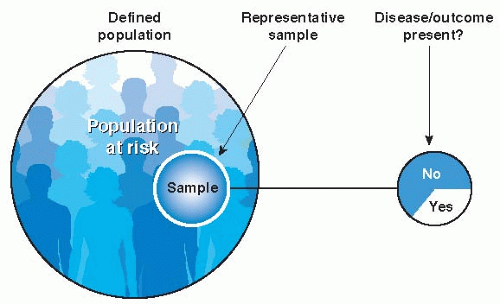
In general, clinically relevant measures of frequency are expressed as proportions, in which the numerator is the number of patients experiencing an event (cases) and the denominator is the number of people in whom the event could have occurred (population). The two basic measures of frequency are prevalence and incidence.
Incidence
Incidence is the fraction or proportion of a group of people initially free of the outcome of interest that develops the condition over a given period of time. Incidence refers then to new cases of disease occurring in a population initially free of the disease or new outcomes such as symptoms or complications occurring in patients with a disease who are initially free of these problems.
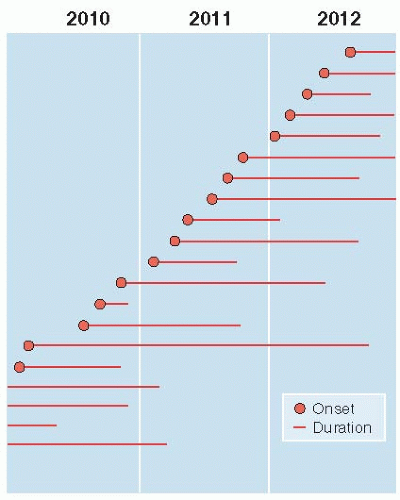
Figure 2.1 illustrates the differences between incidence and prevalence. It shows the occurrence of
lung cancer in a population of 10,000 people over the course of 3 years (2010-2012). As time passes, individuals in the population develop the disease. They remain in this state until they either recover or die—in the case of lung cancer, they usually die. Four people already had lung cancer before 2010, and 16 people developed it during the 3 years of observation. The rest of the original 10,000 people have not had lung cancer during these 3 years and do not appear in the figure.
To calculate prevalence of lung cancer at the beginning of 2010, four cases already existed, so the prevalence at that point in time is 4/10,000. If all surviving people are examined at the beginning of each year, one can compute the prevalence at those points in time. At the beginning of 2011, the prevalence is 5/9,996 because two of the pre-2010 patients are still alive, as are three other people who developed lung cancer in 2010; the denominator is reduced by the 4 patients who died before 2011. Prevalence can be computed for each of the other two annual examinations and is 7/9,992 at the beginning of 2011 and 5/9,986 at the beginning of 2012.
To calculate the incidence of new cases developing in the population, we consider only the 9,996 people free of the disease at the beginning of 2010 and what happens to them over the next 3 years. Five new lung cancers developed in 2010, six developed in 2011, and five additional lung cancers developed in 2012. The 3-year incidence of the disease is all new cases developing in the 3 years (16) divided by the number of susceptible individuals at the beginning of the follow-up period (9,996), or 16/9,996 in 3 years. What are the annual incidences for 2010, 2011, and 2012? Remembering to remove the previous cases from the denominator (they are no longer at risk of developing lung cancer), we would calculate the annual incidences as 5/9,996 in 2010, 6/9,991 in 2011, and 5/9,985 in 2012.
Prevalence and Incidence in Relation to Time
Every measure of disease frequency necessarily contains some indication of time. With measures of prevalence, time is assumed to be instantaneous, as in a single frame from a motion picture film. Prevalence depicts the situation at that point in time for each patient, even though it may, in reality, have taken several months to collect observations on the various people in the population. However, for incidence, time is the interval during which susceptible people were observed for the emergence of the event of interest.
Table 2.1 summarizes the characteristics of incidence and prevalence.
Why is it important to know the difference between prevalence and incidence? Because they answer two entirely different questions: on the one hand, “What proportion of a group of people has a condition?”; and on the other, “At what rate do new cases arise in a defined population as time passes?” The answer to one question cannot be obtained directly from the answer to the other.