Guildelines for the Diagnosis and Outpatient Management of Diabetic Peripheral Neuropathy*
Guidelines on the out-patient management of diabetic peripheral neuropathy have been developed from an international consensus meeting attended by diabetologists, neurologists, primary care physicians, podiatrists and diabetes specialist nurses. A copy of the full document follows this summary (Appendix 1). The document arose out of suggestions from Neurodiab, a subgroup of the European Association for the Study of Diabetes, that there was a need for guidelines developed by consensus, for the outpatient management of patients with diabetic neuropathy. An international consensus group was created, chaired by two of the authors. A pilot working party met in 1995, followed by a full working party of 39 experts, neurologists and diabetes physicians (Appendix 2). This compiled a draft guideline document which was circulated to a number of international bodies. After consultation with its members, the final guidelines were approved by Neurodiab (chairman F.A. Gries) towards the end of 1997.
Definition
Diabetes peripheral neuropathy: the presence of symptoms and/or signs of peripheral nerve dysfunction in people with diabetes, after exclusion of other causes (Table 1).
 Assessment as Part of the Annual Review of the Patient
Assessment as Part of the Annual Review of the Patient
Patient history: age, diabetes, physical factors, lifestyle, social circumstances, symptoms, other possible aetiological factors.
Examination should include:
• Inspection of both feet (Table 2): skin status, sweating, infection, ulceration, calluses/blistering, deformity, muscle wasting, arches; palpation for temperature, pulses, joint mobility; examine gait/shoes
• Vascular examination – foot pulses
• Other investigations, e.g. thyroid function, to exclude non-diabetic aetiologies
• Inspection for the presence or absence of characteristics of the “at risk” foot (Figure 1).
Table 1 Stages of diabetic peripheral neuropathy
Stage of neuropathy | Characteristics |
|---|---|
No neuropathy Clinical neuropathy | No symptoms or signs |
Chronic painful | Burning, shooting, stabbing pains ±pins and needles; increased at night; absent sensation to several modalities; reduced/absent reflexes |
Acute painful | Severe symptoms as above (hyperaesthesia common); may follow initiation of insulin in poorly controlled diabetes; signs minor or absent |
Painless with complete/partial sensory loss | Numbness/deadness of feet or no symptoms; painless injury; reduced/absent sensation; reduced thermal sensitivity; absent reflexes |
Late complications | Foot lesions; neuropathic deformity; non-traumatic amputation |
1. Types of diabetic neuropathy: frequent, sensorimotor symmetrical neuropathy (mostly chronic, sensory loos or pain), autonomic neuropathy (history of impotence and possibly other autonomic abnormalities); rare, mononeuropathy (motor involvement, acute onset, may be painful), diabetic amyotrophy (weakness/wasting usually of proximal lower limb muscles).
2. Staging does not imply automatic progression to the next stage. The aim is to prevent, or at least delay, progression to the next stage.
Table 2 Foot tests
Pin prick test | • Use a disposable instrument, e.g. a disposable pin • Ask “Is It painful?” not “Can you feel it?” |
Light touch | • Use a consistent method, ideally a cotton wisp |
Vibration test | • Use a 128 Hz tuning fork, initially on the big toe |
Pressure perception | • Absence of sensation in the foot to a 10 g monofilament |
Ankle reflex | • Compare the ankle reflex with the knee reflex |
Management
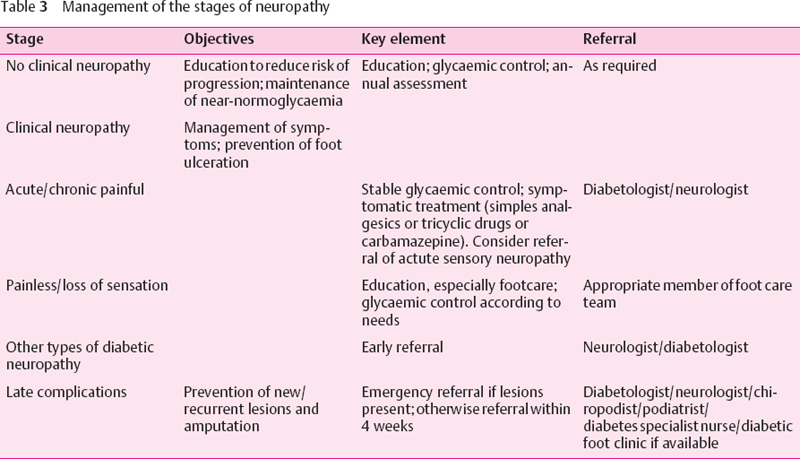
Education of people with clinical neuropathy and referral of people with late complications to a diabetologist or neurologist are the key factors in the prevention of amputation (Table 3). Prompt referral (same day/next available day) of the person with the following lesions will usually prevent amputation: ulcer, blister, bleeding callus, cellulitis, acute ischaemia.
Appendix 1: International Guide on the Outpatient Management of Diabetic Peripheral Neuropathy
Developed form discussions at a meeting of a Pilot Working Party held in Brussels, Belgium, on 13 April 1995 and a meeting of a full Working Party held in London, UK, on 20-22 October 1995.
 Introduction
Introduction
Lack of awareness and inappropriate management of diabetic peripheral neuropathy leads to unnecessary morbidity and substantial healthcare costs. At least half of the foot ulcers, the end stage of such neuropathy, should be preventable, by appropriate management and patient education. However, lack of time and inadequate knowledge and information may lead, in many cases, to suboptimal management.
There is a clear need for a set of simple, practical, international guidelines to be used by primary care physicians (in many countries, 80–90% of people with diabetes receive care from general practitioners) and by hospital physicians for the clinical assessment and management of neuropathy. The guidelines should be applicable in day-to-day practice and should use readily available methods.
The neuropathy study group (Neurdiab) of the European Association for the Study of Diabetes (EASD) has identified the need for three sets of guidelines for diabetic peripheral neuropathy. These will cover the following areas:
• studies of the epidemiology of peripheral and autonomic diabetic neuropathy (DN)
• conduct of clinical trials in DN
• management of diabetic peripheral neuropathy by practising clinicians.
The International Guidelines on the Outpatient Management of Diabetic Peripheral Neuropathy have been developed to fulfil the third need.
The purpose of this document is to provide clear, internationally acceptable guidelines on the clinical diagnosis and management of diabetic peripheral neuropathy in primary or hospital care, the widespread adoption of which would bring about earlier diagnosis, better management, and a reduction in the late sequelae of this complication of diabetes.
The guidelines provide recommendations on methods of assesment and management of diabetic peripheral neuropathy and patient education, all of which should form part of the annual review of people with diabetes. A simple staging system has been developed for diabetic peripheral neuropathy to provide a framework for risk assessment and decisions on treatment and referral of those with diabetes. The emphasis is on simplicity and practicality to facilitate maximal adoption. It is intended that the guidelines should be used by physicians involved in the outpatient management of the person with diabetes. In addition, the guidelines emphasize the concept of a multidisciplinary diabetes footcare team and it is expected that the team members would use those sections that are applicable to their discipline. Clearly, there are variations in the epidemiology of diabetes, economic and cultural factors and healthcare personnel in different geographical regions; therefore, the guideline should be adapted to meet local needs and conditions.
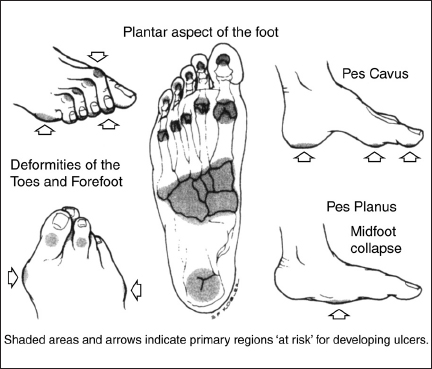
Fig. 1 The “at risk” diabetic foot (illustration by G. Kogler).
Peripheral Neuropathy in Diabetes
People with diabetes mellitus develop several types of peripheral neuropathy, including a distal sensory motor polyneuropathy, autonomic neuropathy, and mononeuropathy. The sensory motor polyneuropathy is the most common form of diabetic peripheral neuropathy and is the main focus of these guidelines. Estimates of its prevalence vary, although it is generally accepted that clinical diabetic peripheral neuropathy is found in approximately 30% of people with diabetes. In the USA, the risk of fool ulceration, a late complication of neuropathy, has been estimated to be 3% per patient per year. Neuropathy is also a major contributory factor in amputation. The incidence of amputation varies from country to country, owing to differences in the management of diabetes and diabetic foot disease. It is estimated, however, that 40% of non-traumatic foot and leg amputations in adults are due to diabetes.
There is an urgent need for improvement of the clinical management of neuropathy in primary care. At least half of the amputations in people with diabetes are believed to be preventable, yet there are still reports of people presenting with foot ulcera in whom diabetes, let alone neuropathy, has not been diagnosed. Neuropathy also has a major impact on healthcare costs. In the USA it is estimated that the cost of the sequelae of neuropathy, foot ulcers, and amputations is equal to the entire cost of the remainder of diabetes management.
Guidance for the primary care physician is lacking. In addition, the physician has limited time available for consultation with the patient with diabetes. It is the objective of this document, therefore, to provide clear and simple guidelines for the diagnosis and management of neuropathy on an outpatint basis, in particular during the annual review of the patient. The emphasis is on simple diagnostic testing, using equipment that is readily available. Although much can be done in primary care to manage and educate people with diabetes, guidance is also given on when it is appropriate to refer the patient to a member of the multi-disciplinary diabetes footcare team. The availability of resources will vary in different locations and it is possible that some reorganization or modification of referral procedures may be required to achieve optimal management.
Adoption of the guidelines should lead to improvements in the management of and this should be documented. Systems should, therefore, be established to monitor the implementation of the recommended practices and to assess their impact, in terms of reduction of the incidence of foot ulceration and amputation, in people with diabetes.
 Definitions
Definitions
Diabetic peripheral neuropathy is the presence of symptoms and/or signs of peripheral nerve dysfunction in people with diabetes, after exclusion of other causes.
Stages of Neuropathy
A staging system has been developed for neuropathy to provide a framework for diagnosis and management. Staging does not imply automatic progression to the next stage and the aim is to prevent, or at least delay, progression (Table A1).
Table A1 The stages of neuropathy
Stage | Characteristics |
|---|---|
Stages 0/1: no clinical neuropathy | • No symptoms or signs |
Stage 2: clinical neuropathy Chronic painful | • Positive symptomatology (increasing at night): burning, shooting, stabbing pains ± pins and needles • Absent sensation to several modalities and reduced or absent reflexes |
Acute painful | • Less common • Diabetes poorly controlled, weight loss • Diffuse (trunk) • Hyperaesthesia may occur • May be associated with initiation of glycaemic therapy • Minor sensory signs or even normal peripheral neurological examination |
Painless with complete/partial sensory loss | • No symptoms or numbness/deadness of feet; reduced thermal sensitivity; painless injury • Signs of reduced or absent sensation with absent reflexes |
Stages 3: late complications of clinical neuropathy | • Foot lesions e. g. ulcers • Neuropathic deformity e. g. Charcot joint • Non-traumatic amputation |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







