Gastrointestinal Disease
1 Nashville Gastroenterology Specialists, Nashville, TN
2 Riley Hospital for Children at Indiana University Health, Indianapolis, IN
Introduction
Digestive disorders are often complex illnesses requiring a multi-faceted approach. Rarely is there one solution that will work for all patients. In addition to medical treatment of the underlying disease, nutrition therapy can improve gastrointestinal (GI) symptoms. The impact of dietary manipulations, such as dietary fiber in irritable bowel syndrome or a gluten-free diet in celiac disease, demonstrates the intricate role that nutrition therapy plays in the management of chronic digestive disorders. GI complaints, even seemingly mild, can negatively impact patients’ quality of life. Healthcare providers often evaluate and treat digestive disorders, and patients seek care for various symptoms from food intolerances to chronic digestive diseases. Clinicians must determine whether symptoms such as abdominal pain, nausea, and altered bowel habits are caused by dietary intolerance, underlying GI pathology, or anxiety. The role of the health professional is to differentiate between more benign versus potentially life-threatening GI symptoms. Once a diagnosis is found, the patient becomes a partner in the management of his/her GI problem. Depending on the diagnosis and the severity of disease, the patient may need a referral to a specialist such as a gastroenterologist or hepatologist. Management of these disorders frequently includes some degree of dietary manipulation. Some dietary guidelines, such as a diet rich in whole grain foods, can be useful across the spectrum of most GI symptoms, whereas certain disorders require specific nutritional modifications. Clinicians with a strong understanding of the role of nutrition in GI illnesses will be well suited to optimize disease management and improve patients’ quality of life.
Digestion and Absorption
Nutrient digestion requires a controlled process of mechanical and chemical breakdown, with subsequent enzymatic and secretory responses that facilitate nutrient absorption. Carbohydrate digestion requires adequate amylase to convert starches into disaccharides, which then undergo further hydrolysis into monosaccharides. Monosaccharides are absorbed through a process of either diffusion or active transport. Dietary fats require the action of lipase, which results in the hydrolysis of free fatty acids from triglycerides. Once hydrolyzed, monoglycerides, glycerol, and fatty acids, as well as fat-soluble vitamins, undergo emulsification by bile acids in order to promote diffusion across the cell membrane of the enterocyte. Protein digestion requires adequate gastric acidity, which activates pepsin and other proteases, allowing breakdown of proteins into peptides and amino acids. Defects in any of the mechanical, chemical, or secretory processes involved in digestion can result in nutrient maldigestion and malabsorption.
Malabsorption
Inadequate nutrient absorption can occur as a result of many diseases of the digestive system. In order to effectively treat the symptoms of malabsorption, one must first identify the cause, after which appropriate treatment can be implemented. The management of disorders of carbohydrate, protein, and fat malabsorption can often be improved with appropriate nutrition therapy.
Carbohydrate Malabsorption
Lactose intolerance is the most common form of carbohydrate malabsorption and has been estimated to affect approximately 70 to 75 percent of the world’s population. Lactose is a disaccharide sugar that requires hydrolysis by the enzyme lactase into glucose and galactose for absorption. Lactose malabsorption or intolerance is usually caused by suboptimal activity or deficiency of lactase. Characteristic symptoms of lactose intolerance include bloating, abdominal pain, flatulence, borborygmi, nausea, or diarrhea after consumption of dairy foods. These symptoms are caused by the passage of undigested lactose into the colon where it is metabolized by colonic bacteria, producing excess fluid and gas in the bowel. In some cases, individuals will have delayed GI motility possibly due to the result of methane production. These patients will often present with constipation. The diagnosis of lactose intolerance can frequently be made by improvement or resolution of symptoms after temporary avoidance of dairy foods. It is sometimes necessary to confirm the diagnosis with a lactose tolerance test or lactose hydrogen breath test if symptom etiology is present, as other GI disorders, such as irritable bowel syndrome, inflammatory bowel disease, or celiac disease may be suspected.
Lactase production naturally declines as one ages. Lactose expression on the mucosal surface of the human enterocyte is at its peak at 34 weeks gestation, and begins to decline within the first few months of life. Thus, while lactase deficiency may be pathological in infants, it is normal in most teens and adults. Secondary lactase deficiency can occur as a result of certain GI disorders including bacterial overgrowth, mucosal injury, or inflammatory bowel diseases. Effective treatment of these underlying disorders may improve lactose tolerance.
The prevalence of lactase deficiency among populations suggests a certain genetic predisposition. Lactose malabsorption occurs in approximately 5 to 20 percent of Caucasians, but may be as high as 50 to 80 percent in Latinos, 60 to 80 percent among African–Americans and Ashkenazi Jews, and nearly 100 percent among Asians and American Indians. The goal of treatment for lactose intolerant individuals is to improve symptoms while preventing secondary bone disease by supporting adequate calcium intake. Lactose-free dairy foods and lactase supplements make it possible for individuals with lactose intolerance to consume adequate dietary calcium from dairy foods. For patients with lactose intolerance, the severity of symptoms is often related to the quantity of lactose consumed. Given the high calcium and vitamin D content in dairy foods, all individuals, regardless of lactose malabsorption, should be encouraged to include three servings of low-fat dairy foods in their diet every day.
Lactose hydrolyzed products can be well tolerated in those patients who are lactose intolerant. In addition, fermented dairy foods such as yogurt, fermented cheese, and fermented milk contain lactic acid bacteria, which improve tolerance and result in decreased symptoms related to lactose malabsorption. There may be some benefit from probiotics in patients with lactose malabsorption, possibly because microbial lactase is present within lactic acid bacteria in the probiotics themselves; however, research is ongoing in this area. In addition, non-dairy foods and beverages enriched with calcium, such as soy, hemp, almond, coconut and rice milk, and yogurt are good options for patients who are lactose intolerant. Ingredients that may not be well tolerated by persons with lactose intolerance include:
- whey or lactose,
- non-fat milk solids, buttermilk, or malted milk,
- margarine or sweet or sour cream.
Lactose intolerant patients who are unable to tolerate adequate intake of dairy foods should be encouraged to consume calcium-fortified foods or take a 1000 mg calcium supplement once a day to ensure adequate recommended intake. The DRI for men and women age 19 to 50 is 800 mg/day and 1000 mg/day for those over 51 years of age. Table 2-2 identifies the recommended daily intake of calcium for all age groups. Food sources of calcium are shown in Appendices G and H.
Protein Malabsorption
Celiac disease, also termed gluten intolerance, is a small bowel absorption disorder characterized by chronic inflammation of small bowel mucosa, villous atrophy, and crypt hyperplasia. It is caused by intolerance to gliadin, the protein fraction of wheat, rye, and barley in genetically predisposed individuals. The prevalence of celiac disease is approximately 1 percent in the general United States population. However, the disorder remains largely under-diagnosed. Frequently there are delays in diagnosis even after a patient seeks medical care for symptoms. Currently the only treatment for celiac disease is a life-long adherence to a gluten-free diet. Disease presentation is variable and onset of celiac disease can occur at any age. Presenting symptoms of celiac disease can be GI in nature (diarrhea, weight loss, vomiting, abdominal pain, bloating, distension, anorexia, and constipation) or may be less specific and include iron deficiency anemia, folic acid or vitamin B12 deficiency, osteoporosis or osteomalacia, infertility, or elevated transaminases. Neurological symptoms, such as ataxia, have also been traced to gluten intolerance. In recent years “silent” celiac disease or “non-celiac” gluten sensitivity has been described. Patients may present with non-specific symptoms, such as those associated with irritable bowel syndrome, or extra-GI symptoms such as headaches (Chapter 7: Case 3).
Testing for celiac disease should be pursued in patients with persistent GI symptoms, such as chronic diarrhea, malabsorption, weight loss, or abdominal distension. Testing should also be considered in patients with unexplained iron deficiency anemia, vitamin deficiencies, infertility, or elevated transaminases. Recent research suggests a higher prevalence of celiac disease among patients with osteoporosis but conflicting data have been presented. High-risk populations for celiac disease include those with autoimmune endocrinopathies (especially type 1 diabetes mellitus), first and second-degree relatives of persons with celiac disease, and Turner syndrome. The diagnostic evaluation of celiac disease should occur while the patient is on a gluten-containing diet and should include serologic testing followed by a small bowel biopsy if serologic testing is positive. The National Institutes of Health (NIH) consensus statement on celiac disease recommends the IgA antihuman tissue transglutaminase (TTG) and IgA endomysial antibody immunofluorescence (EMA) tests to avoid false negative results in IgA deficient patients. Positive results warrant small bowel biopsies for histologic confirmation. Recommendations for people with celiac disease are shown in Table 7.1.
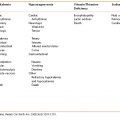
Table 7-1 Key Recommendations for Celiac Disease
|
Clinical evaluation should include an assessment for vitamin and mineral deficiencies. Initial blood work should include liver function tests, serum iron or ferritin, serum or red blood cell folate, vitamin B12, calcium, and vitamin D. A DEXA scan should also be considered in patients diagnosed with celiac disease to screen for osteoporosis. In addition, serum albumin levels should be tested, as low levels may reflect small bowel protein loss. Serum albumin can also serve as one component of the overall assessment of nutritional status and be used as a baseline to monitor improvement as treatment progresses. Identified deficiencies should be replenished, but long-term supplementation is likely not required once the disease is under control. Annual evaluation of vitamin status should be done as deficiencies of folate and vitamin B6 have been documented in patients on long-term, gluten-free diets.
The gluten-free diet excludes all foods containing wheat, rye, and barley. Recent evidence suggests that patients can safely consume small amounts of oat-containing foods and gluten-free labeled oatmeal; however, questions about safety remain with an oat-containing, gluten-free diet. Some patients report worsened GI symptoms when including oats in the diet, even if mucosal integrity is maintained. the principles of a gluten-free diet are described in Table 7-2. Patients should be advised to look for the many “gluten-free” products, which are increasingly available in supermarkets and natural foods stores.
Table 7-2 Gluten-Free Diet Guidelines
Source: The Celiac Disease Foundation and the Gluten Intolerance Group.
| Celiac disease, sometimes called gluten intolerance, is a disorder that prevents wheat products from being properly digested. Gluten is found in most grain products, including wheat, barley, and rye. The list below provides basic guidelines for a gluten-free diet. It is important to get additional education from a nutritional professional who specializes in celiac disease. Allowed Foods
|
After diagnosis, patients should always be referred to a registered dietitian for assessment of nutritional deficits, degree of malnutrition, and education on a gluten-free diet. In addition, information on patient resources and support groups should be provided. Some studies examining the nutritional quality of gluten-free diets demonstrated that despite adherence to dietary restrictions, overall diet quality tends to be poor. The majority of women consume sub-optimal intakes of whole grain foods, fiber, calcium, and iron. While men were more likely to consume adequate amounts of fiber and iron, diet choices remained low in calcium and whole grain foods. In addition, gluten-free diets tended to be higher in concentrated sweets and soft drinks. Some studies have even shown a trend towards increased BMI, rather than weight loss, after the gluten-free diet has been implemented, but this may be due to improved calorie and nutrition absorption. This data has lead some healthcare professionals to question the long-term adequacy of the gluten-free diet and the potential impact it may have on chronic medical conditions such as heart disease and diabetes mellitus. It should also be noted that while most wheat-based products in the United States are fortified with vitamins and minerals, gluten-free products are usually not. To improve diet quality, patients with celiac disease should be encouraged to consume 6 to 11 servings of whole grain or enriched gluten-free grains and three servings of gluten-free dairy foods per day. In addition, gluten-free vitamins are commercially available, and these may aid those with celiac disease in meeting daily vitamin and mineral requirements. All healthcare providers, in partnership with gastroenterologists and dietitians, should reinforce the need for life-long diet adherence to the gluten-free diet in patients with celiac disease, particularly after symptom resolution.
Fat Malabsorption
Fat malabsorption is associated with many GI disorders and frequently presents with symptoms of steatorrhea. Fat malabsorption may occur in cases of impaired luminal transport of products of digestion, and is often seen in disorders causing widespread mucosal injury, such as celiac disease, inflammatory bowel disease, and bacterial overgrowth. In such cases, management of the underlying mucosal disorder is the treatment of choice. Steatorrhea can also be caused by maldigestion of fats, due to lipase deficiency or a lack of emulsification, as seen in chronic pancreatitis, cystic fibrosis, and bile salt deficiencies. In addition, fat malabsorption can be seen in wasting syndromes, such as HIV wasting, or can be iatrogenic in nature, such as post-gastric bypass or extensive resection of the small bowel, particularly the terminal ileum. Untreated fat malabsorption may result in weight loss, failure to thrive, osteomalacia, bone pain, infertility, dysmenorrhea, and amenorrhea. In addition, fat-soluble vitamin deficiencies (A, D, E, and K) may occur.
Adoption of a low-fat diet may aid in symptom management. Patients following a low-fat diet may have difficulty consuming adequate calories to maintain weight. Additional calories can be added to the diet with the use of medium chain triglycerides (MCT). These provide 115 calories per tablespoon. MCT oil is rapidly hydrolyzed and absorbed directly into portal circulation and therefore does not require bile salts or micelle formation for digestion. Factors limiting the use of MCT oil include poor palatability and possible side effects such as nausea and vomiting; therefore, patients are typically unable to consume more than 3 to 4 tablespoons per day. Oral nutrition supplements with added MCT oil are commercially available and may provide some benefit. Unfortunately, these products tend to be very expensive and they are often not covered by medical insurance. For patients with pancreatic exocrine insufficiency, supplemental pancreatic enzymes may be necessary. Recent evidence suggests that patients with chronic pancreatitis may benefit from early screening for fat malabsorption. These patients may present with post-prandial abdominal pain resulting in reduced caloric intake even in the absence of clinically significant steatorrhea. Conjugated bile acids may improve digestion of fat in patients with a history of ileal resection.
Fat malabsorption places patients at risk for vitamin and mineral deficiencies, specifically fat-soluble vitamins (vitamins A, D, E, and K). Monitoring for fat-soluble vitamin deficiencies should occur on an annual basis, with aggressive repletion as needed. Provision of fat-soluble vitamins in a water-miscible form may allow patients to have better vitamin absorption. Deficiencies of calcium, magnesium, zinc, and iron may also be present due to impaired absorption and increased intestinal losses and should be aggressively repleted.
Gastric Disorders
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease (GERD) is characterized by a burning sensation in the substernal area caused by abnormal reflux of acidic gastric contents into the esophagus. This condition has been reported to affect up to 20 percent of the population. As many as one in seven persons may suffer from daily symptoms of “heartburn”, which can negatively affect patients’ quality of life. Although the underlying causes of GERD are not known, the pathogenesis has been related to altered and intermittent relaxation of the lower esophageal sphincter. Over the long term this can result in esophageal mucosal damage and erosion, and may increase risk of complications, such as peptic stricture, chronic esophagitis, Barrett’s esophagus, and development of esophageal adenocarcinoma.
Obesity is considered a significant risk factor for development of GERD. Increasing abdominal circumference is associated with increased intra-abdominal pressure and lower esophageal sphincter relaxation, which may contribute to the development of GERD. The risk of GERD increases with increasing BMI. Other lifestyle factors that have been positively associated with the incidence of GERD include poor quality of sleep, regular use of non-steroidal anti-inflammatory drugs (NSAIDs), heavy alcohol intake, and irregular dietary habits. Recent evidence has also suggested a possible association by Helicobactor pylori infection and gastroesophageal reflux symptoms.
Specific dietary factors have been evaluated as a cause of reflux disease. Although limited data are available, spicy foods, acidic foods, high-fat foods, chocolate, mint, and caffeine (coffee, tea, cola) have been associated with GERD symptoms. High-fat intake, particularly saturated fat, has also been found to increase the risk of GERD. High-fat foods or large meals delay gastric emptying time, which can lead to increased reflux of gastric contents. There is some evidence that increasing dietary fiber may have a protective effect against reflux. The mechanism is unclear, but may be related to fiber’s role as a nitrite scavenger in the gut as nitrites have been implicated in contributing to decreased lower esophageal sphincter tone.
Nutrition therapy for patients with GERD should be focused on minimizing reflux symptoms. Patients may have varying degrees of sensitivity to different high-risk foods. The goals of therapy should be to prevent relaxation of the lower esophageal sphincter, reduce volume of gastric acid, and prevent esophageal irritation. In addition, encouraging patients to gradually increase their intake of whole grain foods may reduce their reflux symptoms. Table 7-3 lists dietary recommendations for patients with GERD.
Table 7-3 Key Dietary Recommendations for Gastroesophageal Reflux Disease
Source: Lisa Hark, PhD, RD and Darwin Deen, MD, 2014. Used with permission.
|
Peptic Ulcer Disease
The management of peptic ulcer disease (PUD) has changed significantly in recent decades. Early treatment of PUD included a bland diet as a mainstay of treatment. It is now understood that most gastric and duodenal ulcers are caused by damage to the gastric mucosa, and the most common causative agents are the bacteria Helicobacter pylori, and the overuse of NSAIDS. Treatment of the underlying cause of PUD may result in resolution of symptoms of PUD.
Gastric acid secretion occurs as a result of vagal stimulation of the parietal cells by the sight or taste of food. Although gastric acid is no longer thought to be responsible for ulcer development, reduction in gastric acid may facilitate healing and decrease abdominal discomfort. Certain foods are known to increase gastric acid secretions including coffee, tea, colas, and alcohol. No differences have been found in randomized controlled trials that compared restricted diets with unrestricted diets in the resolution of ulcers. The focus of nutrition therapy should be based on individual tolerance and patients should be encouraged to avoid their individual triggers. Foods that are often poorly tolerated include coffee, orange juice, fried foods, spicy foods, and fruits. After treatment of a Helicobactor pylori infection, improved tolerance of these trigger foods has been demonstrated. There is some evidence that malabsorption of certain vitamins and minerals may occur in patients with peptic ulcer disease. Specifically, intestinal absorption of iron, vitamin B12, folic acid, and vitamins A, C, and E have been reported to be reduced. This may be due to modified intragastric pH seen in PUD. The clinical significance of this is uncertain. However, the clinician should consider possible testing for these deficiencies in patients with PUD who demonstrate clinical symptoms of vitamin and mineral deficiencies. Table 7-4 outlines key dietary recommendations for symptom management of PUD.
Table 7-4 Key Dietary Recommendations for Peptic Ulcer Disease
Source: Lisa Hark, PhD, RD and Darwin Deen, MD, 2014. Used with permission.
|
Small and Large Bowel Disorders
Diarrhea
Diarrhea is characterized by increased frequency of loose or watery stools, and may be acute or chronic in nature most often due to self-limited viral or bacterial infections. Acute diarrhea often resolves on its own, whereas chronic diarrhea lasts for more than 4 weeks. Up to 5 percent of the population may suffer from chronic diarrhea. Chronic diarrhea occurs in many underlying GI illnesses, and therefore appropriate evaluation of symptoms is vital. Malabsorptive disorders, such as lactose intolerance, celiac disease, or inflammatory bowel disease may result in chronic diarrhea. Assessment should identify the frequency of stools, duration of symptoms, and potential weight loss. Stool characteristics (i.e., watery, mucousal, or fatty) can aid in further evaluation of the pathogenesis of diarrhea. Secretory diarrhea occurs as a result of a disruption in electrolyte transport within the epithelium with resultant diarrhea. It may be caused by enterotoxins, intestinal resections or mucosal disease, or mesenteric ischemia due to atherosclerosis. Osmotic diarrhea occurs after ingestion of poorly absorbed cations and anions, such as sorbitol or sugar alcohols, magnesium sulfate, or phosphate, or may be related to deficiencies of disaccharidases, as in lactase deficiency.
In patients with chronic diarrhea, a comprehensive evaluation is necessary to determine the underlying cause. Management of diarrhea to prevent electrolyte abnormalities and potential weight loss is vital. Adequate fluids are also necessary to prevent dehydration, and oral rehydration solutions are beneficial to compensate for electrolyte losses. While diarrhea may be worsened by the intake of insoluble dietary fibers, soluble fibers may aid in improvement as they form a gel within the intestinal lumen, thus slowing intestinal transit. Sources of soluble and insoluble dietary fiber are reviewed in Table 7-5. After diarrhea resolves, patients may tolerate gradual reintroduction of insoluble dietary fiber, such as whole grain breads and cereals. Other foods that may worsen diarrhea, such as lactose-containing foods or high-fat foods, should be avoided until diarrhea begins to resolve. Evidence suggests that incorporating functional foods containing live, active bacterial cultures, such as yogurt, or probiotic supplements may be helpful in treating diarrhea associated with antibiotic use, acute infectious diarrhea, travelers’ diarrhea, and diarrhea-predominant irritable bowel syndrome. The most studied probiotic strains are Lactobacillus, Bifidobacterium, and Saccharomyces. However, recent studies have shown adverse outcomes associated with administration of probiotics to critically-ill hospitalized patients. The use of probiotic supplementation in this population is not recommended.
Table 7-5 Dietary Sources of Soluble and Insoluble Fiber
Source: Lisa Hark, PhD, RD and Darwin Deen, MD, 2014. Used with permission.
| Soluble Fiber | Insoluble Fiber |
|---|---|
| Apples Citrus fruits Strawberries Carrots Oats Beans Legumes Barley Fiber supplements: Psyllium (Metamucil) Guar gum (Benefiber) | Whole wheat flour Bran Vegetables Whole grains Wheat Fruits with edible seeds (strawberries, blueberries, etc.) |
A thorough medication history can identify potential drugs that may exacerbate diarrhea. Sorbitol or lactulose-containing medications should be adjusted if possible. Significant amounts of sorbitol and other sugar alcohols found in low carbohydrate or sugar-free foods can also play a role. Patients should be encouraged to eliminate these foods temporarily and assess for symptom resolution.
Constipation
Constipation is a common complaint with prevalence estimates of 12 to 19 percent in North America. Risk factors for constipation include advancing age and female gender, with women being twice as likely as men to report symptoms. Constipation is defined as less than two to three bowel movements per week and can be classified as primary constipation, which is caused by disordered movement of stool in the colon, or secondary constipation, which is caused by various systemic disorders or medications. Because the causes of constipation are varied, it is important to rule out structural causes of constipation as well as organic disease.
Nutrition therapy for constipation focuses on increasing fluid intake and gradually increasing fiber intake. It is important that patients are instructed to make gradual dietary changes, as rapid fluctuations in dietary fiber can worsen symptoms of constipation and abdominal discomfort. There is some debate over the efficacy of fiber in treatment of constipation. Recent studies have not shown an association between increasing fiber intake and improvement in symptoms of constipation. Some studies have even shown an increase in abdominal discomfort, such as bloating and distention, with an increase in fiber. This has lead healthcare professionals to recommend a moderate fiber intake in the form of soluble fiber for patients with constipation, in order to avoid a worsening of abdominal symptoms. Regardless of this recent debate, United States Dietary Guidelines recommend 25 to 35 g of fiber daily including fruits, vegetables, whole grains, legumes, and nuts. Clinicians should base their recommendations for fiber intake on individual patient tolerance. Treating constipation in the elderly, another high-risk group, should also involve dietary management that promotes appropriate increases in fluid and fiber intake. Assessment for other contributing factors including co-morbid conditions, decreased mobility, and inability to sit on the toilet should be considered (in the case of bed-bound patients) and should be evaluated by healthcare professionals (see Appendix O for high fiber foods).
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD), including both Crohn’s disease and ulcerative colitis, are idiopathic, chronic, inflammatory conditions affecting the GI tract. Crohn’s disease can involve any part of the digestive tract, while ulcerative colitis primarily involves the colon. Because of the chronic involvement of the GI tract, many patients with IBD, particularly those with Crohn’s disease, are at risk for specific nutritional deficiencies and malnutrition. Enteral nutrition may also be employed as a primary treatment modality for individuals with Crohn’s disease. Therefore, careful attention to diet and in-depth involvement of a gastroenterologist and registered dietitian are important components of the care of individuals with IBD. Dietary interventions in IBD should focus on maintaining or improving nutritional status through adequate intake, and avoiding foods that worsen symptoms. Table 7-6 outlines nutritional concerns, which should prompt involvement of a registered dietitian experienced in the management of individuals with IBD.
Table 7-6 Nutritional Concerns in Patients with Inflammatory Bowel Disease
Source: Julie Vandelpool, RD, 2014. Used with permission.
|
Protein-calorie malnutrition is common among patients with IBD and correlates with disease activity, which may be mediated by pro-inflammatory cytokines such as IL-1, IL-6, and tumor necrosis factor alpha. Nutrition assessment is essential because of the severe consequences of malnutrition, including growth failure and developmental impairment in children and teenagers, impaired wound and intestinal healing, weight loss with loss of muscle mass, metabolic bone disease, and increased susceptibility to infection in children and adults. In addition, a malnourished patient with IBD may present with defects in GI function that further limit the absorption and utilization of nutrients.
Causes of Malnutrition
Malnutrition occurs in patients suffering from IBD as a consequence of decreased dietary intake, increased nutrient losses, and increased nutrient requirements.
Decreased Dietary Intake
Inadequate dietary intake and poor appetite are the most important factors contributing to poor nutritional status in patients with IBD. GI symptoms such as nausea, diarrhea, and recurrent abdominal pain may lead to a decrease in appetite and a fear of eating. Disease-specific complications such as oral aphthous ulceration, gastritis, small intestinal inflammation, or intestinal strictures, may also contribute to inadequate dietary intake or increased symptoms. For example, patients with Crohn’s disease may experience impaction of high-fiber foods in an inflamed or fibrotic section of bowel, which can precipitate an obstruction. High-fat foods or spicy foods may worsen diarrhea. Some medications that may be used to treat IBD such as metronidazole, methotrexate, or sulfasalazine, may also decrease appetite. To maximize nutrient intake, unwarranted dietary restrictions should be avoided.
Increased Nutrient Losses
In patients with Crohn’s disease, small and large bowel inflammation, and/or multiple bowel resections can decrease the absorptive surface area of both the small and large intestine and cause malabsorption of essential nutrients. Resection of the ileum can cause bile salt deficiency, resulting in steatorrhea or fat malabsorption and subsequent deficiency of fat-soluble vitamins A, D, E, and K. Small intestinal bacterial overgrowth may also interfere with nutrient utilization.
Vitamin B12 is coupled with intrinsic factor, which is secreted by the parietal cells of the stomach. Because the vitamin B12–intrinsic factor complex is absorbed in the terminal ileum, complete ileal resection or prolonged inflammation of the terminal ileum may result in a vitamin B12 deficiency that requires treatment via subcutaneous or intramuscular injections, nasal spray, or sublingual vitamin B12.
IBD also can result in a protein-losing enteropathy through excessive intestinal transudate (movement of protein rich fluids through the inflamed bowel wall). In the case of Crohn’s disease, protein-rich fluid can also be lost through fistulas, particularly high-output fistulas. Severe diarrhea causes depletion of electrolytes, minerals, and trace elements, such as zinc. GI bleeding can also contribute to iron deficiency. Prednisone, which is frequently used during IBD flares, reduces calcium absorption and increases protein breakdown.
Increased Nutrient Requirements
The inflammatory process of IBD may increase resting energy expenditure, thereby contributing to weight loss and depletion of fat stores when patients do not consume adequate calories and protein. Patients with fever, infection, sepsis, and those undergoing surgery also have greater dietary requirements compared to patients who are less severely ill. Increased intestinal cell turnover can also raise nutrient requirements in patients with IBD.
Nutrition and Pathogenesis of IBD
With an observed increase in incidence of IBD, the potential role of diet in the pathogenesis of IBD has gained increasing attention. Recent studies have focused on dietary fat intake and the risk of IBD development. In a recent prospective study from Europe, individuals with a higher intake of linoleic acid had an increased risk of developing ulcerative colitis. Linoleic acid is metabolized to arachadonic acid, which can then be used to generate pro-inflammatory mediators. Linoleic acid is present in various dietary sources, including red meat, cooking oils, and margarines. A separate European study has illustrated that a diet high in animal protein is associated with an increased risk of development of IBD. Dietary sources including meat and fish, but not eggs or dairy products, was associated with an increase in development of IBD.
Nutrition Therapy for IBD
While dietary factors may play into the risk of development of IBD, no specific diet has been shown to prevent or treat IBD. However, some diet strategies help control symptoms. Nutritional recommendation must take into account the patient’s digestive and absorptive capabilities. They also depend on whether the patient is hospitalized in an acute flare-up or asymptomatic. Therefore, goals of nutrition therapy for patients with IBD are shown in Table 7-7.
Table 7-7 Nutrition Therapy Goals for Patients with IBD
Source: DeLegge.
|
Oral nutritional repletion may be difficult to achieve during symptomatic flares of active IBD since most patients’ symptoms worsen both during and following meals. To decrease both the symptoms associated with eating and bowel activity during the healing process, patients hospitalized for IBD are sometimes placed on bowel rest. Prolonged bowel rest without nutrition support can lead to nutritional depletion. Any hospitalized patient on bowel rest who is not anticipated to resume oral repletion within 7 days should be considered for total parenteral nutrition (TPN) (Chapter 13).
An oral diet may be tolerated when active IBD is less severe. To control diarrhea and malabsorption, a low-fat, low-fiber, low-lactose diet is often prescribed. Small, frequent feedings may help to limit GI secretions as well as reduce the volume of food that the damaged bowel must handle at any one time. During a flare, the diet should be individualized according to the patient’s clinical condition and food tolerances. While the dietary composition of fat and protein may serve as a risk factor for initial development of IBD, there is no data to suggest that specific dietary triggers can result in flare of established IBD. While certain foods have been associated with causing increased GI pain or other symptoms, they are not believed to cause disease relapses. Restriction of diet when individuals do not have active IBD is not encouraged because it can further limit nutrient intake unnecessarily (unless there is fixed narrowing in the lumen of the GI tract). General dietary recommendations for patients with IBD are listed in Table 7-8.
Table 7-8 Key Dietary Guidelines for Patients with Active IBD
Source: Brown.
|
Patients should be advised to eat foods based on tolerance; however, there are certain foods that can be discouraged because they offer few redeeming nutritional qualities and have been associated with intestinal distress (e.g., popcorn, seeds). This can also allow patients to feel they have more control over their disease. For those who are symptomatic, the goal is to liberalize the diet as much as possible after symptoms have subsided, under the guidelines of a dietitian and gastroenterologists.
Alcohol and caffeine can trigger diarrhea because they stimulate the GI tract; which often occurs within 30 minutes of consumption. Similarly, diet foods and beverages containing sugar alcohols, such as sorbitol, xylitol, and mannitol, can also cause intestinal discomfort and diarrhea, and patients should be encouraged to read labels and avoid these items. Though controversial, heavily spiced foods, fried foods, and concentrated sweets have also been associated with inducing diarrhea. Individuals who experience intense GI pain after eating, benefit from keeping a food diary to determine if any specific foods or beverages they consume may act as a GI irritant. A food diary is essential for patients to gain a better understanding of what foods they can or cannot tolerate. Food diaries can be simple and could include columns in a notebook for:
- type of food or beverage consumed,
- amount of the food or beverage consumed,
- where it was consumed (home, car, restaurant),
- time of day,
- symptoms.
Calories
In adults, ingested calories should be provided in amounts sufficient to maintain or restore bodyweight. In children, the amount of ingested calories should be adequate to support growth and development, as measured on the pediatric growth charts. Active disease and complications, such as fevers, infection, sepsis, and high output fistulas may increase caloric requirements in adults to as high as 35 to 45 kcal/kg per day, or approximately 1.5 to 1.7 times the basal energy expenditure. For example, a female patient with moderate to severe disease activity weighing 110 lb (50 kg) may require 1750 to 2250 kcal/day to maintain her weight. If a patient is severely malnourished and his or her calorie intake is low, the patient should be assessed by a registered dietitian to help determine the most appropriate feeding plan. Usually 20 to 25 kcal/kg per day may be initially prescribed to help avoid complications of refeeding syndrome. Supplemental calories can be given in the form of whole protein, elemental or semi-elemental products, and easy to metabolize MCT oils that do not require bile salts for digestion.
Protein
Protein needs are often increased in patients with IBD due to intestinal inflammation or presence of complications, such as abscesses in patients with Crohn’s disease. The majority of IBD patients have daily protein needs of 1.0 to 1.5 g/kg ideal body weight. For weight gain and to restore loss of lean body mass greater than 10 percent after an acute flare, protein needs may be increased up to 3.0 g/kg. Protein needs are also increased if the patient is taking prednisone.
Vitamins and Minerals
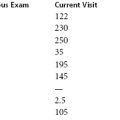
Patients with IBD are at higher risk for vitamin, mineral, and trace element deficiencies. Higher doses of specific nutrients are indicated if clinical or laboratory evidence identifies a deficiency due to possible poor absorption or increased requirements. Vitamin and mineral requirements for patients with IBD are described here and summarized in Table 7-9.
- Patients with Crohn’s disease who have extensive intestinal damage due to prolonged inflammation and/or have undergone resection of the terminal ileum are likely to suffer from inadequate vitamin B12 absorption. Small intestinal bacterial overgrowth may also occur in the setting of loss of the terminal ileum and ileocecal valve, and may predispose to vitamin B12 deficiency due to bacterial use of B12. Patients with Crohn’s disease may require supplementation with intramuscular, sublingual, or intranasal vitamin B12, if they fail to improve B12 levels following oral supplementation.
- IBD patients with persistent, watery diarrhea may have difficulty maintaining adequate zinc, potassium, and magnesium levels and may require supplementation.
- Chronic blood loss and altered iron intake and absorption, frequently observed in patients with IBD, can cause iron deficiency anemia. However, oral iron may cause symptoms of nausea, constipation, and abdominal cramping. Slower iron supplementation, given with ascorbic acid, may be more effective as ascorbic acid enhances the absorption of iron by converting the ferric ions to the ferrous form, which is absorbed primarily in the duodenum. Only 25 to 50 mg of ascorbic acid is needed daily to enhance the absorption of iron. Intravenous iron should be considered in individuals with severe anemia (hemoglobin < 10 g/dL), intolerance to oral iron supplementation, lack of improvement in hemoglobin (normalization or improvement in hemoglobin by 2 g/dL within 4 weeks), or severe intestinal inflammation.
- Patients treated with sulfasalazine (Azulfidine) should receive oral folate supplements, 1 mg/day, because this medication inhibits folate absorption by competitive inhibition of the enzyme folate conjugase in the jejunum. Mexthotrexate also requires folate supplementation at 1 mg daily because it is a folate antagonist (it inhibits the enzyme dihydrofolate reductase) and folate deficiencies may lead to stomatitis and anemia.
- If a patient is taking a bile salt sequestrant used to treat bile salt-induced diarrhea, fat-soluble vitamin deficiency (A, D, E, and K) may develop. Folate and magnesium absorption can also be impaired by bile salt sequestrants.
Table 7-9 Vitamin and Mineral Requirements for Patients with IBD
Source: adapted from Eiden.
| Nutrient | Recommended Daily Requirements | Recommended Replacement for Deficiency (Oral Dose) |
|---|---|---|
| inc | 15 mg | 50 mg elemental/day |
| Iron | 10–15 mg | 300 mg 3times/day |
| Vitamin B12 | 3 μg | 1000 μg /day |
| Calcium | 800–1500 mg | 1500–2000 mg/day |
| Magnesium | 400 mg | 150 mg elemental 4 times/day |
| Vitamin D | 1000 IU | 50,000 IU once weekly × 8 weeks |
Vitamin D and IBD
Vitamin D deficiency and bone demineralization is common in adults and children with IBD. Factors contributing to this include reduced dietary intake, infrequent sunlight exposure, and limited physical activity. Corticosteroid use contributes to bone demineralization, while decreasing calcium absorption and increasing calcium excretion. Research has also recently focused on a potential role for vitamin D in control of disease activity through immunomodulation and modification of the risk of IBD-associated malignancy. Serum concentration of 25-OH vitamin D should be monitored at least yearly in individuals with IBD, with a serum level of 32 ng/mL considered as a minimum level of sufficiency. Replacement strategies are listed in Table 7-9, with 50,000 IU of vitamin D given weekly for individuals with 25-OH vitamin D levels less than 20 ng/mL. Individuals with 25-OH vitamin D levels between 20 and 32 ng/mL may improve vitamin D levels with supplementation of 1000 to 2000 IU/day, but should be followed for normalization of vitamin D status.
Fiber
A low-fiber diet is often prescribed for patients with narrowed sections of bowel to decrease the possibility of intestinal obstruction, minimize physical irritation to the inflamed bowel, reduce stool weight and frequency, and slow the rate of intestinal transit. The diet consists of white bread and refined cereals and avoidance of high-fiber fresh fruits and vegetables, nuts, skins, and seeds. The benefit of a low-fiber diet in managing symptoms or affecting the course of IBD remains unclear. Diets should be recommended based on a patient’s individual tolerance and intolerance; intake of fiber-rich, nutrient-dense foods can generally be encouraged in the absence of bowel strictures and if there is no discomfort. A fiber rich diet should not be prescribed in patients with strictures (Crohn’s disease), as this could potentially contribute to a small bowel obstruction.
Fat
Decreased fat intake may help control the symptoms of steatorrhea, especially in patients with Crohn’s disease involving the small bowel. However, fats serve as a form of concentrated calories, which are needed to promote weight gain in underweight or malnourished patients. Dietary fats are also essential for the absorption of vitamins A, D, E, and K. In order to decrease diarrhea related to fat malabsorption, MCT oil can be substituted as it is more easily absorbed. MCT oil can be added to other foods, but this may change the palatability of the food. Doses should be given in less than 15-g amounts. Referral to a registered dietitian is essential for all patients requiring weight gain who present with fat malabsorption.
Inflammatory versus Anti-Inflammatory Fatty Acids
It has been demonstrated that gene mutations that affect the immune system, causing inflammation, are associated with IBD. Consequently, it has been hypothesized that the ratio of different polyunsaturated fats in the diet may play a role in helping to control inflammation. Western diets are often high in dietary intake of omega-6 fats (vegetable oils) compared to omega-3 fats. An increase in consumption of omega-3 fats and a decrease in omega-6 fats results in reduced arachidonic acid and it is hypothesized that reducing omega-6 fat sources and increasing omega-3 fatty acids results in a reduction of inflammation. However, there are insufficient data to recommend the use of omega-3 fatty acids in treatment of active IBD or in maintenance of remission in IBD. While research has not demonstrated that supplementation with omega-3 is beneficial in helping to sustain remission, food sources of omega-3 fats should be incorporated into a recommended balanced diet. Dietary sources of omega-3 fats include fatty fish, walnuts, soy, flaxseed, canola oil, and in small amounts, certain leafy greens and are listed in Appendix M.
Oxalate
Calcium oxalate kidney stones are a common complication in patients with Crohn’s disease who undergo intestinal surgeries such as ileal resection, or diverting ileostomy which can lead to bile salt malabsorption. Malabsorbed fat then binds intraluminal calcium, decreasing the amount of calcium bound to oxalate and an increase in intestinal and colonic absorption of free oxalate. Low levels of urinary magnesium and citrate may also contribute to a tendency to develop oxalate stones. Dietary modifications to prevent oxalate stones aim to increase intake of fluid, dietary calcium, potassium, magnesium, and phytates. Calcium supplementation may be given in forms of calcium carbonate or calcium citrate, as supplemental calcium will help bind intestinal oxalate; calcium citrate may also improve urinary citrate excretion (as urinary citrate inhibits stone formation). Dietary measures should also include reduced intake of oxalate and dietary fat. Oxalate rich foods to avoid include beets, turnip greens, rhubarb, strawberries, sweet potatoes, wheat bran, chocolate, tea, spinach, nuts, and citrus juices.
Prebiotics and Probiotics
Probiotics
The joint Food and Agriculture Organization (FAO) and World Health Organization (WHO) report on the evaluation of probiotics in food defines probiotics as “live microorganisms which when administered in adequate amounts confer a health benefit on the host.” While many products are labeled as probiotics, few of the commercially available products have been studied within a controlled experimental design. This concept is important, as the majority of probiotic effects are thought to be strain specific and should not be extrapolated from one strain to another, regardless of how closely related. The rationale for the use of probiotics in IBD stem from the thought that alteration in the intestinal microbiome predisposes one to IBD, and animal models which show anti-inflammatory properties of specific probiotic strains or soluble proteins from specific probiotic cultures. Despite this, clinical trials of probiotics in treatment of IBD have been mixed. Caution should be taken when prescribing probiotics to patients, as complications have been described in patients who are immunocompromised, have surgical short bowel syndrome, and patients who are critically ill.
Ulcerative colitis Various probiotic strains have shown promise in treatment of mild/moderate ulcerative colitis, largely in conjunction with standard medical therapy. However, studies are often limited by small sample sizes and various strains and dosing regimens of probiotics used. Two probiotic strains that have shown promise in induction and/or maintenance of remission of ulcerative colitis include VSL3 (probiotic preparation including four Lactobacillus species, three Bifidobacterium species, and one strain of Streptococcus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree