Question 7.1 The family depicted has Lynch syndrome (previously referred to as the hereditary nonpolyposis colon cancer [HNPCC]) syndrome. This syndrome is characterized by a high risk to develop colon and endometrial cancer and an increased risk to develop various other tumor types. Before her death, individual III-2 had genetic testing of the MLH1 and MSH2 genes, and an MSH2 gene mutation was identified. Specifically, the mutation is c.942 + 3A > T. MLH1 and MSH2 gene mutations account for 80% to 90% of families with HNPCC. Individual II-1, depicted with the arrow, has not been diagnosed with cancer. He has undergone frequent colonoscopy screening. He has also had genetic testing and was found to carry the family MSH2 gene mutation. The finding that individual II-1 has not been diagnosed with cancer can be explained by which of the following concepts?
A. Genetic testing laboratory error
B. Clinical variability
C. Genetic heterogeneity
D. Reduced penetrance
Question 7.2 Assuming individual II-3 has the family MSH2 gene mutation, what is the calculated probability Diane (individual IV-1) has inherited the MSH2 gene mutation?
A. 0%
B. 12.5%
C. 25%
D. 50%
Question 7.3 Diane (individual IV-1) is 24 years of age. She approaches her primary care physician about her medical management, given her family history of the Lynch syndrome. She has a healthy body weight and does not smoke. Both her paternal grandmother (II-3) and her father (III-6) refuse to have genetic testing. In addition to her annual Pap smear, which of the following cancer screening is most appropriate for Diane?
A. Colonoscopy screening to begin at 50 years of age
B. Sigmoidoscopy screening to begin by 25 years of age
C. Colonoscopy screening to begin by 25 years of age
D. Colonoscopy and mammography screening to begin by 25 years of age
Question 7.4 Diane (individual IV-1) decides to pursue genetic testing to aid in her medical management. She states that her father will not undergo genetic testing. What specific genetic test should be ordered?
A. Full sequencing of the MSH2 gene
B. Full sequencing of the MSH2 and MLH1 genes
C. Mutation specific analysis of the MSH2 gene
D. Deletion analysis using multiplex ligation-dependent probe amplification
Question 7.5 Which of the following factors suggest that a family may have hereditary cancer?
A. Young age at diagnosis
B. Bilateral cancer in an affected family member
C. Multiple affected generations
D. All of the above
Refer to the following pedigree for Questions 7.6 to 7.8.
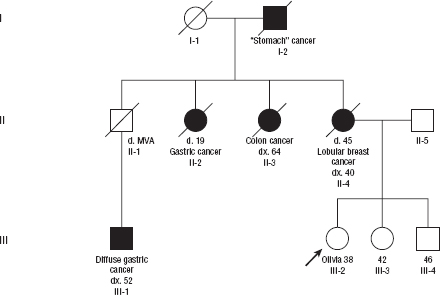
Olivia is a 38-year-old healthy woman who presents to her primary care physician concerned about her family history of cancer. She has no chronic health concerns. Both her mother’s and father’s family are of Ashkenazi Jewish ancestry. Olivia pursues an evaluation with a clinical geneticist for assessment and genetic testing.
Question 7.6 The clinical geneticist diagnoses the family with which cancer predisposition syndrome?
A. HNPCC syndrome
B. Hereditary breast cancer 1 (BRCA1) syndrome
C. Li–Fraumeni syndrome
D. Hereditary BRCA2 syndrome
E. None of the above
Question 7.7 Genetic testing is recommended to begin with which family member(s)?
A. Olivia, III-2
B. Olivia’s oldest sibling, individual III-4
C. Olivia and her two siblings should be tested at the same time
D. Olivia’s maternal first cousin, individual III-1
Question 7.8 Which of the following statements regarding prophylactic oophorectomy is TRUE?
A. Prophylactic bilateral salpingo-oophorectomy (BSO) is the most effective therapy to reduce the risk of ovarian cancer in women with BRCA1 or BRCA2 gene mutation.
B. BSO in BRCA1 or BRCA2 gene mutation carriers is indicated at age 30.
C. BSO in BRCA1 or BRCA2 gene mutation carriers has no effect on the risk of developing breast cancer.
D. All the above.
Question 7.9 Jennifer is a 38-year-old woman who was diagnosed with stage IIA ductal carcinoma at 30 years of age. She undergoes direct genetic testing of the BRCA1 and BRCA2 genes and is found to have a BRCA2 gene variant. Specifically the variant is Q713L (2366A > T), which results in the substitution of leucine for glutamine at amino acid 713 of the BRCA2 protein. The functional significance is unknown. Jennifer’s sister, Angela, is 40 years of age and has no personal history of cancer. Which is the most appropriate genetic testing approach for Angela?
A. Genetic testing is recommended for Angela because it will clarify her breast cancer risk.
B. Genetic testing is not recommended for Angela because it will not clarify her breast cancer risk.
C. Genetic testing is recommended for Angela because it will help clarify Jennifer’s genetic test results.
D. A and C.
Question 7.10 Which of the following statements regarding people with a BRCA1 or BRCA2 gene mutation are TRUE?
A. The majority of BRCA1 gene mutation carriers who develop breast cancer develop estrogen receptor–positive breast tumors, and BRCA2 gene mutation carriers most often develop estrogen receptor–negative breast tumors.
B. BRCA1 and BRCA2 gene mutation carriers have an increased risk to develop pancreatic cancer.
C. BRCA2 gene mutations are associated with an increased risk for follicular thyroid cancer
D. Prophylactic bilateral mastectomy decreases the risk of breast cancer by more than 90% among women with a BRCA1 or BRCA2 gene mutation.
Refer to the following pedigree for Questions 7.11 and 7.12.
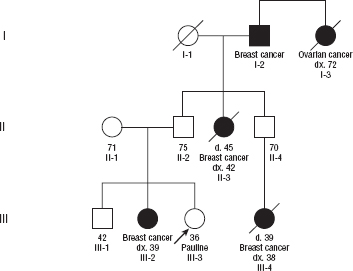
Question 7.11 Pauline, the family proband as designated by the arrow, is a healthy 36-year-old woman who presents to her gynecologist concerned about her breast cancer risk. She requests genetic testing. No other family member has undergone genetic testing. The gynecologist orders BRCA1 and BRCA2 gene testing. No mutation is identified. Which of the following statements is the CORRECT interpretation of Pauline’s testing?
A. Pauline’s test result is a true negative.
B. Pauline’s test result is a variant of uncertain significance.
C. Pauline’s test result is uninformative.
D. Pauline’s test result is positive.
Question 7.12 Pauline’s sister, individual III-2, is currently undergoing neoadjuvant chemotherapy for an aggressive ductal carcinoma of the breast. She is not interested in pursuing genetic testing at this time given the demands of her treatment. What breast health screening recommendations do you make for Pauline given her negative genetic testing?
A. Mammography beginning at age 40 years
B. Mammography and breast ultrasound beginning at age 40 years
C. Mammography and breast ultrasound beginning now
D. Mammography and breast MRI beginning now
Question 7.13 Which of the following malignancies does NOT have a significant increase in incidence among people with Lynch syndrome?
A. Colon cancer
B. Cervical cancer
C. Ovarian cancer
D. Endometrial cancer
Question 7.14 A 28-year-old woman with bilateral ductal cancer presents to the medical oncologist for assessment and treatment. Her medical history is notable for intussusception at 6 years of age. On her physical examination, the medicine resident notices small blue/black hyperpigmented macules on her lips, buccal mucosa, and fingertips. What is her diagnosis?
A. Hereditary BRCA1 syndrome
B. Hereditary BRCA2 syndrome
C. Li–Fraumeni syndrome
D. Peutz–Jeghers syndrome
E. Cowden syndrome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



