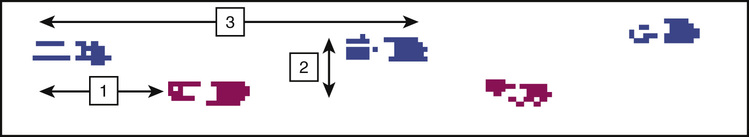
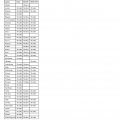
Stephanie Studenski, Jessie Van Swearingen Falls are a major focus of geriatric medicine because they are common among older adults, have complex interacting causes and serious consequences, and require multiple disciplines for effective management. The goals of this chapter are to present the scope and impact of the problem, explore various perspectives on causation, provide guidance about clinical evaluation and treatment, and examine opportunities to implement programs across health care settings and communities. Falls are common among older adults. Up to one third of community-dwelling persons older than 65 years fall annually, and about 20% to 25% of them will fall repeatedly.1 Falling is more common among women than men and increases in prevalence with advancing age. In acute care settings, falls are the most commonly reported adverse incident, with rates varying from 3 to 13 falls/1000 bed days.2 In chronic care settings, falls are so common that typically over 50% of residents are fallers; average rates can run from 1.5 to two to six falls/resident/year.3 The most obvious adverse consequence of falls are injuries, which develop in about 10% of community fallers and 30% of fallers in acute and chronic care.1,2,4 Injuries are more likely in recurrent fallers.1 Falls can be fatal; they are the fifth leading cause of death among older adults.1 Falls are a major contributor to serious injuries, including not only hip fractures but also other fractures, cervical spine injuries, and severe head trauma.5,6 Falls are a common precipitator of hospitalization and contribute to the need for long-term institutionalization.1,7 In acute and chronic care institutions, falls are also a source of complaints from families and even may lead to litigation.8 Although injuries and health care use are serious concerns, falling also creates other serious problems for the older adult, including functional limitations, fear of falling, restricted activity, and social isolation.1,8 Falling can be a precipitator of a vicious cycle of failing health and function, leading to death. In the past, there was no widely agreed on definition of falls. More recently, ProFaNE (Prevention of Falls Network Europe,www.profane.eu.org), a multinational work group dedicated to reducing falls and injuries through research and implementation of evidence-based interventions, has proposed the following as the most reliable and valid definition: “A fall is an unexpected event in which the participant comes to rest on the ground, floor or lower level.”9 Although this definition provides some consistency for reporting, there are still areas of confusion. It is not clear if it is appropriate to include in the definition of falls those events associated with loss of consciousness or overwhelming external forces, such as being hit by a moving vehicle. Similarly, it may or may not be important to include events such as a near-fall, in which the individual barely avoids a fall to the floor by suddenly grabbing for furniture or wall or is caught by another person. Frequent near-falls, such as stumbling and tripping, are risk factors for future falls. There are also problems with fall reporting. Fall events may not be remembered retrospectively, especially if there were no injuries. Prospective monitoring improves accuracy but can be burdensome. Although falls in general are important, it is possible that the most clinically relevant concern is the recurrent faller or a fall injury. There are also serious health-related concerns for those who does not actually fall because they have restricted their own activity. This group may also be at high risk for future falls, injuries, and social isolation. Another area of recent discussion has encompassed the role of exposure intensity in estimates of fall risk. Just as in estimates of automobile accidents, for which rates are adjusted for the exposure to miles driven, adjusting for physical activity intensity has been proposed as a more appropriate indicator of fall risk.10 Falling is considered a classic geriatric syndrome because it is often due to multiple interacting conditions that create an organism with reduced tolerance to any type of external stress. The evidence base that has been used to define the causes of falls is highly dependent on the perspective and priorities of the researchers, definitions of falling and fallers, time frame and approach to monitoring for falls, characteristics of the population under study, factors that were measured, and how interactions between factors were assessed in the analyses. Whatever the focus of the research, it is clear that many fallers demonstrate multiple abnormalities and that interactions among these abnormalities influence fall risk. Epidemiologic observational studies of older adults in the community and in acute and chronic care institutions have identified risk factors for falls; all suggest that risk increases as the number of risk factors increases. Table 103-1 summarizes risk factor profiles by the setting in which older adults were studied. Across settings, altered mobility and cognition are major risk factors for falls. Interestingly, it is possible to be too immobile to fall.11 For example, in one chronic care setting, residents with fair standing balance had the highest fall rates, those with good standing balance had intermediate fall rates, and persons with poor standing balance had the lowest fall rates.12 Risk factor patterns and appropriate preventive interventions may differ substantially by overall mobility capacity; active older adults may experience falls and injuries for reasons very different than those for persons who stand and walk with difficulty, who in turn may fall for very different reasons than those who cannot stand. TABLE 103-1 Predisposing Risk Factors for Falls in Older Person in Three Settings* Fall history Weakness Balance problem Gait problem Visual problem Mobility limitation Cognitive impairment Decreased functional status Postural hypotension Gait instability Agitated confusion Urinary incontinence and frequency Fall history High-risk medications Cognitive impairment Visual impairment Weakness Neurologic problems Gait and balance problems Cardiovascular problem Risk factors for injurious falls may differ from risk factors for all falls. In a study of older adults in residential care facilities, fracture risk among fallers was higher in those with better balance and no history of falls, perhaps suggesting that in some persons, activity increases the risk of producing sufficient force to fracture.13 Risk factor profiles are also limited in that they generally only identify chronic and stable risk factors, sometimes called predisposing risk factors. Many falls might occur because an individual with a predisposing risk has additional acute precipitating factors.14 For example, an older adult with limited mobility and cognition might not become a faller until he or she develops diarrhea, becomes dehydrated and dizzy, and tries to rush to the bathroom. Because risk factor studies have rarely accounted for these more transient and dynamic precipitating contributors, much less is known about them. Risk factors for falls overlap substantially with risk factors for other geriatric syndromes.15 Older age and impairments in cognition, mobility, and function are risk factors for falls, incontinence, delirium, and frailty.15 Thus, there is a population of older adults with multiple impairments who are at risk for numerous geriatric syndromes, including falls and injuries. There may be other populations of older adults who are at risk for different types of falls; active older adults may fall and injure themselves during demanding activities, whereas very immobile older adults may fall out of bed and chairs or even be dropped by caregivers. In the future, more distinct risk factor profiles might be defined based on overall mobility status. Epidemiologic studies have also identified environmental risk factors for falls. Virtually all falls can be considered the result of interactions between a person and her or his environment. The individual has some level of ability to move, and the environment has some level of challenge. The issue is the context in which the person and environment interact. The risk factors identified in Table 103-1 are sometime called intrinsic factors because they relate to the individual, and risk factors associated with the environment are sometimes called extrinsic factors. The typical older faller experiences a fall in an environment and while performing tasks that would not cause a healthy young person to fall. This phenomenon of falling under a low challenge is the rationale for believing that many falls in older people are due largely to intrinsic factors. If an older adult has many intrinsic risk factors, it is possible that only modest problems with the environment or modest degrees of challenge in a task will precipitate a fall. Table 103-2 lists environmental risk factors for falls. Commonly reported indoor environmental factors are uneven walkways, loose rugs, absence of grab bars in the bathroom, and poor lighting.16,17 Outdoor hazards are less frequently assessed but might be important, especially for more active older adults. Other extrinsic elements, such as the availability of help, may be an important factor in falls among persons living in the community and are even more likely to contribute to falls in an institutional setting.10 Additional risk factors for falls include psychological and attitudinal characteristics such as risk preference.11,18 Other risk factors for injury include osteoporosis, low body weight, and fall direction.19 TABLE 103-2 Environmental Risk Factors for Falls Poor lighting Loose or absent railings Throw rugs Trailing cords and wires Uneven transitions (e.g., level change between rooms) Lack of bars in the bathroom Slippery floors Cluttered walkways Uneven and broken sidewalks Wet surfaces Poor lighting Irregular steps Unpredictable level changes Contributors to falls can be examined from the perspective of physiologic systems that affect balance. The rationale for using a framework of organ-based physiologic systems that affect balance is based on models of disablement. These models draw links between pathologic processes and altered organ system performance (termed impairments), which combine to affect body movements (termed functional or performance limitations), then affect functional abilities and disability, and ultimately interfere with social roles such as being a homemaker or volunteer (termed handicap). There are several disablement models. When assessing causation of problems of aging, these multisystem physiologic approaches are helpful for several reasons. First, such approaches can address interactions between systems. Second, they can include mild or subclinical impairments that might affect function without being clinically obvious for an individual. Third, well-functioning systems might actually serve to compensate for problems with other systems. Thus, individual organ systems and even overall functions such as balance are on a continuum; they might be obviously abnormal, subclinically abnormal under usual conditions, abnormal only under stressful conditions, normal, or even have backup or reserve excess capacity. From a physiologic perspective, balance dysfunction results from impairment in one or more of the following systems: peripheral sensory receptors for input, central nervous system (CNS) structures for processing sensory input and planning motor output, and effector organs to carry out the movement plan (Box 103-1). In many situations, it is the combination of deficits across these systems that produces instability and falls. There are three main sensory systems used for balance—vision, somatosensation, and vestibular function. Visual functions such as acuity, depth perception, dark adaptation, contrast sensitivity, and peripheral vision help determine body position and trajectory in space and monitor the environment.20 Because bifocal glasses prioritize two focal lengths, one in the lower field at about 20 inches for reading and one in the upper visual field at about 20 feet for distance, bifocals can limit acuity in the critical zone in front of the feet while walking.21 Diseases of the aging eye that affect multiple visual functions are common; these include glaucoma, macular degeneration, and cataracts. Medications that cause miosis, or constriction of the pupil, can reduce dark adaptation. Peripheral sensation is important for balance. These sensors provide information about the position of the body relative to the support surface and gravity and reflect the relationship of one body part to another during rest and movement. Peripheral sensation is the most important system for monitoring the characteristics of the weight-bearing surface and distribution of body weight onto the feet. Peripheral sensory loss is common in older adults due to diabetes and peripheral vascular disease. In case of peripheral sensory loss, visual systems can compensate by supplementing information about body position. Thus, a combination of vision loss and peripheral sensory loss can create serious problems with the ability to monitor body position. The vestibular system detects the position of the head with respect to gravity, monitors linear and angular acceleration of the head, and coordinates head and eye movements to maintain gaze and visual field stability while moving. Vestibular system impairments can occur with usual aging and are affected by ischemia or head trauma.22 Several widely recognized vestibular conditions, such as benign paroxysmal vertigo and perhaps Meniere disease, are common in older adults. Others are also common but less well recognized, such as chronic bilateral vestibular hypofunction.23 The CNS has numerous structures that contribute to balance. Structures in the brainstem and spinal cord are considered central pattern generators that produce stepping behaviors. Balance is further controlled by higher level brain structures, including the frontal cortex, basal ganglia, cerebellum, and motor cortex. Degeneration of brain regions can affect balance, as in the basal ganglia in Parkinson disease and in cerebellar degeneration. All brain processes depend on adequate levels of brain perfusion, so any threats to perfusion affect central processes of gait and balance. Thus, many of the conditions that produce syncope or presyncope can cause transient cerebral hypoperfusion and falls, such as orthostatic hypotension, tachyarrhythmias, bradyarrhythmias, and critical aortic stenosis.24 There has been increased awareness of the role of more diffuse microvascular brain disease as a contributor to balance disorders and falls.25 This mechanism is posited to involve ischemia in vulnerable brain areas, especially the frontal lobes, and in important white matter tracts connecting the frontal lobes to critical subcortical areas. Radiologically, this ischemia is manifested as leukoaraiosis (white matter disease) on magnetic resonance imaging scans. White matter disease has been associated with specific patterns of cognitive dysfunction involving psychomotor slowing and altered attention and executive functions, such as sequencing and visual spatial organization.25–27 These cognitive abnormalities have been associated with alterations in gait, especially excessively variable length and timing of stepping, and with falls.28,29 Thus, there is an emerging concept of altered balance and gait due to abnormal nonamnestic cognitive functions and movement planning produced by regional microvascular brain disease. This condition may be manifest by irregular walking patterns and exacerbated by placing stress on cognition and movement. Tasks that simultaneously stress cognition and movement are part of an emerging conceptual approach to balance assessment termed dual tasking.30,31 Older adults whose performance worsens substantially when asked to walk and solve cognitive problems simultaneously may be at increased risk for falls.32 The CNS also operates a multisynaptic righting reflex that produces automatic correcting movements when balance is lost. Typically appearing as a stepping response that occurs much more quickly than what can be done voluntarily, this righting reflex is lost in many CNS disorders, including extrapyramidal diseases and other forms of multisystem atrophy. Sedation, clinical or subclinical, may further reduce alertness and attention. Thus, both sleepiness and sedative medications have been found to increase fall risk.33,34 Less specific but potentially important are psychological factors, such as fear of falling and risk preferences.11,35 Muscles and joints are effector organs critical for balance and mobility. Muscle weakness is widespread in older adults and can be due to primary muscle mass loss (sarcopenia), disorders of peripheral nerves or neuromuscular junctions, or inactivity. Specific muscle diseases such as inflammatory myositis or steroid myopathy can produce proximal muscle and trunk weakness that presents with falls. Lower motor neuron conditions, radicular nerve deficits due to spinal stenosis, or peripheral nerve damage can result in localizing strength deficits that affect specific muscle groups and more distinct functional movements. For example, a foot drop due to damage to the peroneal nerve prevents the forefoot from lifting to clear obstacles and can induce trips and stumbles. Evidence has suggested that low vitamin D levels may contribute to muscle weakness and falls.36 Low testosterone levels have been found to be associated with falls in men younger than 80 years.37 Other common conditions such as arthritis can reduce range of motion and produce pain that alters stepping and weight bearing.38 Deformities distort the weight-bearing surfaces of the foot and cause pain. Fatigue, generalized or localized to muscle, can contribute to loss of balance. Thus, acute conditions such as overworked muscles or chronic conditions associated with fatigue such as anemia39 or congestive heart failure might increase risk for falls. Although traditional assessments of strength have focused on the extremities, more recent thinking has emphasized the role of trunk or core strength involving the abdomen and pelvis as critical to postural control, which is a novel avenue to pursue interventions.40 When fall onset is abrupt or there is a major change in balance, the likelihood is higher that there is a medical event that has affected the CNS. Any illness or episode that reduces cerebral perfusion through hypoxia, decreased oxygen-carrying capacity, or hypotension could present as dizziness, lightheadedness, unsteadiness, and falls. Toxic or metabolic abnormalities due to medications, infection, or electrolyte disorders could present as unsteadiness and falls through effects on attention. New focal neurologic deficits due to stroke can also present as unsteadiness. Older adults with predisposing subclinical balance disorders could be more vulnerable to such precipitating factors. These types of physiologic acute, and sometimes transient, changes are harder to include in research studies because stable chronic effects are usually the focus of an investigation. A biomechanical approach to fall risk is based on the concepts of mass, force, momentum, and acceleration of the body as a whole, as well as of body segments. The standing human body is a long tall column that rests over a small base of support. The main task of movement is to displace and recover this column while the base of support changes. Therefore, the assessment of balance includes two main conditions: (1) static balance, defined as steadiness of the fixed column over a constant base of support; and (2) dynamic balance, defined as control of the column and supporting structures during movement. The most essential and classic dynamic balance task is walking. Walking involves alternating the use of one leg to support the body while the other swings from behind to in front of the body. There is an extensive knowledge base about normal and abnormal walking based on a set of biomechanical characteristics; it uses a specialized terminology. Walking can be characterized by the pattern of steps using spatial factors such as step length, stride length (distance between two heel contacts from the same foot), and step width (Figure 103-1). Walking can also be characterized by temporal factors such as double support time (the duration of the stride when both feet are on the ground at the same time) and cadence (step frequency). Walking has been described as controlled falling because the body column moves forward past the base of support, and the feet must be timed to contact the support surface at the right location and time in anticipation of the moving location of the trunk.41 When this timing is altered by disease, gait becomes irregular, and trunk movement can be altered. Walking can also be characterized by changes in other body segments and joints. During normal walking, the foot begins a step with a push-off from the toe, lifts the foot to swing through, and ends with a heel strike and forward rolling foot contact to initiate the next push-off. The knee is in full extension at the time of toe push off, swings forward with slight flexion to aid foot clearance and then returns to full extension at the point of heel contact. The hip is in extension behind the trunk at push off and swings into flexion at heel contact. The arms swing alternately and in a sequence opposite to the step sequence of the legs. Biomechanical factors that have been found to be abnormal in fallers encompass both static and dynamic balance. Abnormal static balance associated with falling is manifested as increased sway during quiet standing. Some studies have suggested that increased sway to the side, or mediolateral plane, is especially associated with falls.42 Alterations in dynamic balance among fallers are diverse, depending on the underlying cause. Frequently observed abnormalities include prolonged double support time during walking, increased step width, increased trunk sway during movement, increased or decreased toe clearance, reduced hip extension, abnormal lateral stepping, and delayed correcting movements at the hip or ankle when the trunk is displaced.43,44 Screening for fall risk has two main goals, to identify persons at high risk and identify remediable factors for intervention. Screening for risk alone can be more efficient than assessment for modifiable factors, so screening sequences that first identify risk and then assess remediable factors may make the best use of scarce resources. Because fall risk varies by population and type of fall, there is unlikely to be a single screening approach that works well in all settings. Certainly in diverse community populations, it makes sense to identify groups who are at low risk and who therefore can be spared more detailed, time-consuming assessments. The American Geriatrics Society and British Geriatrics Society have recommended fall screens that identify risk as the following: (1) more than one fall in the last year; (2) one or more falls with injury; (3) self-report of unsteadiness; or (4) unsteadiness on performance testing.45 Many older adults do not complain about falling to health care providers, so it is important to ask about falls explicitly. Some older adults fail to report falls because they have forgotten them, and some may actively hide the fact that they are falling because they worry that the family or health care provider will insist on relocation or activity restrictions. Screening in chronic care settings differs from screening in primary care. In chronic care settings, fall rates are often high, and screening tool are more likely to have high false-negative rates. If prevalence is very high, it may be sensible to consider almost everyone as high risk and act accordingly. Fall risk screening in acute care is a high priority, but some have argued that no screening tool is accurate enough to justify the current investment in detailed admission fall screening because it consumes much nursing staff time, with little real benefit.46 In addition, general screens for functional problems in acutely ill, hospitalized older adults may do as well at predicting falls as more specific fall screens, and general screens can be used for a number of nursing issues.47 There is some evidence that nursing global judgment is comparable in accuracy to formal screening tests in some chronic care settings.48 There are two main types of screening tools—those based on professional assessment of various historical and health factors and those based on observed performance of mobility and balance tasks. Some of the more common tools are described in Table 103-3. There are no clearly superior tools that have been shown to have high accuracy in multiple settings, so the optimal tool must be tailored to the population, goals of screening, and time and other resources available. TABLE 103-3 Scales Used for Fall Risk Screening and Balance Assessment Among persons who can stand without assistance—poor balance or two of three the following: fall history, nursing home residence, urinary incontinence Among persons who cannot stand without assistance—one of three of the following: fall history, hostel residence, use of nine or more medications
Falls
Introduction
Epidemiology
Causation
Epidemiologic Perspective
Community Dweller
Acute Care
Chronic Care
Indoor Falls
Outdoor Falls
Physiologic Perspective
Biomechanical Perspective
Screening
Instrument
Items
Setting
Community
Acute
Chronic
MULTIFACTORIAL REPORTS
STRATIFY71
Five items—history of falls, agitation, visual impairment, frequent toileting, able to stand but needs assistance with moving
X
X
Morse Fall Scale72
Six items—history of falls, secondary diagnoses, parenteral therapy, use of ambulation aids, gait, mental status
X
X
FROP-Com73
13 risk factors in 26 items—fall and fall injury history, medications, medical conditions, sensory loss, feet, cognitive status, toileting, nutrition, environment, function, behavior, balance, gait; total score, 0 to 60; fall risk high with score > 24
X
Fall risk for residential care74
X
Functional Mobility
Berg Balance test50,75
14 tasks scored 0 to 4; total range 0 to 56; fall risk increases as score decreases
X
X
X
Functional reach76
Distance reached in inches without moving the feet; fall risk < 7 inches
X
X
X
Performance-oriented mobility and balance77
Balance subscale score 0 to 16, gait subscale 0 to 12, summary score 0 to 28; summary score < 19 indicates high fall risk
X
X
Timed up and go78
Time in seconds to rise from a chair, walk 3 m, turn, walk back, and sit down; <10 sec normal; fall risk increases with time > 13.5 sec
X
X
Dynamic gait index51
Eight walking tasks scored 0 to 3, total score 0 to 24; <18 or 19 indicates fall risk
X
Functional mobility tests79
Time to complete eight step ups (alternate step test) > 10 sec, timed sit to stand five times > 12 sec, 6-m walk time > 6 sec increased fall risk
X
Physiologic profile assessment80
Performance in five domains: sway, reaction time, strength, proprioception, contrast sensitivity; total score 0 to > 3; fall risk increased with score ≥ 2
X
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Falls
103