Introduction
As discussed in prior chapters, osteosarcopenia is a geriatric syndrome resulting in falls and fractures as two of its common manifestations. Falls and fractures are consistently among the most frequent reasons for acute care use among older adults, and as a result have a major impact on individuals, families, and society. One out of five falls is injurious, resulting in fracture or head injury . Both fractures and head trauma in older adults are associated with increased disability, mortality, and decreased quality of life. In 2010, the medical cost of osteoporotic fractures in Europe was over €37 billion, and this cost is expected to increase by 25% in 2025 . By 2025, the annual medical cost of osteoporotic fractures in the United States is expected to be $25.3 billion .
In light of the high burden of falls and fractures, substantial efforts have been made to develop effective screening and prevention strategies. Clinical practice guidelines for treating osteoporosis and preventing falls in older adults have been written and widely disseminated. However, these efforts have largely considered osteoporosis and fall as separate geriatric syndromes in their own right, and have not considered how their overlapping pathogenesis and epidemiology should impact the screening and treatment for the other.
In this chapter, we describe the synergistic contributions of osteoporosis, obesity, and sarcopenia to the epidemiology of falls and fractures in older adults. We define important components of validated risk assessment tools for falls and fractures and point out opportunities to improve their predictive ability by incorporating markers of both muscle and bone quality. Finally, we highlight the potential of interventions targeting osteosarcopenia to have a pleiotropic impact on falls and fractures in older adults.
Overlapping epidemiology of sarcopenia, osteoporosis, falls, and fractures
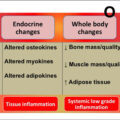
Available epidemiology suggests a synergistic and bi-directional relationship between sarcopenia and osteoporosis, falls, and fractures. The association between sarcopenia and subsequent falls has been consistently described, with a recent metaanalysis estimating an 89% higher odds in prospective studies (OR 1.89, 95% CI 1.33–2.68) . Similarly, there is an increased risk of falls among obese individuals in metaanalyses of prospective studies (OR 1.16, 95% CI 1.07–1.26) . Perhaps less well recognized, the odds of fracture are also greater in sarcopenic older adults (OR 1.84, 95% CI 1.30–2.62), even in studies adjusting for bone mineral density (BMD) . This temporal relationship goes both ways. Fractures, especially hip and vertebral, are associated with a subsequent loss in both bone mineral density (BMD) and muscle mass . While the loss of muscle mass and BMD has not been well studied following a fall, activity restriction and declines in physical performance after falls have been well described , and are likely related in part to the loss of muscle due to deconditioning.
Osteoporosis and falls have an especially important synergistic effect with each other. For example, in a study of more than 2600 women in Europe, women with osteoporosis but without a prior fall had an age- and BMI-adjusted fracture risk that was 2.8 times higher than women with neither. However, women with both osteoporosis and a history of falls had an adjusted fracture risk nearly 25 times higher . The risk of mortality in hip fracture patients is also higher in osteosarcopenic patients compared to those with osteoporosis or sarcopenia alone .
Risk assessment: An opportunity for prevention
The underlying common pathophysiology and synergistic, bi-directional relationship between osteoporosis, sarcopenia, falls, and fractures provides an opportunity for streamlined risk assessment and prevention for these conditions simultaneously in clinical care. Fall and fracture risk assessment in older adults should include a medication review and identification of chronic medical conditions that contribute to both osteoporosis and sarcopenia. Body composition measures offer a means of detecting osteosarcopenia, but clinical applications remain limited. Validated clinical tools are available, but have limitations that should be appreciated. Detection of osteosarcopenia is critical to decreasing falls and fractures and subsequently increasing patients’ quality of life and ability to age gracefully.
Medications associated with osteosarcopenia, falls, and fractures
Medications are an important target for both screening and prevention of falls and fractures in older adults. While there are several mechanisms by which medications increase the risk of falls and fractures (e.g., sedation, orthostatic hypotension), we will focus on those that directly impact the musculoskeletal system and thus contribute to osteosarcopenia. A summary of these medication classes and how they impact muscle and bone is found in Table 1 .
| Medication/co-morbidity | Proposed mechanism for osteosarcopenia |
|---|---|
| Medications | |
| Glucocorticoids | Detrimental
|
| Metformin | Protective
|
| Sulfonylureas | Protective
|
| Thiazolidinediones | Detrimental
|
| Dipeptidyl peptidase 4 inhibitors | Protective
|
| Insulin | Data mixed regarding protective or detrimental
|
| Statins | Data mixed regarding protective or detrimental
|
| Co-morbidities | |
| Type 2 diabetes mellitus |
|
| Chronic liver disease |
|
| Chronic kidney disease |
|
| Rheumatoid arthritis |
|
| Chronic gastrointestinal disorders (i.e., celiac disease, inflammatory bowel disease) |
|
Glucocorticoids are commonly prescribed for prevalent conditions in older adults including rheumatoid arthritis, polymyalgia rheumatica, giant cell arthritis, inflammatory bowel disease, and chronic lung disease. Glucocorticoids negatively impact bone through a multitude of pathways and are the most common cause of secondary osteoporosis . Glucocorticoids directly affect osteoblasts by altering protein synthesis and regulation. Additionally, glucocorticoids reduce the production of growth hormone and insulin-like growth factors, which are osteoblast stimulators. Glucocorticoids enhance bone resorption by increasing the production of receptor activators of nuclear factor kappa-B ligand (RANKL) and decreasing the production of osteoprotegerin. Finally, osteocytes cannot function appropriately and undergo more apoptosis with glucocorticoid treatment. Fractures are the most serious adverse effect related to chronic glucocorticoid use and are associated with an increased fracture risk as quickly as after the first dose . Glucocorticoids impact muscle strength and promote skeletal muscle loss, leading to an increased risk of falls and fracture as well. Specifically, glucocorticoids reduce sarcolemmal excitability, decrease serum levels of creatine kinase and myoglobin, and decrease the cross-sectional area and strength of certain myofibers. Additionally, glucocorticoid-induced protein catabolism contributes to muscle atrophy .
Antidiabetic medications are another class that influences bone, muscle, and fat. Studies have suggested that metformin improves bone quality and decreases the risk of fracture. A key molecule in metformin, AMP-activated protein kinase, is thought to be effective in signaling pathways in bone physiology, having direct osteogenic effects . Sulfonylureas increase insulin levels and may positively impact bone metabolism; for example, glimepiride enhances the proliferation of osteoblasts in animal models, though this has not been duplicated in humans. Another study, the ADOPT trial, suggests that patients treated with metformin and sulfonylureas had a similar rate of fracture; these results have been duplicated in other studies as well . However, thiazolidinediones influence gene expression for glucose and energy metabolism in adipose tissue, liver, and muscle . They activate peroxisome proliferator-activated receptor γ, suppress insulin-like growth factor, increase osteoclast formation, and decrease osteoblast formation; thus, these have been shown to increase fracture risk and decrease bone mineral density . Dipeptidyl peptidase 4 inhibitors may positively influence bone metabolism by reducing osteoclast activity and promoting bone anabolism and subsequent increase in bone mineral density in mice, however human clinical data suggesting this is limited . Finally, though animal studies suggest that insulin has a positive anabolic effect on bone metabolism, clinical data suggest an increased risk of both falls and fracture ; it is unclear if this effect in humans is direct or indirect due to hypoglycemia . Insulin therapy is associated with the highest risk of fractures of all antidiabetic medications, although whether this is mediated by the higher risk of hypoglycemia and falls or direct impact on muscle or bone is not clear .
Statins have been thought to positively influence bone metabolism, leading to modest increases in BMD. For example, a nationwide retrospective population-based cohort study in Taiwan suggests that long term use of high-potency statins is associated with a decreased risk of osteoporosis . However, other robust studies and reviews, including the JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin), suggests that statins do not reduce fracture risk . Though statins have been associated with decreased muscle strength and impaired balance, statins have been shown to be protective against falls. However, this may be secondary to its cardioprotective properties .
Chronic diseases associated with falls and fractures
The pathophysiology of certain chronic diseases places older adults at risk for changes in bone, muscle, and fat with a resulting increase in the risk of falls and fractures. These are also summarized in Table 1 .
Patients with type two diabetes mellitus have an increased fracture risk despite higher BMD, due to obesity, increased risk of falls, sarcopenia, co-morbidities, and antidiabetic drugs as noted above . In diabetic patients, advanced glycosylation end-products are toxic to bone tissue, and their bone microvascular system is impaired . In vitro, hyperglycemia leads to adipogenic differentiation instead of osteogenesis and enhanced apoptosis of osteoblasts . Obesity increases the risk and impact of falls, immobility, inflammation, vitamin D insufficiency, and adverse effects of adipose tissue on bone remodeling. Diabetic older adults have reduced muscle strength and impaired gait, independent of peripheral neuropathy or peripheral vascular disease; literature suggests that fat infiltrates muscles, and these patients have lower muscle density .
Patients with chronic liver disease are also at increased risk of sarcopenia, osteoporosis, and fracture. One study in Japan revealed an association with body mass index (BMI) in chronic liver disease, and suggest that BMI should be used to predict fracture in these patients . The exact mechanism remains to be elucidated; however, one hypothesis is that the imbalance between RANKL and osteoprotegerin in chronic liver disease and may be related to bone turnover and poor maintenance of bone homeostasis . Finally, cirrhotic patients may have higher serum myostatin levels; in vitro, myostatin accelerates RANKL mediated osteoclast formation and may be related to osteoporosis . Sarcopenia has been well-described with chronic liver disease, and is likely related to this increased myostatin, impaired mitochondrial function, and impaired fatty oxidation related to hyperammonemia .
It is well known that chronic kidney disease, mainly stages 3–5, is associated with increased fall and fractures in the setting of muscle weakness, neuropathy, polypharmacy, and renal osteodystrophy. The literature and the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines support BMD testing to assess fracture risk in patients with CKD stage 3a to 5 if it will impact treatment decisions .
Rheumatoid arthritis is also associated with an increased risk of osteoporotic fractures, not only because of treatment with steroids but also due to systemic inflammation. The effects of systemic inflammation adversely affect cortical and trabecular bone ; sclerostin and dickkopf-1 inhibit signaling pathways leading to reduced bone formation and regeneration . Muscle loss and adverse fat distribution also impact BMD in these patients . Limited studies suggest that cytokines and growth factors contribute to muscle wasting .
Finally, chronic gastrointestinal disorders are associated with osteoporosis and subsequently increased fracture risk. For example, patients with Celiac Disease who have persistent duodenal villous atrophy have increased fracture risk . Inflammatory bowel diseases (IBD) lend to malnutrition, for example, vitamin D and calcium deficiencies, and increase the risk of falling, developing osteoporosis, and sustaining fractures. Additionally, inflammatory cytokines such as interleukin 1 and 6 and tumor necrosis factor α may impact bone metabolism through increasing RANKL, which induces bone resorption .
Clinical tools to estimate fall and fracture risk
There are several validated clinical tools that allow the clinician to assess the risk of falls and fracture risks. For example, the FRAX (Fracture Risk Assessment) integrates risks associated with clinical risk factors and medications (including some with overlapping muscle/bone impacts discussed above such as rheumatoid arthritis, glucocorticoids, type 1 diabetes, chronic liver disease, malabsorption, and glucocorticoids) and BMI or BMD at the femoral neck. It is widely generalizable as it was developed from studying population-based cohorts from Europe, North America, Asia, and Australia. The FRAX predicts the 10-year probability of hip fracture and of a major osteoporotic fracture, adjusting for survival probability . Notably, FRAX does not include a history of falls which is consistently one of the strongest risk factors for fracture as outlined above and does not provide any assessment of muscle strength or function. The Garvan tool, in contrast, is driven largely by age, BMD, and fall history, and is highly predictive in an Australian cohort. When compared in a separate validation cohort, both calculators have similar, moderate predictive ability with AUCs between 0.60 and 0.70; the 2 tools over- or underestimated fractures variably for different populations, and neither was significantly better than age and BMD alone . The International Osteoporosis Foundation and International Society for Clinical Densitometry have published a position statement suggesting that a history of falls and frailty (which is highly associated with sarcopenia) should ideally be added to FRAX in the future and that in the meantime clinicians should consider these risk factors in addition to the FRAX score .
A commonly used tool to evaluate sarcopenia is the SARC-F questionnaire; its components are strength, assistance with walking, rise from a chair, climb stairs, and falls. Scores range from 0 to 10, and a score greater than four is predictive of sarcopenia . This screening tool is useful to prompt the clinician to pursue further diagnostic testing . Validation in some populations has suggested an association with subsequent disability, quality of life, and mortality , and the SARC-F score has added predictive value above FRAX for hip fracture risk .
The Centers for Disease Control and Prevention developed the “Stopping Elderly Accidents, Deaths and Injuries” (STEADI) initiative for healthcare providers to reduce fall risk. This toolkit has materials to help providers screen to identify older adults at increased fall risk, assess modifiable risk factors, and intervene with effective, evidence-based strategies. While outcome studies of multifactorial interventions have been mixed with regards to fall rates, fall-related injuries, and time of benefit, STEADI has been shown to be feasible and trends toward a decrease in fall-related hospitalizations . Notably, the 12-question self-assessment screening tool suggested by STEADI includes only 2 questions related to sarcopenia (difficulty rising from a chair without using arms, difficulty stepping onto a curve), but no questions related to fractures or bone density or the medications/medical conditions related to muscle and bone loss.
Tests to assess muscle quality and quantity exist but are not yet highly utilized clinically. For example, bioelectrical impedance analysis estimates fat-free mass; peripheral quantitative computerized tomography estimates bone structure, muscle cross-sectional area, intramuscular adipose tissue; magnetic resonance imaging measures small muscle volume; and finally, the D3-creatine dilution method measures muscle mass and has shown a strong relationship with falls and fractures in older men . However, these are relatively expensive, may use radiation, and their optimal use in clinical care has not been defined.
In contrast, physical performance tests are a simple, safe indicator of muscle strength and function that are suggested screening tests for older adults. Gait speed has a U-shaped association with falls, such that participants with faster (≥ 1.3 m/s) and slower (< 0.6 m/s) gait speeds are at higher risk than those with normal gait speeds . In contrast, gait speed has a linear relationship with hip fracture risk , suggesting that the falls in the high gait speed adults may be related to increased physical activity and opportunities for noninjurious falls. The Timed Up and Go (TUG) test is another commonly used screening test that assess hip flexor strength, gait speed, and balance. A metaanalysis suggests that this has poor sensitivity but reasonable specificity in identifying fallers, and its predictive value for future falls is limited . The Short Portable Performance Battery and the Performance-Oriented Mobility Assessment have the modest discriminative ability for fallers vs nonfallers and subsequent falls , but their predictive ability for subsequent fracture has not been well defined.
Potential for pleiotropic interventions to reduce both falls and fractures
Because of their clinical overlap, there is a potential for interventions that optimize the interplay between bone, muscle, and fat to subsequently decrease the risk of both falls and fractures. Nutritional interventions are of interest to many older adults. Increased protein consumption not only improves muscle mass but also may protect lumbar spine bone mineral density, especially during weight loss in obese older adults . Vitamin D is essential for muscle function and osteoblast activity, and several studies also support calcium and vitamin D supplementation (if meeting dietary recommendations) to reduce fall and fracture risk in the general population . The role of vitamin D in the pathogenesis and treatment of osteosarcopenia is summarized in Chapter 8 of this book.
Resistance and aerobic exercise have the most evidence for a pleiotropic beneficial impact on reducing age-related lean muscle mass and BMD loss. Specifically, resistance exercises stimulate osteoblastogenesis and muscle protein synthesis, which improves bone microarchitecture, muscle mass, strength, and functional capacity. Additionally, physical activity prevents intramuscular adipose tissue increases and its negative impact on muscle quality . There is strong evidence from randomized trials linking exercise interventions for both community-dwelling and institutionalized older adults to decrease falls, and at least in some studies, fractures . Whole body vibration on portable platforms has been studied as an alternative to weight-bearing exercise in light of the difficulty in sustaining exercise regimens in older populations. Data is mixed and generally low quality but suggests a possible beneficial impact on muscle strength, balance, bone density, and subsequent falls that should be confirmed in well-designed clinical trials. The role of exercise in the treatment of osteosarcopenia is summarized in Chapter 15 of this book.
Treatment of osteoporosis to reduce the risk of fracture is widely available. Pharmacotherapy includes antiresorptive agents (denosumab, bisphosphonates), anabolic agents (teriparatide, abaloparatide), antisclerostin agents (romosozumab), and hormonal agents (hormone replacement therapies, selective estrogen receptor modulators). Generally, these therapies treat bone alone but do not have clinically important impacts on muscle or fat composition. One trial has suggested that denosumab may impact muscle, based on improved handgrip strength and lean body mass .
No pharmacotherapy options have yet been approved for sarcopenia. However, bimagrumab (a monoclonal antibody that binds to activin type 2 receptors on skeletal muscle fibers), has been shown to induce muscle growth in cell culture and mice. A pilot study suggests that one dose in humans augmented muscle volume and lean body mass. Studies have been mixed regarding improvements in 6-min walking distance. Additionally, no significant changes were seen in quadriceps muscle strength, handgrip and pinch-grip dynamometry, and falls .
Conclusions
Falls and fractures are the most important clinical manifestations of osteosarcopenia in older adults, and preventing them is a critical public health goal. Screening and prevention efforts for both should include careful assessment and management of medications and co-morbidities that have a dual impact on muscle, fat, and bone. Current clinical tools do not fully capture the synergistic impact of muscle quality, bone quality, obesity, and prior falls on subsequent fall and fracture risk. We suggest using a combination of validated clinical risk tools, imaging, and brief physical performance testing to optimize management decisions. Exercise and dietary interventions are a key component of fall and fracture prevention; pharmacologic interventions targeting underlying osteosarcopenia are urgently needed.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree