Gene
Chromosomal location
Function
Mode of inheritance
Lifetime risk of developing breast cancer
Other major cancer risk
Clinical syndrome association
TP53
17p13.1
Regulates expression of many genes by anti-proliferative mechanisms inducing cell cycle arrest and apoptosis
Autosomal dominant
85–90 %
Soft tissue (sarcomas), bone (osteosarcoma), CNS tumors (choroid plexus tumors), adrenal glanda
Li-Fraumeni syndrome, Li-Fraumeni-like syndrome
ATM
11q22-q23
Upstream regulator of proteins involved in double-stranded DNA repair, including BRCA1, TP53, and CHEK2
Autosomal dominant and recessive
~20 % or less
Lymphoproliferative disorders
Ataxia-telangiectasia
CHEK2
22q12.1
Encodes for a threonine/serine kinase that prevents cell proliferation by phosphorylation of proteins involved in checkpoint control
Autosomal dominant and recessive
~20 % or less
Colorectal, prostate
–
BRIP1
17q22.2
Encodes for a DNA helicase that performs BRCA1-dependent DNA repair and checkpoint control
Autosomal dominant and recessive
~20 % or less
Ovary, cervix
Fanconi anemia
PALB2
16p12.2
Acts as a functional bridging molecule linking the DNA repair functions of BRCA1 and BRCA2
Autosomal dominant and recessive
~20 % or less
Pancreas
Fanconi anemia
CDH1
16q22.1
Encodes for a cell adhesion molecule called E-cadherin
Autosomal dominant
50–60 %
Stomach
Hereditary diffuse gastric cancer syndrome
PTEN
10q23.3
Down-regulates the phosphatidylinositol-3-kinase (PI3K) signal transduction cascade and acts as a tumor suppressor and growth regulator
Autosomal dominant
25–50 %
Thyroid (except medullary carcinoma), endometrium, colon, rectum
Cowden syndrome
STK11
19p13.3
Encodes for serine threonine kinase
Autosomal dominant
~30 %
Colorectal, gastric, pancreatic, ovary
Peutz-Jeghers syndrome
RAD50
5q31
Part of MRN complex along with MRE11 and NBS1, which facilitates double-strand DNA break repair
Unknown
Unknown
Unknown
Ataxia-telangiectasia-like disorder, Nijmegen breakage syndrome (NBS) and NBS-like disorder
Table 2.2
Clinical syndromes associated with breast cancer
Gene(s) involved | Clinical manifestations | Cancer prevention strategy | Cancer management | |
|---|---|---|---|---|
Hereditary breast and ovarian cancer syndromea | BRCA1, BRCA2 | Early onset of breast and ovarian cancer. Also high risk for early onset prostate, pancreas, skin (melanoma), gastrointestinal tract cancers | • Genetic counseling and standard genetic testing with full gene sequencing and large genomic alterations analysis • Patient awareness and routine monthly self breast exam from 18 years of age onwards • Biannual clinical breast exam from 25 years of age onward • Annual bilateral mammogram and MRI starting at age 25 • Discuss ovarian cancer screening (transvaginal ultrasound and serum CA125 testing every 6 months) • Discuss risks and benefits of chemoprevention • Risk-reducing mastectomies and salpingoophorectomies • Prostate cancer screening in men after age 40 | • Individualized chemotherapeutic regimen with poly(ADP-ribose) polymerase inhibitors ± platinum or other combination therapy • Bilateral mastectomies and salpingoophorectomy |
Li-Fraumeni and Li-Fraumeni-like syndromea | TP53 | Autosomal dominant cancer predisposition syndrome associated with early onset of breast cancer, choroid plexus carcinomas, adrenocortical carcinoma, soft tissue sarcoma and osteosarcomas. Also high risk for many other visceral malignancies and lymphoproliferative disorders | • Genetic counseling and testing • Patient awareness and routine monthly self breast exam from 18 years of age onwards • Biannual clinical breast exam from 25 years of age (or as early as 18 years) onward • Annual bilateral mammogram and MRI from 25 years of age (or as early as 18 years) onward • Colonoscopy every 2–5 years starting 25 years of age onward • Annual skin and neurologic exam | • Surgical management preferred ± individualized chemotherapeutic regimen • Radiation therapy often used as last option as there is a questionable risk for therapy induced secondary malignancy |
Cowden syndromea | PTEN | Autosomal dominant cancer predisposition syndrome with early onset of breast, thyroid, endometrium, and colorectal cancers. Also characterized by multiple hamartomas, facial trichilemmomas, acral keratoses and oral papillomatous papules | • Genetic counseling and testing • Patient awareness and monthly breast exams • Discuss annual mammography ± MRI • Discuss increased surveillance for endometrial, thyroid, and colorectal cancers, although there is no consensus screen strategy • Discuss prophylactic mastectomies and hysterectomy | • Individualized treatment strategy |
Peutz-Jeghers syndrome | STK11 | Rare autosomal dominant condition characterized by hamartomatous polyps in the GI tract, mucocutaneous pigmentation and increased risk for breast, colorectal, gastric, pancreatic, and ovarian cancer | • Patient awareness, genetic counseling and testing • No established guidelines on cancer prevention, patients may be followed on an individualized basis | • Individualized treatment strategy |
Ataxia-telangiectasia (AT), AT-like disorder, Nijmegen breakage syndrome (NBS) and NBS-like disorder | ATM, RAD50, NBS1, MRE11 and MRN complex | AT is an autosomal recessive disorder characterized by progressive neurologic impairment, cerebellar ataxia, ocular telangiectasia, variable immunodeficiency, defective organogenesis and an increased risk of developing visceral malignancies and lymphoproliferative disorders | • Patient awareness, genetic counseling, and testing • No established guidelines on cancer prevention, patients may be followed on an individualized basis | • Individualized treatment strategy |
Fanconi anemia | BRIP1, PALB2, BRCA2 and other FANC group of genes | X-linked recessive disorder characterized by bone marrow failure, developmental abnormalities, and increased risk for ovarian, prostate, pancreas, skin gastrointestinal tract, and cervix cancers. Clinical features include skin pigmentation, short stature, upper limb, and eye malformations | • Patient awareness, genetic counseling and testing • No established guidelines on cancer prevention, patients may be followed on an individualized basis | • Individualized treatment strategy • Cells with mutated FANC genes show profound sensitivity to DNA interstrand cross-linking agents (cisplatin and mitomycin C) • Radiation and PARP inhibitors may play a role |
Hereditary diffuse gastric cancer syndrome | CDH1 | Autosomal dominant cancer predisposition syndrome with increased risk for developing breast and gastric cancers | • Patient awareness, genetic counseling, and testing • No established guidelines on cancer prevention, patients may be followed on an individualized basis | • Individualized` treatment strategy |
Genetics of Breast Cancer
High-Penetrance Genes
Breast Cancer 1, Early Onset (BRCA1)
BRCA1 is a large gene located on the long (q) arm of chromosome 17 at position 21 (17q21). BRCA1 is a tumor suppressor gene, which is expressed in response to genomic instability and is influenced by estrogen. Its main function is related to DNA repair including homologous recombination, nucleotide excision repair, and spindle regulation. It also acts as a gatekeeper of cell-cycle progression mainly through checkpoint control [5]. Recent studies have described complex and innovative mechanisms for the localization of BRCA1 to DNA-breaks, including an emerging ubiquitylation-dependent cascade and an association with BRCA2 and genes in the Fanconi anemia pathway [6]. Thus, BRCA1 acts as a regulator of genome stability and its main function is to respond to various types of DNA damage via a complex interaction with BRCA2 and other genes.
Numerous mutations in BRCA1 have been described. The majority of which are point mutations and small insertions/deletions leading to truncated forms of the BRCA1 protein [7]. Large genomic deletions including whole exon deletions have also been detected using more sophisticated methods such as multiplex ligation-dependent probe amplification (MLPA) [8]. Some mutations appear to be more common in certain ethnic groups (founder mutations). The most commonly described is the c.5266dupC mutation (also known as 5382insC or 185delAG), which is seen in up to 2 % of the Ashkenazi Jewish population. However, recent studies have suggested that this mutation may be prevalent in some other ethnic groups where genetic screening of BRCA1 is not routinely performed [9].
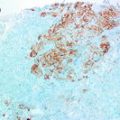
Approximately 1 in 1000 individuals in the female population carries a pathogenic mutation in BRCA1. BRCA1 cancers account for approximately 10 % of all familial cancers; [10–12] and a mutation in BRCA1 confers a 70–85 % lifetime risk of developing breast cancer [11–13]. BRCA1 mutations also are associated with a 50 % increased risk of developing ovarian cancer, especially high-grade serous carcinoma [14]. The risk for developing both breast and ovarian cancer in BRCA1 patients is age dependant, and the age at which these cancers present is much younger than that of the general population [11, 14]. Tumors developing in patients with BRCA1 mutations are usually triple-negative (negative for ER, PR, and HER2), high-grade invasive ductal carcinomas. However, approximately 5–25 % of BRCA1 breast carcinomas can be ER positive and a small percentage can show low-grade nuclear histology. Gene expression profiling studies show that BRCA1 associated breast carcinomas tend to cluster with sporadic triple-negative cancers [15–18]. BRCA1 breast cancers share many morphologic features with medullary-like carcinoma and basal-like carcinoma, with pushing margins, a prominent lymphocytic infiltrate, high-grade nuclear atypia and brisk mitosis (see Chap. 11) [15, 16]. Further, immunohistochemical expression of basal cytokeratins such Cytokeratin (CK) 5/6, CK14, CK17 and epidermal growth factor receptor (EGFR) which define BLBC are also identified in many BRCA1 related tumors [19]. BRCA1 carcinomas also tend to show high expression of cell proliferation marker Ki-67 as well as p53 and p16 positivity as compared to sporadic cancers [20].
Breast Cancer 2, Early Onset (BRCA2)
BRCA2 is a large gene located on the long (q) arm of chromosome 13 at position 12.3 (13q12.3). BRCA2 belongs to a family of genes involved in the Fanconi anemia pathway; which also includes partner and localizer of BRCA2 (PALB2) and BRCA1 interacting protein C-terminal helicase 1 (BRIP1) which are discussed later in the chapter.
As in BRCA1, BRCA2 is also involved in DNA repair. Its role however is not as well understood as that of BRCA1. It is now thought that BRCA2 facilitates homologous recombination and double-strand break repair through its interaction with RAD51. The BRCA2 protein forms a stable complex with the RAD51 protein and directs it to sites of DNA damage [21]. 21 BRCA2 also plays a role in the Fanconi anemia pathway of breast cancer through its interaction with other FANC (Fanconi anemia, complementation groups) genes such as BRIP1 and PALB2. A defect in any one of the proteins along the Fanconi anemia pathway prevents cancer cells from repairing interstrand crosslinks, predisposing them to chromosomal instability. It is suggested that BRCA2 protein helps to prevent these interstrand crosslinks by its ability to facilitate homologous recombination [22, 23].
Similar to BRCA1, hundreds of mutations have been described in BRCA2, the majority being point mutations leading to frameshifts and production of an abnormally truncated BRCA2 protein. Founder mutations in BRCA2 have been described in certain ethnic groups such as the c.5946delT (6174delT) mutation in the Ashkenazi Jewish population [3, 11].
Approximately 1 in 800 individuals in the female population carry a pathogenic mutation in BRCA2. Similar to BRCA1, BRCA2 cancers account for approximately 10 % of familial cancers; [10–12] and a mutation in BRCA2 confers a 50–85 % lifetime risk of developing breast cancer [11–13]. There is an approximate 30 % risk for BRCA2 patients to develop ovarian cancer [14]. Males who are carriers of germline mutations in BRCA2 have an increased risk of developing breast cancer, approximately 10 % greater than men in the general population [24]. BRCA2 also confers an increased risk for the development of other cancers. Compared to non-carriers, men with BRCA2 mutations have a three-fold risk of developing prostate cancer and; according to recent studies; these tumors are often of a higher grade (Gleason score >7) and have an increased risk of recurrence [25]. Germline BRCA2 gene mutations are also responsible for approximately 5–20 % of familial pancreatic cancers [26, 27]. Additionally, there is some evidence for an increased risk of gastrointestinal tract cancers, melanomas, bone tumors and even rarely pharyngeal carcinomas in BRCA2 families [28, 29]. BRCA2 associated breast cancers are generally heterogeneous and unlike BRCA1, there is no specific phenotype that has proven to be predictive of BRCA2 status. Clinical features of BRCA1 and BRCA 2 genes and their associated cancers are compared in Table 2.3.
Table 2.3
Comparison of BRCA1 and BRCA2
Gene | BRCA1 | BRCA2 |
|---|---|---|
Chromosomal location | 17q21 | 13q12.3 |
Function | DNA repair including homologous recombination, nucleotide excision repair, and spindle regulation | Homologous recombination and double-strand break repair through its interaction with RAD51 |
Mode of inheritance | Autosomal dominant | Autosomal dominant |
Lifetime risk of developing breast cancer | 70–85 % | 50–85 % |
Other major cancer risk | Ovary | Ovary, male breast, prostate, pancreas, skin (melanoma), gastrointestinal tract |
Clinical syndrome association | Hereditary breast and ovarian cancer syndrome | Hereditary breast and ovarian cancer syndrome, Fanconi anemia |
Typical phenotype | High-grade ductal carcinomas, often with ‘basal phenotype’ (medullary appearance, pushing edges, lymphocytic infiltrate, high nuclear grade, and brisk mitotic activity). Tumors are often triple negative | No specific phenotype, ductal carcinoma NOS |
Cancer management | Individualized chemotherapeutic regimen with poly (ADP-ribose) polymerase (PARP) inhibitors ± platinum-based therapy. Bilateral mastectomies and salpingoophorectomy | Individualized chemotherapeutic regimen with poly (ADP-ribose) polymerase (PARP) inhibitors ± platinum-based therapy. Bilateral mastectomies and salpingoophorectomy |
Tumor Protein P53 (TP53)
TP53 is a tumor suppressor gene located on the short (p) arm of chromosome 17 at position 13.1 (17p13.1). It is the most commonly altered gene in human cancer; being mutated in more than 50 % of all cancers.
TP53 encodes a transcription factor which responds to numerous cellular mechanisms to regulate expression of target genes, and does so primarily by anti-proliferative mechanisms inducing cell cycle arrest and apoptosis.
Thousands of mutations in TP53 have been described in a variety of human cancers. The majority of which are missense substitutions; and other alterations include frameshift insertions and deletions, nonsense mutations, and silent mutations [30]. An exhaustive and comprehensive list of over 25,000 germline, somatic and experimentally induced mutations in TP53 along with information on the functional impact of mutant p53 proteins is available online at the International Agency for Research on Cancer (IARC) TP53 Database [31].
Rare germline mutations in TP53 cause Li-Fraumeni and Li-Fraumeni-like syndrome, which are autosomal dominant genetic disorders characterized by an increased likelihood of developing a number of different malignancies. Somatic mutations in tumors are very common and occur in more than 50 % of all human cancers. In patients with a TP53 mutation, the lifetime risk for developing any cancer is almost 100 %. This risk is age dependant, with approximately 35–50 % developing by age 30, and 80–90 % by age 60 [32]. The majority of cancers seen in affected families are breast cancer (most common), soft tissue sarcomas, osteosarcomas, central nervous system tumors (especially choroid plexus tumors) and adrenocortical carcinomas. Other cancers seen in patients with TP53 mutations are gastrointestinal malignancies (esophageal, gastric, and colorectal), genitourinary malignancies (bladder, renal, Wilms tumor, endometrial, ovarian, germ cell tumors, prostate), melanoma, thyroid cancers, and lymphoproliferative disorders. Due to its general low prevalence, TP53 mutations account for less than 1 % of familial breast cancers [10]. There is no specific phenotype seen in TP53 mutated breast cancers.
Moderate Penetrance Genes
Ataxia Telangiectasia Mutated Gene (ATM)
The ATM gene is located on the long (q) arm of chromosome 1, between positions 22 and 23 (11q22-q23). A large number of mutations involving the ATM gene have been identified, which are responsible for approximately 2 % of familial breast cancers [33].
The ATM protein acts as an important upstream regulator of proteins involved in double-stranded DNA repair, including BRCA1, TP53, and CHEK2. ATM mediates checkpoint regulation and homologous repair by phosphorylation of these proteins. Most mutations in this gene lead to truncated forms of the ATM protein which increases the susceptibility for developing genomic instability, especially during exposure to ionizing radiation [34]. Mutations in ATM lead to ataxia-telangiectasia, an autosomal recessive disorder characterized by progressive neurologic impairment, cerebellar ataxia, ocular telangiectasia, variable immunodeficiency, defective organogenesis and an increased risk of developing visceral malignancies, and lymphoproliferative disorders. A link between ATM mutations and breast cancer has been suspected for many years. Recent studies of patients with ataxia-telangiectasia have suggested that female relatives have a two to five fold increase in risk of developing breast cancer [35–37]. There are no known histologic phenotypes of breast cancer that predict an ATM mutation, and the clinical usefulness of testing for ATM mutations in breast cancer patients is uncertain at this time.
CHEK2 (Checkpoint Kinase 2 Gene)
The CHEK2 gene is located on the long (q) arm of chromosome 22 at position 12.1 (22q12.1). CHEK2 is a tumor suppressor gene, and mutations in this gene have been identified in a number of human malignancies including breast, prostate, and colon cancers [38].
CHEK2 encodes a threonine/serine kinase involved in the same pathways as TP53 and BRCA1. In response to DNA damage, this protein prevents cell proliferation by phosphorylation of proteins involved in checkpoint control, thus blocking cellular entry into mitosis [39]. Mutations in CHEK2 were originally investigated as a cause of Li-Fraumeni like syndrome [40], however, many subsequent studies have shown that CHEK2 mutations are directly associated with the development of breast cancer. Although numerous mutations in CHEK2 have been described, perhaps the most important is a founder mutation, 1100delC, discovered in people of North European descent. The 1100delC mutation is present in ~1 % of European families and in up to 5 % of breast cancer families of North European descent. Individuals heterozygous for this mutation have a two to three fold increased risk of developing breast cancer [41, 42]. In women with estrogen receptor–positive breast cancer, 1100delC heterozygosity is also associated with a three to four fold risk of developing a second breast cancer [43]. Many more CHEK2 mutations have been described, but their clinical significance are still unknown.
BRCA1 Interacting Protein C-Terminal Helicase 1 (BRIP1)
The BRIP1 gene is located on the long (q) arm of chromosome 17 at position 22.2 (17q22.2). BRIP1 belongs to the Fanconi anemia pathway of genes, which also includes PALB2 (discussed ahead) and BRCA2.
BRIP1 encodes for a DNA helicase that interacts with BRCA1 and has BRCA1-dependent DNA repair and checkpoint functions. Biallelic mutations in BRIP1 result in the chromosome instability disorder Fanconi anemia, while heterozygous inactivating mutations have been reported to confer an increased susceptibility to breast cancer in monoallelic carriers [44, 45]. These account for less than 0.5 % of all breast cancers. Patients with BRIP1 mutations have approximately a 20 % lifetime risk of developing breast cancer. Frameshift mutations in BRIP1 have been described which may be associated with an increased risk of developing ovarian cancers in some European populations [46]. Most recently, BRIP1 has been implicated in the genetic susceptibility for developing cervical cancer [47].
Partner and Localizer of BRCA2 Gene (PALB2)
The PALB2 gene is located on the short (p) arm of chromosome 16 at position 12.2 (16p12.2). As discussed above, PALB2 belongs to the FANC group of genes in the Fanconi anemia pathway of breast cancer.
PALB2 encodes for a protein that is involved in double-stranded DNA break repair. Studies have suggested that PALB2 acts as a functional bridging molecule linking the DNA repair functions of BRCA1 and BRCA2; as well as stimulating the recombinant functions of RAD51, and hence is critical in the maintenance of genomic stability [48–50]. PALB2 mutations account for a minority of breast cancer (less than 0.5 %). Similar to BRIP1 mutations, PALB2 mutations confer an approximate 20 % overall lifetime risk of developing breast cancer. Recently, PALB2 germline truncating mutations have also been implicated in the development of pancreatic cancer [51].
Other Genetic Mutations Conferring an Increased Risk of Developing Breast Cancer
Germline mutations of CDH1 [cadherin 1, type 1, E-cadherin (epithelial) located at 16q22.1] are associated with Hereditary Diffuse Gastric Cancer, which is an autosomal dominant cancer predisposition syndrome. CDH1 encodes for a cell adhesion molecule called E-cadherin. Patients with germline CDH1 mutations have a very high risk of developing gastric cancer but are also at an increased risk of developing breast cancer including both ductal and lobular carcinomas [52, 53]. Lobular carcinomas that arise in CDH1 mutation carriers as well as sporadic cases show similar phenotypes; i.e., both are characterized by a loss of E-cadherin expression at the cell membrane which can be demonstrated by immunohistochemistry. CDH1 mutations account for a small fraction of familial breast cancers (<2 %); and female carriers have an approximate 50 % lifetime risk of developing breast cancer [54]. Studies have estimated the cumulative risk of developing gastric cancer by age 80 years to be ~65 % for men and ~80 % for women [55].
STK11 (serine/threonine kinase 11, located at 19p13.3) mutations lead to Peutz-Jeghers syndrome, a rare autosomal dominant condition associated with the development of hamartomatous polyps throughout the gastrointestinal tract and mucocutaneous pigmentation. These patients are at increased risk of developing gastrointestinal as well as breast cancers. Women who are STK11 mutation carriers have an approximate 30 % lifetime risk of developing breast cancer. These tumors are often bilateral and sometimes develop at an early age [56].
PTEN (phosphatase and tensin homolog), located at 10q23.3) mutations are associated with the development of the autosomal dominant Cowden syndrome, characterized by multiple hamartomas in different organs, increased risk of cancers, facial trichilemmomas, acral keratoses and oral papillomatous papules. PTEN functions by down-regulating the phosphatidylinositol-3-kinase (PI3K) signal transduction cascade and acts as a tumor suppressor and growth regulator [57]. Many types of mutations in the PTEN gene have been identified in patients with Cowden syndrome. Breast cancer is the most common cancer seen in Cowden syndrome and females who carry mutations in the PTEN gene have a 25–50 % lifetime risk of developing breast cancer [58]. Cowden syndrome is responsible for less than 1 % of familial breast cancers. Other cancers seen in patients with PTEN mutations include thyroid cancers (non-medullary), colon, rectal, and endometrial carcinomas.
RAD50 (RAD50 homolog gene, located at 5q31) is a gene that has been implicated in the development of breast cancer. RAD50 interacts with two other genes, MRE11 (meiotic recombination 11, located at 11q21) and NBS1 [Nijmegen breakage syndrome 1 (also called Nibrin), located at 8q21], to form the MRN complex which acts as the primary sensor of double-stranded DNA breaks. The MRN complex facilitates double-strand DNA break repair by activating ATM kinase (discussed above). Mutations of MRE11, NBS1, and RAD50 give rise to cancer predisposition syndromes: ataxia-telangiectasia-like disorder, Nijmegen breakage syndrome (NBS) and NBS-like disorder, respectively [59, 60]. A founder mutation in RAD50 (687delT) has been discovered in breast cancer families of Finnish descent, but as this mutation is rare and has not been discovered in non-familial populations, its actual role in breast cancer development is still under scrutiny [61].
The risk of breast cancer in Lynch Syndrome (Hereditary Non-Polyposis Colorectal Cancer Syndrome) is uncertain due to conflicting data, and currently the National Comprehensive Cancer Network (NCCN) has no guidelines on risk assessment or screening for breast cancer in patients with Lynch Syndrome [62].
In recent years, well-validated studies have implicated a number of SNPs in various genes (e.g.,: FGFR2, TOX3/TNRC9, MRPS30, MAP3K1, NOTCH2, RAD51L1 etc.) to be associated with a slightly increased or decreased risk of developing breast cancer [4, 63–70]. SNPs in these genes are considered to be of low penetrance in the development of familial breast cancer and their clinical significance is currently uncertain. These genes are however important in understanding the biology of breast cancer development and may play a key role in discovering potential therapeutic targets in the future.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree