Fibroepithelial lesions
Some lesions of the breast present as discrete masses composed of both stromal and epithelial components. Included within this category of biphasic lesions are fibroadenomas and phyllodes tumors. In addition, several other breast lesions present as well-defined nodules that possess histologic features that may resemble fibroadenomas, including several lesions categorized as “adenomas” and mammary hamartomas.
FIBROADENOMA
Fibroadenomas are the most common benign tumors of the female breast. They are most frequent in young women, especially those under 30 years, but may be seen at any age. They generally present as a solitary, palpable, firm, mobile mass and are typically <3 cm in size. Less frequently, multiple synchronous or metachronous lesions occur, which may be unilateral or bilateral. In addition, nonpalpable fibroadenomas may be detected by mammography as a mass, microcalcifications, or both.
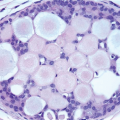
Fibroadenomas are easily shelled out surgically and, on gross examination, appear as firm, well-circumscribed, ovoid nodules that have a smooth, bosselated outer surface and a tan-gray, bulging, lobulated cut surface, often with visible slit-like spaces (Fig. 6.1). However, the gross appearance may vary from soft and mucoid to extremely fibrotic and calcified.
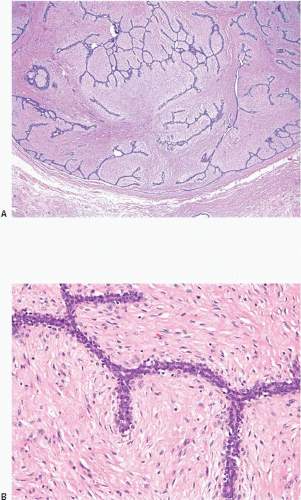
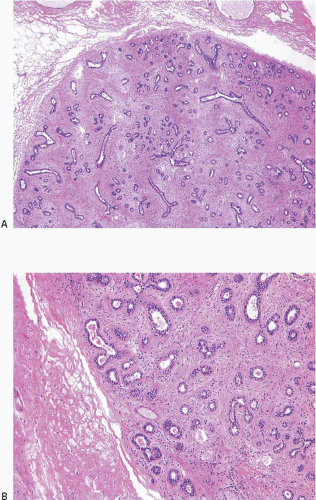
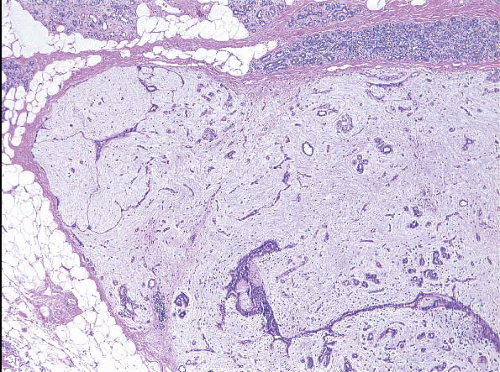
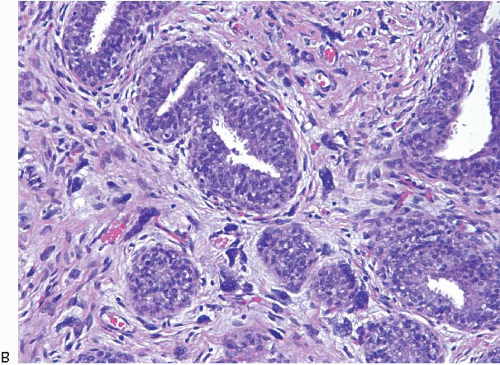
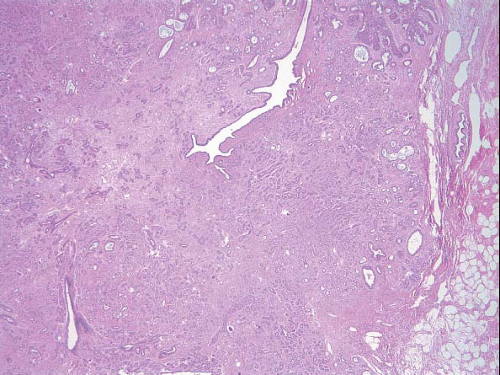
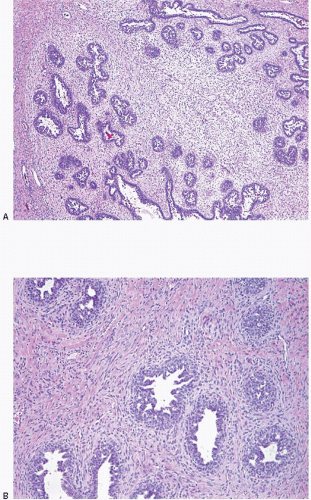
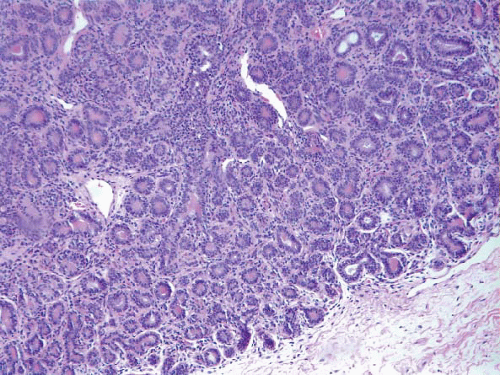
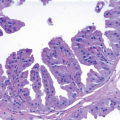
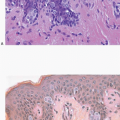
Microscopically, fibroadenomas are well-circumscribed, but unencapsulated lesions characterized by a proliferation of both stromal and glandular elements. In most fibroadenomas, the proportion of glands and stroma is relatively consistent throughout the lesion. Two growth patterns are recognized: an intracanalicular pattern, in which the glands are distorted, stretched, and compressed by the proliferating stroma (Fig. 6.2, e-Fig. 6.1), and a pericanalicular pattern, in which the stroma surrounds glandular structures with open lumina (Fig. 6.3, e-Fig. 6.2). These patterns often coexist and are not thought to have any clinical significance. However, a fibroadenoma with a prominent intracanalicular pattern could
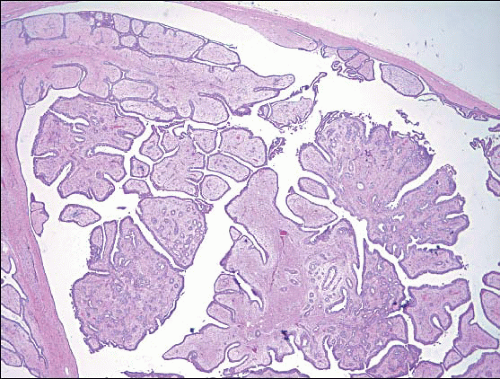
be misconstrued as a benign phyllodes tumor or an intraductal papilloma, particularly in the small samples provided by core-needle biopsy (Fig. 6.4).
be misconstrued as a benign phyllodes tumor or an intraductal papilloma, particularly in the small samples provided by core-needle biopsy (Fig. 6.4).
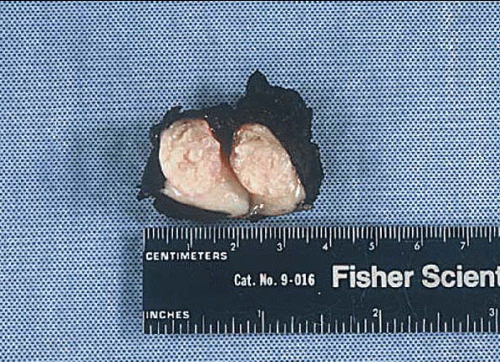 FIGURE 6.1 Fibroadenoma, bisected. The tumor is well-circumscribed and bulges above the cut surface of the specimen. Slit-like spaces are apparent. |
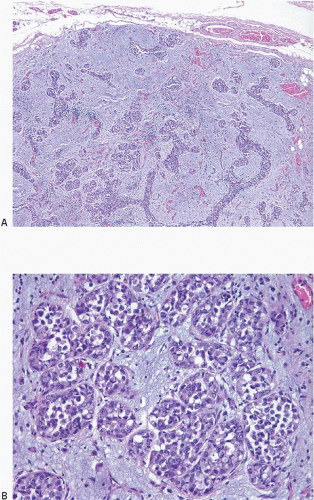
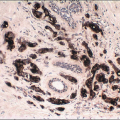
The glands in fibroadenomas, as in other benign lesions, have an inner epithelial and outer myoepithelial cell layer. The epithelium may consist of a single layer of cuboidal to columnar cells or may exhibit a variety of alterations. These include metaplastic changes (most often apocrine, less frequently squamous), cystic changes, and sclerosing adenosis. Epithelial proliferative changes may occur, including usual ductal hyperplasia, atypical ductal hyperplasia, atypical lobular hyperplasia, and lobular and ductal carcinoma in situ.1,2 In situ carcinomas are confined to the fibroadenoma in the majority of cases (Fig. 6.5, e-Fig. 6.3). Invasive carcinoma may also involve a fibroadenoma. Although this may be confined to the fibroadenoma, more commonly, it is the result of extension of a carcinoma in the adjacent tissue into the fibroadenoma.
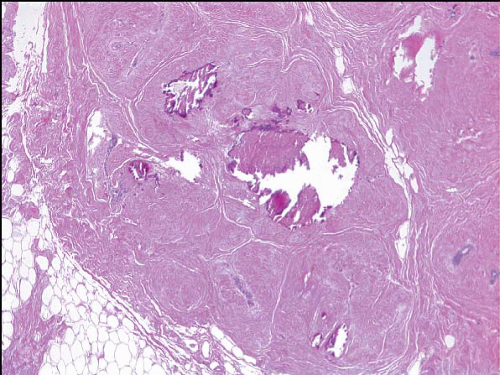
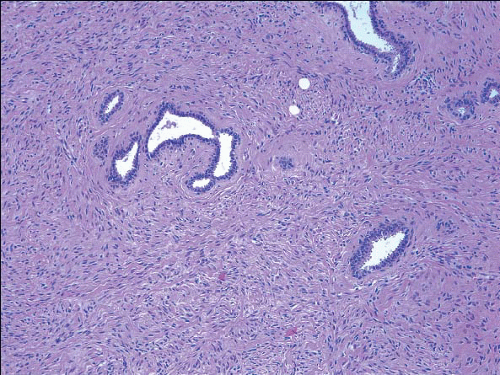
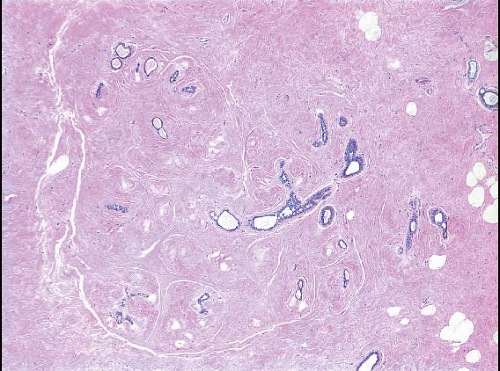
The stromal component varies in both appearance and the degree of cellularity but tends to be relatively uniform within a given lesion. Most commonly, the stroma is composed of an admixture of collagen and spindle-shaped stromal cells with bland ovoid to elongated nuclei. Stromal cell mitoses, while uncommon, may be seen, particularly in lesions in adolescents and young women. Some fibroadenomas show prominent stromal myxoid change (Fig. 6.6, e-Fig. 6.4). Myxoid fibroadenomas (as well as myxomas) have been reported in patients with Carney syndrome,3 but most patients who have fibroadenomas with prominent myxoid change do not have this syndrome. In other cases, particularly in older women, the stroma may be hyalinized and show calcifications (Fig. 6.7, e-Fig. 6.5). Focal or diffuse stromal hypercellularity may be seen and when prominent warrants a diagnosis of “cellular fibroadenoma” (Fig. 6.8, e-Fig. 6.6). However, there are no agreed upon guidelines regarding how cellular the stroma must be in order to warrant categorization as hypercellular. As will be discussed later, lesions of this type must be distinguished from phyllodes tumors. An uncommon feature within the stroma of fibroadenomas is the presence of multinucleated giant cells (Fig. 6.9).4, 5 and 6 These can produce a striking low-power picture, but the cytologic features, although bizarre, are benign and mitotic figures are not seen. These cells are identical to the multinucleated giant cells that are occasionally seen in otherwise normal breast stroma (see also Fig. 1.12). The stroma of fibroadenomas may contain adipose tissue or areas of pseudoangiomatous stromal hyperplasia. Heterologous stromal elements such as smooth muscle, cartilage, and bone may also be seen, albeit rarely.
Fibroadenomas may undergo infarction; this occurs most frequently during pregnancy and lactation.
Estrogen receptor (ER)β, but not ERα, is expressed in the stromal cells of fibroadenomas,7 whereas the epithelium often shows variable expression of ERα. The level of expression of stromal ERβ correlates with young age and stromal cellularity.7 Progesterone receptor can be expressed in both the epithelium and stroma.
Fibroadenomas are benign lesions. Although they have traditionally been treated with local excision, management by observation only is a reasonable option when identified in core-needle biopsy specimens. Clinical follow-up studies have indicated that women with fibroadenomas have a slightly increased risk of subsequent breast cancer, which is comparable to that seen in association with other proliferative lesions without atypia (relative risk ∽1.5 to 2.0).8 The risk is higher among women with complex fibroadenomas (see the subsequent text). Of note, the presence of atypical hyperplasia in a fibroadenoma does not appear to be associated with the same increased level of cancer risk as atypical hyperplasia in otherwise normal breast tissue.9
The key features of fibroadenomas are summarized in Table 6.1.
TABLE 6.1 Key Features of Fibroadenoma | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
FIBROADENOMA VARIANTS
Complex Fibroadenoma
Fibroadenomas that contain cysts larger than 3 mm, sclerosing adenosis, epithelial calcifications, or papillary apocrine change have been called “complex fibroadenomas” (Fig. 6.10, e-Fig. 6.7).8 In one clinical followup study, complex fibroadenomas were reported to be associated with a greater subsequent breast cancer risk than fibroadenomas that lack such changes (relative risk ∽3.0).8
Juvenile Fibroadenoma
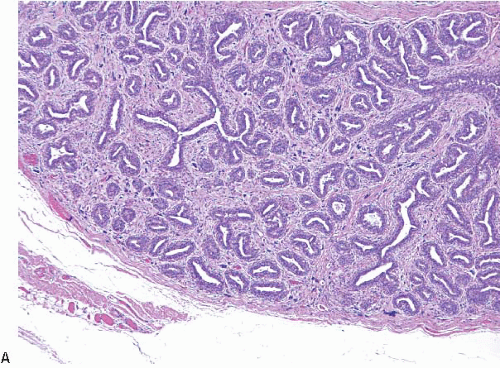
Most fibroadenomas in young girls and adolescents have the appearance of typical fibroadenomas as described previously. The term juvenile fibroadenoma has been used to describe fibroadenomas that occur predominantly in adolescents and are characterized by more stromal cellularity and a greater degree of epithelial hyperplasia than seen in fibroadenomas of the usual type (Fig. 6.11, e-Fig. 6.8). Juvenile fibroadenomas may grow rapidly and may become extremely large and even produce marked distortion of the breast.10 Some authors have used the term giant fibroadenoma to describe such large, juvenile fibroadenomas. However, others have used “giant fibroadenoma” to describe typical fibroadenomas that become very large.
Fibroadenomatous Change (Fibroadenomatoid Hyperplasia)
Fibroadenomatous change or fibroadenomatoid hyperplasia is a term used to describe histologic changes in the breast similar to those seen in fibroadenomas, but in which no discrete mass is formed (Fig. 6.12).
ADENOMAS
A variety of lesions of the breast have been considered to represent “adenomas.” Some (such as tubular adenomas) may be variants of fibroadenoma, whereas others are unrelated to fibroadenomas or to each other.
Tubular Adenoma
Tubular adenomas are well-demarcated lesions that have features in common with fibroadenomas.11 These relatively rare lesions usually occur in young women. It is debatable whether tubular adenoma should be considered a separate entity or merely a variant of fibroadenoma in which the epithelial elements predominate. On gross examination, like fibroadenomas, they are well-defined, but are softer and are characteristically tan-brown. The hallmark of tubular adenomas is the presence of closely packed round to oval glands or tubules, with little intervening fibrous stroma (Fig. 6.13). The tubules are lined by a double cell layer, but the myoepithelial cells are often inconspicuous. A stromal lymphocytic infiltrate may be present.
Lactating Adenoma (Nodular Lactational Hyperplasia)
This lesion consists of a relatively circumscribed breast mass that occurs only in pregnancy and the postpartum period. Although some lesions with these features may represent fibroadenomas in which the glands show superimposed secretory features (Fig. 6.14




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree