and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Introduction
Gastroenterological symptoms such as abdominal pain, nausea, vomiting, jaundice, diarrhoea, constipation and weight loss are common, and can be due to complications of SCD or to other common medical conditions, some of which are more frequent in SCD. Table 13.1 lists the most important gastroenterological complications together with their clinical features, laboratory and radiological findings.
Table 13.1
Gastroenterological complications of sickle cell disease-clinical features, laboratory and radiological findings.
Clinical features | Investigations | |
|---|---|---|
Directly related to SCD | ||
Abdominal sickle crisis (‘girdle crisis’) | History: Acute onset diffuse abdominal pain and tenderness, often associated with bony pain. Examination: abdominal distension, scanty bowel sounds. | Reduced Hb with reticulocytosis. |
AXR : Distended small and large bowel loops. | ||
Acute splenic sequestration(See Chap. 11) | History: Acute onset left upper quadrant pain, lethargy . Examination: Pallor, jaundice, spleen palpable and becoming larger, often tender. | Reduced Hb with reticulocytosis. |
Usual presentation is in infants, but also in older children and adults with milder phenotypes of SCD | AUS (not essential if diagnosis obvious): Enlarged spleen | |
Acute hepatic sequestration | History: Acute onset right upper quadrant pain, fatigue, often associated with an acute painful crisis. Examination: pallor, jaundice, abdominal distension, liver palpable and rapidly enlarging. | Reduced Hb with reticulocytosis. Increased bilirubin, increased AST, ALT, Alk Phos, gamma GT. |
Seen in older children, adolescents and adults | AUS: Enlarged liver | |
Hepatic crisis/hepatopathy/intrahepatic cholestasis | Acute, sub-acute or chronic presentation. Features may be similar or overlapping with acute hepatic sequestration. Commoner in older adults | Reduced Hb with reticulocytosis. Very high bilirubin, and increased AST, ALT, Alk Phos, gamma GT persisting during steady state. |
AUS: Enlarged liver, intrahepatic ducts may be distended, with thickened irregular walls. | ||
Causes indirectly related to SCD | ||
Gall-stone related problems: Acute biliary colic, obstructive jaundice, acute cholecystisis, acute pancreatitis | History: Right upper quadrant or epigastric pain, may be colicy. Dark urine, pale stool. | Increased bilirubin, increased AST, ALT, Alk Phos, gamma GT. Amylase raised in acute pancreatitis. |
Examination: Jaundice. May have fever, pallor. Epigastric and right upper quadrant tenderness | AUS: Gallstone (s) in gallbladder and/or biliary tree. Thickened edematous gallbladder wall, dilated intrahepatic and/or extrahepatic bile ducts. Pancreas may appear inflamed | |
Gastritis, peptic ulceration | Predominantly epigastric pain. May be episodic and predominantly at night. May be a history of chronic use of non-steroidal anti-inflammatory drugs | Hematology and biochemistry usually unchanged from steady state. Normal AUS. Gastritis or ulcer demonstrated on upper GI endoscopy |
Constipation | Common in children and adults and may be the sole cause of abdominal pain. May be related to diet, opioid analgesic use, pica, or abdominal sickling | AXR shows faecal loading, but not advised routinely because of radiation dose |
Acute pyelonephritis | Fever, loin pain and tenderness | Perturbation of steady state hematology and biochemistry tests if accompanied by disseminated sepsis or intercurrent acute crisis |
Abdominal Crisis (Girdle Syndrome, Mesenteric Sickling)
The abdomen is a common site of pain during acute painful crisis, particularly in children. A more severe form of abdominal crisis is sometimes referred to as ‘girdle syndrome’, the clinical and radiological features of which are listed in Table 13.1.
Incidence
In our experience girdle syndrome is commoner in children and usually develops during the course of an acute painful crisis.
Etiology
It is thought to be due to vaso-occlusion and sequestration in the small vessels of the mesentery, giving rise to abnormal bowel perfusion, transient dysfunction and pain due to ischemia.
Clinical Features
Pain may be restricted to the abdomen, but it is often accompanied by bone pain in the limbs, chest and/or back. There may be additional gastro-intestinal symptoms such as nausea, anorexia and patients usually recognise the pain as being similar to an acute painful crisis. This contrasts with presentations due to a surgical cause, where the pain is recognised as different.
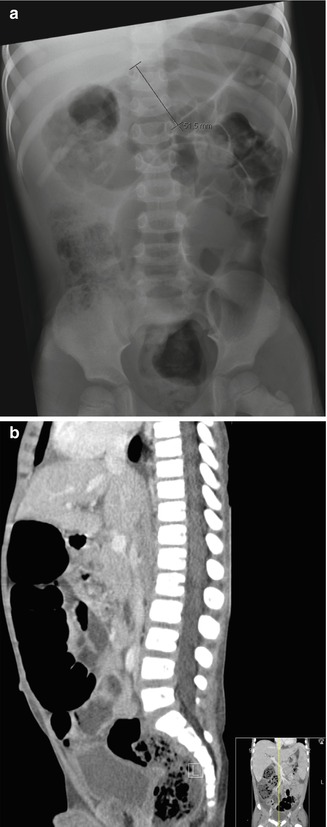
There may be a distended abdomen with very scanty or absent bowel sounds and dilated bowel on abdominal X-ray. The large bowel tends to be the predominant site of dilatation, and this is often accompanied by faecal loading in the distal colon (Figure 13.1). There is usually a drop in hemoglobin with reticulocytosis, presumably reflecting increased hemolysis and mesenteric sequestration of red cells.