Foot and Ankle Amputations: Ray Resections and Lisfranc/Chopart
Braden J. Criswell
Yvette Ho
Martin M. Malawer
Loretta B. Chou
BACKGROUND
Malignant tumors of the foot present a significant and formidable challenge to the orthopaedic oncologist due to the foot’s unique function and anatomic peculiarities.
Both bone and soft tissue contribute to the structure and function of the foot. Furthermore, the foot is composed of compact compartments that are interconnected by nerves and vascular structures. Complete resection (wide local excision) of osseous structures of the foot is difficult because of the interruption of these complex anatomic relationships, which afford stability to the foot, in addition to the interconnected compartments. Malignant tumors of bone are rare in the foot and rarer still in locations distal to the metatarsophalangeal joints.5,9,12,14,17,18 Many of these tumors are treated with amputations.
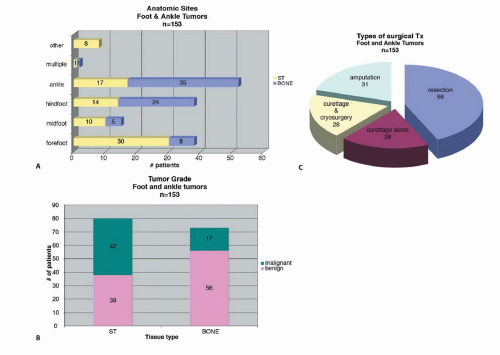
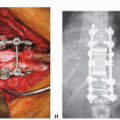
FIG 1A shows all anatomic sites, FIG 1B shows the distribution of malignant and benign cases, and FIG 1C shows the distribution of all types of surgical procedures.
In the senior author’s experience of foot and ankle tumors in 153 cases, 31 amputations were performed (see FIG 1C). Fortunately, tumors distal to the metatarsophalangeal joint can be treated by amputation through the metatarsophalangeal joint with minimal disruption to function. The only exception is the first ray, which typically bears 50% of the weight with toe-off during each gait cycle. Therefore, preservation of as much proximal phalanx as possible is important to optimize this important structure.
ANATOMY
The foot is uniquely adapted for bipedal motion and as such is essentially a tripod. The tripod is basically formed by the first ray, the fifth ray, and the calcaneus and is supported by the osseous configuration of bones in the midfoot that form a Roman arch, which in and of itself is inherently stable.
These bones are supported by ligamentous structures as well as tendons that help preserve the arch and support foot function. For this reason, resections of the first and fifth rays typically result in significant alterations in function, especially the first ray. The resulting forces after resection of the first ray result in transfer to the lesser metatarsals, which are ill adapted to structurally support the weight of the body, resulting in transfer metatarsalgia.
These structural alterations can be mitigated in part by the judicious use of orthotics, such as a medial heel wedge to transfer the forces farther lateral or the use of a metatarsal bar, which will more evenly distribute the weight across the lesser metatarsals. Resection of the fifth ray is relatively easily compensated for by creating an orthosis that transfers the forces medially; thus, a lateral heel wedge is beneficial.
Resection of the middle rays results in insignificant loss of function and acceptable cosmesis. The only net result is narrowing of the forefoot, which can be easily compensated for with shoe modifications.
The Lisfranc joint is the tarsometatarsal joint. An amputation at this level will preserve the dorsiflexors and plantarflexors. These amputation levels are highly functional with minor shoe-wear modifications and forefoot fillers. If the metatarsal bases can be preserved using a transmetatarsal amputation, the functional outcome is improved.
The Chopart joint is also known as the transverse tarsal joint. It includes the talonavicular and calcaneocuboid joints. An amputation at this level preserves the plantarflexors but sacrifices the dorsiflexors, often resulting in an equinus contracture due to unopposed action of the Achilles tendon.
To circumvent this problem, the tibialis anterior is used. It is detached from the tarsal navicular with a cuff of soft tissue, preferably periosteum. A drill hole is made through the neck and head of the talus in an oblique fashion from dorsolateral to plantar medial. The tendon is then routed through this bone tunnel and sewn to itself or soft tissue as it exits through the tunnel. This repair may be augmented with bone anchors placed near the dorsal opening of the tunnel. The residual foot is maintained in maximal dorsiflexion (FIG 2).
The advantage of a Chopart amputation over a Syme amputation is the maintenance of hindfoot height. This is an end-bearing residual limb and the patient can negotiate short distances without modified shoe wear or prosthetic fitting.
INDICATIONS
Ray Resections
The indications for ray resections are tumors involving the toe or metatarsal bone. Benign tumors make up the majority of these lesions.12
Lisfranc
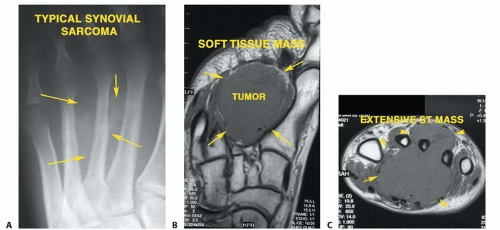
Extensive tumor involving the first and second interspaces in adjacent metatarsals or multiple metatarsals (FIG 3)
Chopart
Tumors extending to the tarsometatarsal joint with soft tissue extension. FIG 4 shows the pathology specimen after wide resection of a chondrosarcoma involving multiple small bones of the foot.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with tumors of the metatarsals complain of pain with an associated mass. The mass may be small and chronic. It may be first noticed after a minor injury. The patient may have difficulty with weight-bearing activities, including walking and standing. Shoe wear, particularly fashionable shoes, may be limited.
Physical examination (Table 1) often shows a tender mass localized to the toe, metatarsal, or midfoot. There may be associated swelling. If a sensory nerve overlies the mass, there may be paresthesias. If the mass is large, there may be loss of motion or discomfort with active range of motion of the foot and ankle.
IMAGING AND OTHER STAGING STUDIES
Preoperative studies include standing plain radiographs of the foot, including anteroposterior, lateral, and oblique views. If there is involvement of the ankle joint, anteroposterior and mortise views of the ipsilateral ankle are obtained as well.
SURGICAL MANAGEMENT
The goal of the surgical procedure is to remove the tumor with adequate margins.
FIG 6 illustrates a case of osteosarcoma of the calcaneus. Osteosarcoma is usually treated with wide resection, but in this case, the tumor was confined to the calcaneus. The patient had a good response to adjuvant chemotherapy, with 100% tumor necrosis and was treated with the only calcaneal prosthesis reported in the world.
A long plantar flap is important for a sturdy end-bearing stump.
The quality of the tissue is more important than the quantity.1
The bony edges should be smooth and beveled if possible.
Myodesis is helpful to pad the end of the stump.
Reconstruction of the anterior tibialis tendon insertion into the neck of the talus in the Chopart amputation will help prevent an equinus contracture.
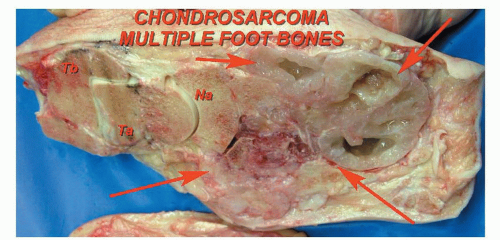 FIG 4 • Chondrosarcoma can spread to involve multiple sites. This photograph shows the pathology specimen after a below-knee amputation of a chondrosarcoma involving multiple small bones of the foot. |
Preoperative Planning
Preoperative planning is crucial for a good outcome. The preoperative radiographs, computed tomography (CT), and MRI studies are important to determine the amount of tumor involvement (FIG 7). They also show the extent of soft tissue tumors and may be helpful in distinguishing benign from malignant tumors.19 The results of the biopsy will determine the level of amputation.
The level of amputation is an important part of preoperative planning. The length of the residual stump is as important as the quality of soft tissue. There must be adequate padding of skin, subcutaneous fat, muscle, and tendons to cover the end of the bones.
Table 1 Physical Examination Methods | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
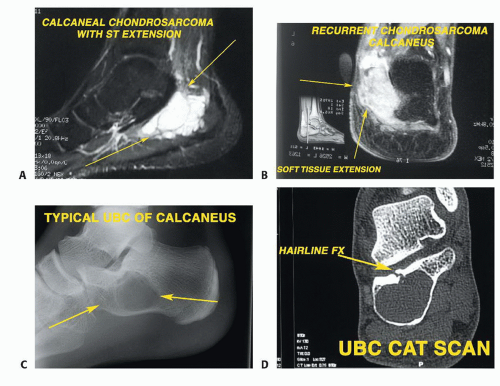 FIG 5 • Chondrosarcoma of the calcaneus. A,B. MRI shows extension into the soft tissue. It was treated with cryosurgery but recurred and a below-knee amputation was performed. C,D. Unicameral bone cyst (UBC) of the calcaneus. The radiograph shows the typical expansile appearance of the UBC. The CT scan shows greater bony detail. The lesion was treated with curettage, graft, and PMMA.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|