Chapter 8
Falls and immobility
Part 1: Falls
Introduction
‘This patient was found on the floor, exact circumstances unclear’
Many older people present to the ED having been found on the floor in their place of residence. Some are unable to recollect the exact circumstances of the event and even those who are cognitively intact may be too tired, distressed or unwell to give a clear history when they first present.
Differentiating between a fall due to a slip or trip and a fall complicated by transient loss of consciousness can be challenging, but early differentiation between these phenomena is essential in directing further investigation and management.
Definition
A fall is an unexpected event that results in a person coming to rest on the ground or other lower surface (1).
Background
One in three people over the age of 65 will fall each year (2), rising to one in two people over the age of 80 (3); half of those who fall will fall again in the following year. Falls are the leading cause of accidental death in the United Kingdom and the United States for people aged over 65 (2).
Falls are a common presenting symptom to the ED with over 2.3 million non-fatal falls treated in United States EDs in 2010 (2) and over 90,000 hospital admissions per year in the United Kingdom (3). The number of hospital admissions relating to falls is rising, and it is estimated that in the next 10–20 years, falls and fall-related injuries will cost the US Healthcare system $54.9 billion (4) and the UK National Health Service will spend over £6 billion on hip fractures alone (3).
| Drug class | Mechanism of action |
| Benzodiazepines and hypnotics | Reduce reaction time Reduce proprioception Balance disturbance/ataxia |
| Antidepressants & antipsychotics TCAs SSRIs Antipsychotics | Sedation with psychomotor retardation Orthostatic hypotension |
| Anti-convulsants | Sedation Dizziness Balance disturbance/ataxia |
| Digoxin Type 1 antiarrythmics Diuretics | Proven association with falls but causal mechanism remains unclear |
| ACE inhibitors Nitrates Ca channel blockers and β-blockers | Systematic reviews have identified no formal association; however, they are likely to contribute to orthostatic hypotension Frequently feature in polypharmacy (i.e. heart failure) which increases falls risk |
| Levodopa | Orthostatic hypotension |
| Opioids | Sedation |
TCA, tricyclic antidepressant; SSRI, selective serotonin reuptake inhibitor; ACE, angiotensin-converting-enzyme.
History
When undertaking the initial assessment of the patient found on the floor think: Before, During and After.
Box 8.2 highlights a few questions that should help clarify important aspects of the event.
The exact details surrounding a fall can be difficult to establish. The questions above will help distinguish a fall from transient loss of consciousness; however, the acronym SPLATT (symptoms, previous falls, location, activity, time, and trauma) (6) can be helpful in obtaining a focused history from a patient who has fallen, which, combined with a targeted examination is a solid foundation for further assessment and management.
- Symptoms around time of fall
- Previous falls
- Location of fall and length of lie
- Activity at time of fall
- Timing of the fall
- Trauma (physical or psychological) resulting from the fall.
History should also encompass a systemic screen for symptoms of recent illness, and environmental considerations such as trip hazards or the use of restraints.
Examination
General
The first objective of examination is to establish whether there is significant injury or medical complication resulting from the fall and if there is any underlying acute illness responsible. See Chapter 11 for a more detailed discussion on initial assessment following trauma.
All patients should then receive a general physical examination with particular focus on the locomotor system and neurological assessment.
A gait assessment should also take place in the ED. This may take the form of the ‘get up and go test’, where the patient is asked to stand up from a chair, walk a short distance, turn around, return and sit down again (13).
Specific areas of focus on examination
See Figure 8.1.
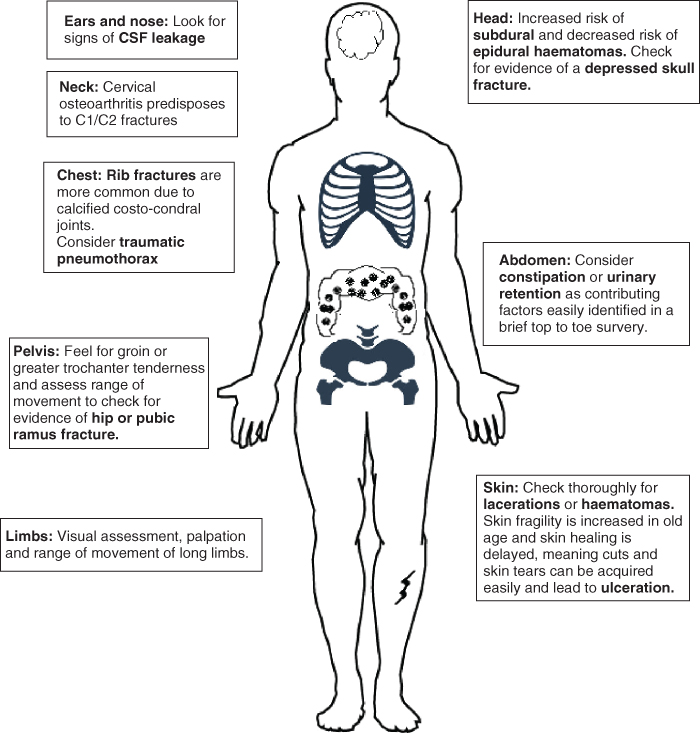
Figure 8.1 Head to toe assessment for minor trauma post fall: considerations when examining an older patient.
Investigations
Initial investigations
- Blood tests: Full blood count, urea and electrolytes, glucose
- ECG: 12 lead ECG
- Imaging: will be directed by the history and presentation but a low threshold for chest, hip and pelvic radiographs should be adopted, in addition to plain films of any area that is significantly bruised or tender.
Further investigations
Consider CT head and neck in patients with suspected head injury (see Chapter 14).
In patients with severe hip or groin pain and normal plain films, consider CT or MR hip to identify more subtle fractures; this is discussed further in Chapter 12.
There is a role for tilt table testing, 24 hour ECG and detailed vestibular assessment in older patients who have recurrent or unexplained falls; however, these are usually undertaken at a later stage (14).
Management
General
The management of patients who fall depends on the underlying cause and resulting complications. Acute illnesses such as pneumonia or urinary tract infection should be treated promptly and complications such as fractures or pneumothorax should be referred to the appropriate specialty.
For the management of falls resulting in major trauma, head injury, skin tears and fractures in older patients, see Chapters 11–14.
Patients presenting to the ED with recurrent falls who do not require hospital admission should be directed to their primary care provider or local falls multi-disciplinary clinic where they can be appropriately assessed. There is evidence that multi-disciplinary input from physiotherapy, occupational therapy, nursing and specialist medical staff reduces the incidence and prevalence of falls in community dwelling adults (17).
Specific management considerations in older patients
Soft tissue injury
Thirty to fifty percent of falls result in soft tissue injuries such as lacerations and bruising (15). Whilst many of these injuries are relatively minor and easily managed in the ED, in some cases, skin tears can be a major cause of morbidity requiring hospital admission, plastic surgery input and prolonged follow-up by specialist tissue viability (wound care) nurses. For more information on managing skin tears, see Chapter 13.
Fractures
Falls are the commonest cause of fractures in older people, Chapter 12 covers fracture management in further details.
Head injury
Many older people are on anticoagulants and this alters the management of traumatic head injury. For specific information on managing head injury in older patients, see Chapter 14.
Prolonged immobility
A ‘long lie’ can lead to multiple complications associated with prolonged immobility; these include rhabdomyolysis, dehydration, pneumonia and pressure ulcers. The management of these conditions is covered later in this chapter under the section Immobility.
Overview of an approach to a patient with a fall
If major injury and medical complications have been excluded, a decision should be made regarding the need for discharge or follow-up; this will often depend on a number of factors including mental state, ability to walk safely and social circumstances (Figure 8.2).
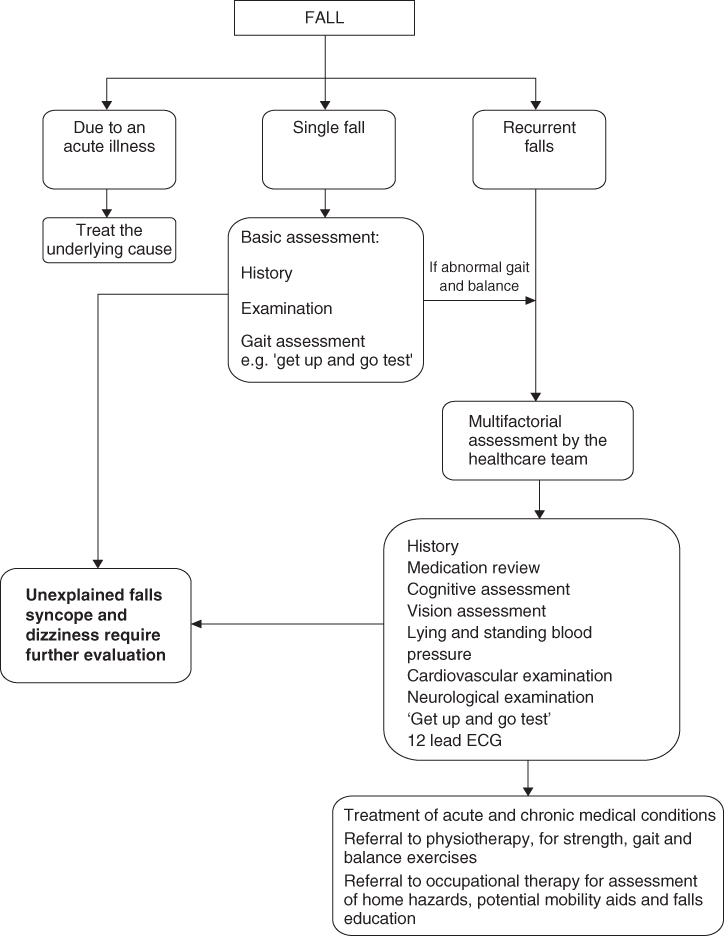
Figure 8.2 Overview of an approach to a patient with a fall.
Source: Adapted from ‘Falls’ in ABC of Geriatric Medicine, Cooper N et al, 2009, with permission from Wiley & Sons.
Part 2: Immobility
Introduction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








