Considerable progress has been recently made in the treatment of elderly patients with multiple myeloma (MM). In Europe the combination of thalidomide with melphalan and prednisone and of bortezomib with melphalan and prednisone are 2 standards of care for frontline therapy for elderly patients. In United States the combination of lenalidomide and dexamethasone is the preferred option in this setting. This article focuses on more recent therapeutic approaches in older MM patients, not eligible for high-dose therapy and autologous stem cell transplantation.
Key points
- •
Considerable progress has been recently made in the treatment of elderly patients with multiple myeloma (MM).
- •
In Europe the combination of thalidomide with melphalan and prednisone and of bortezomib with melphalan and prednisone are 2 standards of care for frontline therapy for elderly patients.
- •
In United States the combination of lenalidomide and dexamethasone is the preferred option in this setting.
Introduction
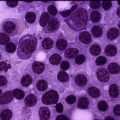
Multiple myeloma (MM) accounts for 1% of all cancers and approximately 13% of all hematologic malignancies. Approximately 86,000 new cases of MM occur annually worldwide. This malignant neoplasm affects primarily elderly patients with a median age at the time of diagnosis of about 70 years. Approximately two-thirds of patients are older than 65 years and one-third older than 75 years. Patients older than 65 years, who represent most of the newly diagnosed symptomatic cases, are generally considered ineligible for autologous stem cell transplantation (ASCT). During the past decade, considerable progress has been made in the treatment of MM. In the group of elderly patients, newer regimens and therapies that increase overall response and even complete remission rates have been evaluated in phase II and III trials. Before the introduction of novel agents, combination chemotherapy with melphalan and prednisone (MP) had been the standard treatment approach for elderly myeloma patients since the 1960s. The addition of thalidomide to this regimen (MPT) was the first step leading to survival improvement. Subsequently, bortezomib was added to MP (VMP), and this VMP regimen also showed a survival benefit over MP. These 2 regimens, MPT and VMP, are the most widely used combinations in Europe. In the United States, a melphalan-free regimen has been developed, combining lenalidomide and low-dose dexamethasone (Rd), and this has shown favorable results. The Rd combination has recently been compared with MPT in a large international prospective randomized trial, and this regimen will become another standard of care in the near future. This article focuses on more recent therapeutic approaches in older MM patients, not eligible for high-dose therapy and ASCT.
Introduction
Multiple myeloma (MM) accounts for 1% of all cancers and approximately 13% of all hematologic malignancies. Approximately 86,000 new cases of MM occur annually worldwide. This malignant neoplasm affects primarily elderly patients with a median age at the time of diagnosis of about 70 years. Approximately two-thirds of patients are older than 65 years and one-third older than 75 years. Patients older than 65 years, who represent most of the newly diagnosed symptomatic cases, are generally considered ineligible for autologous stem cell transplantation (ASCT). During the past decade, considerable progress has been made in the treatment of MM. In the group of elderly patients, newer regimens and therapies that increase overall response and even complete remission rates have been evaluated in phase II and III trials. Before the introduction of novel agents, combination chemotherapy with melphalan and prednisone (MP) had been the standard treatment approach for elderly myeloma patients since the 1960s. The addition of thalidomide to this regimen (MPT) was the first step leading to survival improvement. Subsequently, bortezomib was added to MP (VMP), and this VMP regimen also showed a survival benefit over MP. These 2 regimens, MPT and VMP, are the most widely used combinations in Europe. In the United States, a melphalan-free regimen has been developed, combining lenalidomide and low-dose dexamethasone (Rd), and this has shown favorable results. The Rd combination has recently been compared with MPT in a large international prospective randomized trial, and this regimen will become another standard of care in the near future. This article focuses on more recent therapeutic approaches in older MM patients, not eligible for high-dose therapy and ASCT.
Thalidomide-based regimens
Thalidomide-Dexamethasone
Thalidomide combined with dexamethasone (TD) has been compared prospectively to high-dose dexamethasone (RD) and was superior in terms of partial response (63% vs 41%) and time to progression (TTP) (22.6 vs 6.5 months), but was found to be more toxic. Similarly, TD was superior to MP for responses, but progression-free survival (PFS) was similar, and overall survival (OS) was shorter. Therefore, the TD regimen is not considered to be among the main options for the frontline therapy for elderly patients.
Melphalan-Prednisone-Thalidomide
Six randomized studies have compared MPT with MP alone. Despite differences in doses and schedules among the trials, better responses and PFS were reported with MPT in all of these. The effect on OS varied across the studies, and only 2 trials showed a significant survival benefit. In a meta-analysis of individual data from 1682 patients, MPT improved PFS by 5.4 months (median 20.3 vs 14.9 months, respectively) and OS by 6.6 months versus MP (median 39.3 vs 32.7 months, respectively). The benefit of MPT has to be balanced against the increased risks of toxic effects. MPT is associated with higher risks of thromboembolism and peripheral neuropathy than MP, but these adverse events are manageable. The introduction of systematic anticoagulant prophylaxis has considerably reduced the rate of thromboembolism to less than 5%. Similarly, improvements in the management of neuropathy have been observed. Prompt reduction of thalidomide dose is recommended as soon as symptoms occur. Discontinuation of the drug is necessary when paresthesia is accompanied by pain, motor deficit, or interference with daily functions. Other thalidomide-related adverse events include cytopenia and fatigue. The MPT regimen was approved by the European Medicines agency in 2008 and is considered one of the standards of care in elderly patients. This combination, oral and cost-effective, is recommended by United States and European guidelines, as well as the International Myeloma Working Group (IMWG).
Cyclophosphamide-Thalidomide-Dexamethasone
An attenuated regimen of cyclophosphamide, thalidomide, and dexamethasone (CTD) has been prospectively compared with MP in a large randomized study (MRC IX) in the United Kingdom in 856 patients with newly diagnosed MM ineligible for ASCT. The overall response rate was significantly higher with CTD than MP (63.8% vs 32.6%), with a complete response (CR) rate of 13.1% versus 2.4%. No differences in PFS and OS were observed between the 2 groups. Therefore, the CTD regimen, although oral and cost-effective, is not routinely recommended as part of frontline therapy in elderly patients.
Bortezomib-based regimens
Bortezomib-Melphalan-Prednisone
Preclinical trials have demonstrated in vitro synergy when bortezomib, the first proteasome inhibitor, is combined with melphalan. The phase I/II study of VMP in 60 newly diagnosed elderly MM patients, which was reported in 2006 by the Spanish group PETHEMA, was conducted to identify the most appropriate dose of bortezomib in combination with the standard MP regimen (phase I) and to determine the efficacy of bortezomib + MP in terms of response rate (phase II). The VMP response rate was 89%, including 32% immunofixation-negative CRs, and the median TTP with VMP was 27.2 months. The 1.3 mg/m 2 intravenous bortezomib dose level was selected, with a biweekly administration of the drug. These impressive preliminary results were the basis for the prospective, randomized phase III VISTA (Velcade as Initial Standard Therapy) trial comparing MP with VMP. Six hundred eighty-two patients 65 years of age or older, not transplant eligible, and with untreated MM were randomized to receive MP for nine 6-week cycles (n = 338) or the VMP combination (n = 344). The total duration of treatment was 54 weeks in both arms of the study. Response rates were higher in the VMP arm (30% vs 4%); the median TTP was 24 months in the VMP arm versus 16.6 months in the MP arm; and with a median follow-up of 16 months, OS was also significantly in favor of the VMP arm. This improvement was also observed in patients older than 75 years. The final analysis was published in 2013 and confirmed that there was a 31% reduced risk of death with VMP versus MP, which was maintained after a median follow-up of 5 years and despite substantial use of novel-agent–based salvage therapies. VMP, although manageable, was more toxic than MP with a discontinuation rate of 34%. The most frequent grade 3 to 4 toxicities were neutropenia (40%), thrombocytopenia (37%), peripheral neuropathy (17%), and infections (10%). The efficacy results led to the approval of the VMP combination by the European authorities in 2008, and this regimen is also considered one of the standards of care in the frontline treatment of elderly patients and is currently recommended in United States and European guidelines, as well as in the IMWG consensus.
VMP Modified
When the twice-per-week bortezomib administration schedule was reduced to once per week in 2 prospective trials conducted in Spain and Italy, the rate of grade 3 to 4 peripheral neuropathy was found to be significantly lower, 17% versus 8%, respectively, whereas efficacy was comparable with the 2 schedules. In the Spanish trial, melphalan in the VMP regimen was substituted by thalidomide, and the combination of bortezomib-thalidomide-prednisone (VTP) was prospectively compared with VMP in 260 patients. This VTP regimen yielded similar response rates and survival outcomes as compared with VMP, but was associated with more serious adverse events and discontinuations. A more intensive approach was used in the Italian trial in which VMP was compared with the 4-drug combination of VMP plus thalidomide (VMPT) in 511 patients and with a once-weekly bortezomib infusion. Maintenance with thalidomide and bortezomib (VT) was administered in the VMPT, but not in the VMP arm. The VMPT-VT arm (nine 5-week cycles of VMPT followed by 2 years of VT maintenance) demonstrated better responses (38% CR vs 24%) and an improvement in 3-year PFS from 41% to 56% compared with VMP, but the efficacy advantage was mainly reported in fit patients aged 65 to 75 years old. The updated results of this trial were recently published and have shown that the 5-year OS was greater with VMPT-VT (61%) than with VMP (51%; hazard ratio, 0.70; P = .01). Despite positive results and recommendations from the IMWG, this 4-drug induction regimen followed by 2 years of maintenance is not routinely used as part of frontline therapy in elderly patients.
Recently, bortezomib administered subcutaneously was shown to be as effective as the intravenous route of administration, with a reduced risk of peripheral neuropathy. Therefore, subcutaneous bortezomib is now considered as a routine and feasible treatment of elderly patients and can be an option for prolonged therapy.
Bortezomib-Cyclophosphamide-Dexamethasone, Bortezomib-Lenalidomide-Dexamethasone
Interesting results have been obtained when cyclophosphamide (VCD) or lenalidomide (VRD) were combined with bortezomib and RD, producing high-quality responses. Although VRD and VCD have not been evaluated in randomized phase III trials, these 2 regimens are commonly used in the United States in clinical practice on the basis of positive results from phase II studies. VCD adds neither cost nor significant toxicity to the VD regimen, and the addition of cyclophosphamide allows for a weekly rather than twice weekly administration of bortezomib. In a phase II randomized trial, VCD had similar activity compared with VRD. Despite the lack of phase III data, these 2 regimens are recommended by the IMWG and by the US guidelines. VCD is the most cost-effective option.
Lenalidomide-based regimens
Lenalidomide–Low-dose Dexamethasone
Lenalidomide, an oral drug, is an analogue of thalidomide, which was designed to improve efficacy and tolerability over the parent drug. Lenalidomide has a safety profile that is distinct from that of thalidomide, with fewer neurologic symptoms but more myelosuppression. A phase III trial conducted by the ECOG (ECOG E4A03) assessed the safety and efficacy of lenalidomide plus high-dose RD versus lenalidomide plus low-dose dexamethasone (Rd) in 445 patients. The median age of the patient population was 66 years, and 233 patients were older than 65 years (up to 88 years). Patients eligible for ASCT could discontinue therapy after 4 induction cycles. Patients treated with RD had a higher overall response rate (79% vs 68%) but a lower 1-year OS (87% vs 96%). For patients aged older than 65 years, the 1-year OS rate was 83% with RD and 94% with Rd. RD was associated with a higher incidence of grade 3 to 4 nonhematological adverse events when compared with Rd, particularly deep-vein thrombosis (26% vs 12%), infections (16% vs 9%), and fatigue (15% vs 9%). In routine practice, all patients treated with Rd require antithrombosis prophylaxis. Aspirin is adequate for most patients, but in patients who are at a higher risk of thrombosis, either low-molecular-weight heparin or Coumadin is needed. In the ECOG study Rd was associated with a reduction in the rates of discontinuation and of early death compared with RD. The 3-year OS rate with Rd in patients aged 70 years and older who did not receive ASCT was 70%, which seems to be comparable to what is achieved with VMP or MPT. Therefore, the oral combination of Rd is widely used in the United States and is currently recommended by US guidelines, and by the experts from IMWG, but it is not approved in the Europe.
In the most remarkable recent study involving 1623 patients not eligible for transplantation (IFM07–01, MM020 trial), the combination of Rd administered until disease progression or intolerance (continued Rd) was compared with MPT administered for 12 cycles (72 weeks) or Rd administered for 18 cycles (72 weeks) (Rd18). The trial revealed a significant benefit of continued Rd over Rd18 and MPT and a significant increase in OS over MPT. With a median follow-up of 37 months, the median PFS was 25.5 months for continued Rd compared with 20.7 months with Rd18 and 21.2 months for MPT (continued Rd vs MPT: P = .0006, continued Rd vs Rd18: P = .0001). Four-year OS was 59.4% for continued Rd, 55.7% for Rd18 and 51.4% for MPT (continued Rd vs MPT: P = .017, continued Rd vs Rd18: P = .307). Given the significant improvement in survival, the relatively acceptable toxicity, and the ease of administration of continued Rd, this combination will likely become a frequently used protocol and another standard of care in elderly patients in the near future.
Melphalan-Prednisone-Lenalidomide
The combination of melphalan, prednisone, and lenalidomide (MPR) has been investigated in a dose-escalating Phase I/II study, which enrolled 54 patients (median age 71 years). They received 9 cycles of lenalidomide plus melphalan and prednisone every 6 weeks, followed by maintenance therapy with lenalidomide alone (10 mg/d, days 1–21, every month). The maximum tolerated dose was lenalidomide 10 mg/d for 21 days and melphalan 0.18 mg/kg for 4 days every 6 weeks. At this dose level, the overall response rate was 81%, including 24% of patients with immunofixation-negative CR. The 1-year event-free survival and OS rates were 92% and 100%, respectively. Overall, MPR was considered a promising first-line treatment of elderly patients, and these results formed the basis for an international randomized trial comparing MPR followed by lenalidomide maintenance (MPR-R) to MPR and MP (MM015 study). MPR-R resulted in a higher overall response rate compared with MPR and MP (77% vs 68% vs 50%). Furthermore, MPR-R reduced the risk of disease progression by 60% compared with MP. The median PFS was 31 months in the MPR-R arm versus 14 and 13 months in the MPR and MP arms, respectively. The PFS benefit associated with MPR-R treatment was evidenced especially in patients aged 65 to 75 years of age. No difference was observed in terms of OS when comparing the 3 arms of the study. Lenalidomide maintenance was well tolerated with no evidence of cumulative toxicity and low rates of adverse events. The most frequent hematologic adverse events in the MPR-R arm were neutropenia (35%) and thrombocytopenia (11%). Infections were the most frequent nonhematologic adverse events (9%), whereas a low rate of deep-vein thrombosis was observed (1%) because patients received aspirin prophylaxis as part of the protocol. MPR-R is currently considered a reasonable option in elderly patients with de novo MM by the experts of the IMWG, but the regimen is not approved in Europe and not widely used in the United States where Rd is the preferred option.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree