacour and colleagues found significantly longer progression-free (27.9 vs 17.9 months) and overall (101.7 vs 54.3 months) survival when compared with patients with sporadic ovarian cancer. In addition, these investigators noted that BRCA status was an independent predictor of progression-free and overall survival.
The cause of the survival advantage for BRCA carriers with ovarian cancer is unknown. Although several hypotheses exist, the theory that BRCA mutations improve chemotherapy sensitivity has garnered the most evidence. BRCA1 plays an important role in the repair of double-stranded DNA breaks, a process called homologous recombination. Because mutated BRCA is unable to recognize and repair double-stranded DNA breaks, BRCA mutation carriers may be incapable of repairing chemotherapy-induced DNA damage, thus leading to improved treatment response. Ongoing research into the function of these 2 genes may help to elucidate the underlying improved prognosis seen in clinical studies.
A novel class of therapeutics, PARP (poly[ADP-ribose] polymerase pathway) inhibitors, exploit the inability of BRCA mutated cancers to adequately repair double-stranded DNA breaks. PARP is involved in the repair of single-stranded DNA breaks. Therefore, the combination of PARP inhibition with defective BRCA function in ovarian tumors leads to enhanced cell death, a concept termed synthetic lethality. Phase I and II studies of olaparib (an oral PARP inhibitor) have reported it to be efficacious with minimal side effects in BRCA-associated ovarian and breast cancers. In the phase II study, olaparib at a dose of 400 mg twice daily showed a 33% response rate. In addition, it seems to be most effective in platinum-sensitive patients.
Identifying Women at Risk for HBOC
Given their propensity for developing other malignancies, and the risk of having family members with the same mutation, it is important to identify patients with a BRCA mutation. The Society of Gynecologic Oncologists (SGO) has developed guidelines to aid in identifying patients at risk for HBOC. These same guidelines were also endorsed by the American College of Obstetricians and Gynecologists (ACOG). Table 1 details the SGO criteria.
| Risk Assessment Helpful | Risk Assessment Recommended |
|---|---|
| Women with breast cancer ≤40 years Women with bilateral breast cancer, especially if the first cancer was at ≤50 years Women with breast cancer at ≤50 years and a first-degree, second-degree, or third-degree relative with breast cancer at ≤50 years Ashkenazi Jewish women with breast cancer at ≤50 years Women with breast or ovarian cancer at any age and ≥2 first-degree, second-degree, or third-degree relatives with breast cancer at any age, especially if ≥1 breast cancer was at ≤50 years Unaffected women with a first-degree or second-degree relative meeting one of the above criteria | Women with a personal history of breast and ovarian cancer Women with ovarian cancer and a first-degree, second-degree, or third-degree relative with breast cancer at ≤50 years or ovarian cancer at any age Ashkenazi Jewish women with ovarian cancer Women with breast cancer at ≤50 years and a first-degree, second-degree, or third-degree relative with ovarian cancer or male breast cancer Ashkenazi Jewish women with breast cancer at ≤40 years Women with a first-degree or second-degree relative with a BRCA mutation |
| Patients with one of the above criteria have a 5%–10% chance of a BRCA mutation | Patients with one of the above criteria have a 20%–25% chance of a BRCA mutation |
There may be patients who do not meet these criteria but warrant genetic risk assessment. For example, families in which there are few female relatives or those in which multiple family members have undergone oophorectomy or hysterectomy at a young age may lead one to falsely assume a low risk of HBOC. In addition, women who are adopted may have little or no knowledge of their family history. Women with breast or ovarian cancer who present with one of these family histories should be considered for BRCA testing.
As expected, women diagnosed with a BRCA-associated cancer have a greater risk of having a BRCA1 or BRCA2 mutation than the general population. For example, women with high-grade ovarian cancer (excluding Ashkenazi Jewish women, who have a substantially increased risk) have an estimated 1 in 8 to 1 in 10 risk of one of these mutations. Based on this increased prevalence, it has been suggested that it is reasonable to offer BRCA testing to all women diagnosed with high-grade ovarian cancer. In general, women less than 21 years old should not be tested.
Kwon and colleagues recently performed an analysis highlighting the importance of genetic testing of patients with ovarian cancer. This study found that applying the SGO criteria to determine which patients with ovarian cancer to test for BRCA1 and BRCA2 mutations resulted in a cost-effective strategy for the prevention of future cancers in first-degree relatives of women who were tested. Many women who are high risk for HBOC are never referred for genetic assessment. In their retrospective study, Meyer and colleagues found that 48% of patients with ovarian cancer who in 2007 fulfilled the criteria outlined earlier were referred to genetic counseling. Although it seems that most providers are aware of referral criteria, a substantial portion are still not referring their high-risk patients for genetic testing. Reasons for this discrepancy are unclear, although a contributing factor may be that clinicians are not consistently able to identify patients at high risk for HBOC. A recent study noted that only 19% of primary care physicians were able to delineate low-risk from high-risk patients in a survey of clinical scenarios.
There is currently no consensus on the timing of referral for genetic testing for patients at high risk for HBOC. In the breast literature, many providers report a preference to refer their patients after they complete adjuvant treatment. However, most patients wish their physicians had broached the subject of genetic counseling earlier in their treatment course. In a study of patients with ovarian cancer who underwent BRCA testing, one-third had not been referred for genetic counseling until they had recurrent disease. Given the poor prognosis of recurrent ovarian cancer, the investigators argue for genetic counseling referral at initial diagnosis.
Surveillance
It is generally agreed that women diagnosed with a BRCA mutation should be routinely screened for cancers of which they are at risk. To date, there is limited evidence that ovarian cancer screening leads to improved survival. An evaluation of 13 ovarian cancer screening studies in high-risk women noted that of the 70 tumors discovered, only 24% were early stage. This finding is similar to the incidence of early-stage disease in the general population of unscreened patients, arguing that there may be no difference in mortality between screened and unscreened populations. However, survival outcome was unavailable for all but one of the studies included in the analysis. Large, prospective trials are under way in the United States and the United Kingdom to better determine the best way to screen women at high risk of ovarian cancer.
Expert consensus groups agree that BRCA-carriers with intact ovaries should be offered periodic screening given their high risk for developing ovarian cancer. Screening consisting of twice-yearly CA125 and transvaginal ultrasonography beginning at age 30 to 35 years, or 5 years earlier than the earliest age of ovarian cancer in the family, has been recommended by ACOG and the National Comprehensive Cancer Network (NCCN). Patients should be made aware that these recommendations are based on presumptive benefit only. The benefit of surveillance to women who have undergone salpingo-oophorectomy is unknown, and there are currently no recommendations for screening these patients for peritoneal cancer.
Chemoprevention
The protective effect of oral contraceptives against ovarian cancer in high-risk women has been shown in multiple studies. One of the largest studies to date, a case-control study of more than 3000 BRCA-positive women with and without ovarian cancer, noted an increasingly reduced risk of ovarian cancer with each year of use for up to 3 to 5 years. The decreased risk existed for both BRCA1 and BRCA2 carriers. Several other studies have also reported a protective effect of oral contraceptive use against ovarian cancer in BRCA-positive women, with longer use associated with decreased risk. Together, these studies suggest it may be reasonable for BRCA carriers with intact ovaries to use oral contraceptives to decrease their risk of ovarian cancer. However, there is conflicting evidence on the effect of oral contraceptive use on the risk of breast cancer in BRCA-positive women. Therefore, as with any intervention, women and physicians should have a balanced discussion of potential risks and benefits before initiating oral contraceptives.
RRSO
RRSO is the practice of removing the bilateral ovaries and fallopian tubes in BRCA carriers, and is the most efficacious method of ovarian cancer risk reduction. Oophorectomy has been recognized as a method of decreasing ovarian cancer risk since the 1950s. More recently, there have been multiple prospective and retrospective studies evaluating RRSO in BRCA-positive women. The most recent was a multicenter cohort study of almost 2500 BRCA-positive women who underwent either RRSO or surveillance. This study found an 86% decrease in ovarian cancer risk in patients who had a previous history of breast cancer and a 72% decrease in risk in women without breast cancer history. Other studies have reported a 75% to 96% decrease in ovarian cancer risk in BRCA carriers who underwent RRSO. A risk of 1% to 6% of primary peritoneal cancer remains after RRSO. Although small, this risk seems to persist for up to 20 years after oophorectomy. In addition, there is evidence that RRSO provides a survival advantage. Grann and colleagues reported that women who had undergone RRSO prolonged their survival by 2.6 years. Other studies have noted a 60% to 72% decrease in overall mortality in BRCA carriers who have undergone RRSO compared with those who have not.
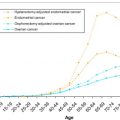
RRSO should be recommended to all BRCA carriers at the age of 40 years or after conclusion of childbearing. This guideline was developed because less than 2% to 3% of women with BRCA mutations develop ovarian cancer before the age of 40 years. In addition, BRCA1 mutation carriers’ chance of developing ovarian cancer increases exponentially during their 40s. Although BRCA2 mutation carriers’ risk of ovarian cancer does not increase until a later age, they have a greater decrease in their risk of breast cancer the earlier their ovaries are removed.
During RRSO, it is important to ensure that all ovarian and fallopian tube tissue is excised. In addition, pelvic washings should be performed at the beginning of the case because there are reports of positive cytology with no tumor found in the tissue specimen. There is currently insufficient evidence to recommend routine hysterectomy at the time of RRSO in the absence of other uterine or cervical pathologic results. Proponents of the procedure argue that it removes the intramural fallopian tube tissue and eliminates the possible increased risk of endometrial cancer in BRCA carriers. However, there have been no reports of patients developing cancer from the small amount of intramural fallopian tube tissue, and it remains unclear if BRCA-positive women truly have an increased risk of endometrial cancer.
Studies of pathologic specimens from RRSO have noted that up to 12% have an occult malignancy that is not grossly visible. Therefore, it is important that the entire pathologic specimen is carefully evaluated. It has been recommended that the entire tube and ovary be serially cut into 2-mm to 3-mm sections. In addition, clear communication with the pathologist is important to ensure that the specimen is assessed appropriately.
Although RRSO has definite benefits, concerns remain regarding the adverse effects for these young women undergoing surgical menopause, including osteoporosis and cardiovascular disease risks. Based on these concerns and emerging evidence of the fimbria as the site of origin for serous carcinomas, Leblanc and colleagues recently reported their experience on radical fimbriectomy in a cohort of BRCA mutation carriers undergoing risk-reducing surgery. With this procedure, the patients had most of their ovarian tissue left in situ, with plans to undergo a bilateral oophorectomy at a later date. Although the investigators found the procedure to be safe, they caution that the risks of an incomplete risk-reducing surgery are unknown and further studies are warranted.
Lynch syndrome
Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC) syndrome, accounts for most inherited endometrial cancer cases. The original family was described in 1913 by Aldred Warthin, although the syndrome was not characterized until the 1960s and 1970s. Since that time, Lynch syndrome has been recognized as an inherited mutation in one of the DNA mismatch repair genes ( MLH1 , MSH2 , MSH6 , or PMS2 ). The prevalence of these mutations in the general population is approximately 1 in 500 to 1 in 1000.
Inheritance and Penetrance
MLH1 , MSH2 , MSH6 , and PMS2 are all inherited in an autosomal-dominant pattern. These genes function to repair base-base mismatches and eliminate insertion or deletion loops of repetitive sequences that occur during DNA replication. Mutations in the mismatch repair genes are typically point mutations that lead to nonsense or missense mutations. Genomic deletions have also been observed. More than 1200 mutations have been described in these genes.
Most patients with Lynch syndrome are found to have a mutation in either MLH1 (50%) or MSH2 (40%). Approximately 10% of cases are attributable to an MSH6 mutation. Only a few patients have a mutation in PMS2 . Mutations in other mismatch repair genes have been described as associated with Lynch syndrome, including MLH3 and MSH3 . However, they have been only in isolated families.
Mutations in the mismatch repair genes associated with Lynch syndrome all express incomplete penetrance. In addition, the amount of penetrance seems to vary based on factors such as gene mutation. For example, MSH2 mutation carriers have been noted to have a significantly more increased risk of developing cancers than MSH1 mutation carriers. In addition, MSH6 mutations have been found to be responsible for a lower incidence of colorectal cancer, but a higher incidence of endometrial cancer. The reasons for these differences in penetrance are unknown.
Lynch-associated Malignancies
In women, Lynch syndrome is most commonly associated with colorectal and endometrial cancers, with a 40% to 60% lifetime risk of each. These patients typically develop endometrial cancer at an earlier age than the general population, with the mean age at diagnosis being 50 years. Approximately 10% of women diagnosed with endometrial cancer less than the age of 50 years have Lynch syndrome. Multiple other malignancies are associated with Lynch syndrome, which are listed in Table 2 .
| Malignancy | Lifetime Risk (%) |
|---|---|
| Endometrial | 40–60 |
| Colorectal (women) | 40–60 |
| Gastric | 13 |
| Ovary | 6–12 |
| Renal pelvis/ureter | 4–8 |
| Small bowel | <5 |
| Brain | 4 |
| Biliary tract | 2 |
Pathology of Lynch-associated Endometrial and Ovarian Cancers
Compared with sporadic endometrial cancers, the histology of Lynch syndrome-associated tumors is heterogeneous. A study comparing Lynch-associated endometrial cancers with sporadic cancers in women less than the age of 50 years and sporadic microsatellite instability-high cancers noted that although most of the tumors were of endometrioid histology, women with Lynch syndrome frequently had nonendometrioid histology and more stage II, III, and IV disease. The nonendometrioid tumors included clear cell carcinomas, carcinosarcomas, and mixed papillary serous and clear cell carcinomas, with most of these malignancies arising in MSH2 mutation carriers. In addition, studies have noted an important association between lower uterine segment tumors and Lynch syndrome. Westin and colleagues found that 29% of these uncommon tumors were in patients with Lynch syndrome.
Although limited data exist regarding Lynch-associated ovarian cancers, it seems that they are also heterogeneous. In the largest study of these malignancies to date, Watson and colleagues found that most were epithelial cancers with a wide variety of histologies. However, 85% were well or moderately differentiated. Ten percent to 22% of Lynch-associated ovarian cancers arise in the setting of a synchronous endometrial cancer, whereas approximately 5% of endometrial cancers are associated with a synchronous ovarian cancer.
Prognosis of Lynch Syndrome-associated Endometrial Cancer
In general, patients with Lynch syndrome-associated colorectal cancer have a better prognosis than those with sporadic tumors. However, there are limited data regarding endometrial and ovarian cancer prognosis for these women. Boks and colleagues found no statistical difference in survival rates between women with sporadic endometrial cancers and those with Lynch syndrome-associated tumors. An additional study of patients with ovarian cancer found a significant survival advantage for women with Lynch syndrome. However, both of these studies were small and have not been validated.
Identifying Women at Risk for Lynch Syndrome
Given their propensity for developing more than 1 primary malignancy, and the risk of having family members with the same mutation, it is important to identify patients with Lynch syndrome. Initial guidelines to assist physicians in identifying patients with Lynch syndrome were focused on colorectal cancer. However, women with HNPCC have an equal risk of colorectal and endometrial cancers. In addition, there is evidence that approximately 50% of patients with Lynch syndrome diagnosed with both endometrial and colon cancer were diagnosed with endometrial cancer first. For these reasons, screening guidelines that incorporate the risk of endometrial cancer are necessary. The SGO has published guidelines to aid with determining which patients should be screened for Lynch syndrome ( Table 3 ).
| Risk Assessment Helpful | Risk Assessment Recommended |
|---|---|
| Patients with endometrial or colorectal cancer diagnosed before 50 years Patients with endometrial or ovarian cancer with synchronous or metachronous Lynch-associated malignancies Patients with colorectal or endometrial cancer and more than 2 first-degree relatives with a Lynch-associated malignancy Patient with a first-degree or second-degree relative meeting the above criteria | Patients meeting revised Amsterdam criteria a Patients with synchronous or metachronous colorectal and ovarian or endometrial cancers Patients with a first-degree or second-degree relative with a known MMR mutation |
| Patients with one of the above criteria have a 5%–10% chance of Lynch syndrome | Patients with one of the above criteria have a 20%–25% chance of Lynch syndrome |
a Revised Amsterdam criteria are as follows: (1) at least 3 relatives with a Lynch-associated cancer in 1 lineage; (2) one affected individual is a first-degree relative of the other two; (3) at least 2 successive affected generations; (4) at least 1 Lynch-associated cancer is diagnosed before age 50 years.
Surveillance
Although there are compelling data to recommend colonoscopy every 1 to 2 years for individuals with Lynch syndrome, there is currently no strong evidence on how to screen these women for gynecologic malignancies. A study based on families diagnosed with Amsterdam II criteria found that only approximately 3% to 7% of gynecologic malignancies would develop before 30 to 35 years if screening were begun at this age. Studies have attempted to evaluate transvaginal ultrasonography alone, transvaginal ultrasonography with CA125, and endometrial biopsy with hysteroscopy as screening methods for endometrial cancer in patients with Lynch syndrome. Other studies have examined the use of transvaginal ultrasonography with endometrial biopsy and the combination of transvaginal ultrasonography, endometrial biopsy, and CA125. In general, it has been noted that these tests have low sensitivity for detecting disease, although studies that include endometrial biopsy seem to be the most effective. Although endometrial cancer is typically characterized by abnormal vaginal bleeding, women with Lynch syndrome are often premenopausal, and abnormal bleeding may not be recognized promptly. Based on these limited data, expert opinion has generally recommended that women with Lynch syndrome should receive annual endometrial biopsies and transvaginal ultrasonography once they reach the age of 30 to 35 years.
Risk-reducing Surgery
In 1997, the Cancer Genetics Studies Consortium stated “evidence of benefit is lacking” in regards to the risk-reducing surgery for women with Lynch syndrome. However, since that time there have been additional studies addressing the ability of prophylactic hysterectomy and bilateral salpingo-oophorectomy to decrease the risk of gynecologic malignancies for these women. Schmeler and colleagues reported their experience with 315 women with Lynch syndrome who underwent surveillance or prophylactic hysterectomy with or without salpingo-oophorectomy. These investigators found that they prevented 100% of endometrial and ovarian cancers by performing surgery, although the difference in ovarian cancer between the surgery and surveillance group was not statistically significant. A recent analytical model of 10,000 theoretic women with Lynch syndrome found it would take 28 surgeries to prevent 1 case of ovarian cancer, but only 6 surgeries to prevent 1 case of endometrial cancer. These and other studies have led experts to recommend that prophylactic hysterectomy and bilateral salpingo-oophorectomy be offered to all women with Lynch syndrome at the age of 35 years or once childbearing is complete. Women undergoing risk-reducing surgery may still be at risk for primary peritoneal cancer, and should be counseled accordingly. However, the amount of risk is unknown because only case reports are available.
As with BRCA mutation carriers, it is important that patients with Lynch syndrome undergoing prophylactic surgery have all pathologic specimens carefully examined. Schmeler and colleagues noted that 5% of women undergoing prophylactic surgery had an occult endometrial cancer. In addition, it has been suggested that patients undergo preoperative endometrial biopsy, transvaginal ultrasonography, and CA125 to aid with diagnosis of these occult malignancies before surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree