Fig. 27.1
AP pelvis X-ray of a right displaced femoral neck fracture
Plain radiographs with anteroposterior and lateral are sufficient to diagnose fracture in 98 % of cases. MRI is a low-radiation, high-sensitivity and high-specificity alternative when there is a high suspicion of fracture without conclusive findings on X-ray [74]. Treatment plan and outcome measures are correlated with displaced vs. non-displaced fracture features [75]. Eighty-five percent of femoral neck fractures are displaced at the time of diagnosis [23].
Non-displaced [76] or valgus-impacted femoral neck fractures are generally treated with percutaneous pinning using a cannulated screw system (Fig. 27.2) [77]. Patients can bear weight as tolerated after surgery and should be followed with serial radiographs to evaluate union [78, 79].


Fig. 27.2
AP pelvis X-ray of percutaneous screws for fixation of a valgus-impacted femoral neck fracture
There is a high risk of complications treating non-displaced fractures nonoperatively. Rates of subsequent displacement range from 19 to 46 % [80–82]. Ultimately, these complications lead to worse outcomes overall than operative treatment. Thus, nonoperative treatment should be reserved for those patients whose comorbidities make them very poor candidates for surgery or nonambulatory patients in a palliative care setting. Additionally, patients may elect to try nonoperative treatment, but should be made aware of the alternatives [83].
Displaced femoral neck fractures are typically treated with hemiarthroplasty or total hip arthroplasty (Fig. 27.3). These procedures eliminate the risk of nonunion and fixation failure by using a prosthesis to bridge the joint space. Prostheses may be cemented or uncemented. Cemented femoral components may offer a decreased risk of intraoperative fracture and improved postoperative function over many uncemented components; however, comparative studies are not available for current generation uncemented systems [84–87]. These procedures are performed with the patient in a lateral position through either the lateral or posterior approach to the hip. The posterior approach preserves abductor strength better, but the lateral approach gives a lower risk of postoperative dislocation. The selection of procedure and implant type depends on patient demographics, baseline function, and functional goals.


Fig. 27.3
AP pelvis X-ray of a bipolar hemiarthroplasty for treatment of a displaced femoral neck fracture
In unipolar hemiarthroplasty, the femoral neck and head are replaced by a non-modular implant. The modularity of bipolar hemiarthroplasty is thought to provide an advantage over the unipolar design. In bipolar hemiarthroplasty, an inner head articulates with a shell that in turn articulates with the acetabulum. In theory, this reduces wear and acetabular protrusion (femoral head migration into the pelvis) [88–91]. The modularity of a bipolar system allows the surgeon to test a variety of head/neck options in order to optimize stability. Despite these theoretical advantages, results are comparable with unipolar hemiarthroplasty [92, 93].
Total hip arthroplasty has been shown to have better outcomes for treatment of displaced femoral neck fractures in cognitively intact patients [94]. This comes at a risk of a higher dislocation rate [95]. Total hip arthroplasty is a longer and more complex procedure, and may have higher cost [96]. Although the procedure is more complex than hemiarthroplasty or percutaneous screws, 30-day mortality is low at 2.4 % [97]. Long-term mortality and reoperation are low at 12 and 5 %, respectively. All of these data compare favorable to other methods of treatment. Rates of complication are understandably higher for secondary total hip arthroplasty to revise failed internal fixation [86, 98–100].
In conclusion, non-displaced femoral neck fractures should be treated with percutaneous screw fixation. Displaced femoral neck fractures in the elderly should be treated with replacement, either hemi- or total hip arthroplasty. This decision is based on age, activity level, and cognitive status of the patient [101–105]. Patients with preexisting hip arthritis may also benefit from total hip arthroplasty [106, 107].
Intertrochanteric Fractures
Intertrochanteric fractures are extracapsular, proximal metaphyseal fractures between the greater and lesser trochanter. In older patients, these injuries are predominantly due to low-energy trauma such as falls from standing height [108, 109]. The greater and lesser trochanters and the intertrochanteric region are sites of extensive muscle attachment, and fractures in this region are subject to considerable stress. Stable anatomic reduction and fixation are the paramount challenges of treating fractures in this functionally essential region [110, 111].
Nonoperative treatment is reserved for patients with very low baseline function or very short life expectancies where medical palliation is adequate to control pain. Patients should be quickly mobilized to an upright position to minimize the risks of prolonged bedrest [112].
Operative fixation of intertrochanteric hip fractures is the standard of care. For stable fractures, which are either non-displaced or displaced but a stable fracture pattern, a sliding hip screw is often preferred (Fig. 27.4a, b) [113, 114]. Sliding hip screws are designed to provide dynamic compression across the fracture to enhance stability and healing. If additional rotational stability is required, an additional screw can be placed in the femoral neck, parallel to the sliding screw system [115]. If possible, a closed reduction to anatomic position is achieved under fluoroscopy. Otherwise, open reduction is performed. The sliding screw system is placed using a lateral approach to the proximal femur. Guide wires placed under fluoroscopy are used to direct the screw in the correct position, and a plate is placed over the screw and secured to the femur [23, 116]. The typical mode of failure is cutout, which occurs in 4–7 % of patients. Reoperation is required in around 4 % of patients [23].
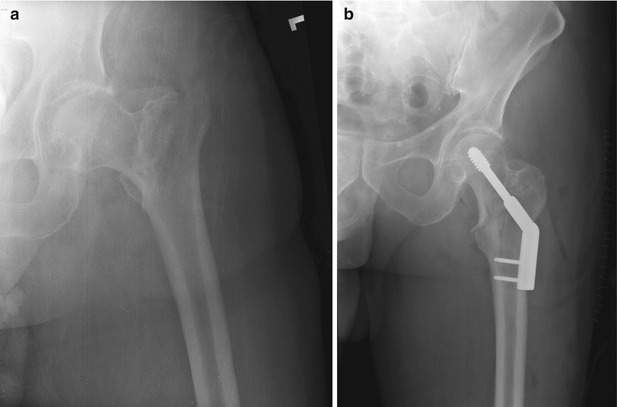
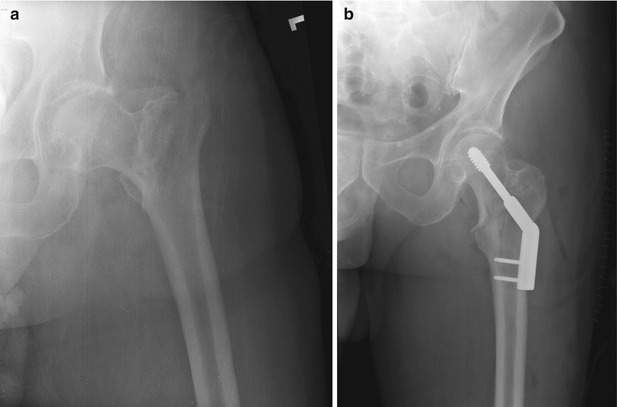
Fig. 27.4
Pre- (a) and post- (b) operative radiograph of a stable intertrochanteric hip fracture fixed with a sliding hip screw
For unstable fractures, an intramedullary device should be chosen to avoid excessive settling of the fracture (Fig. 27.5a, b) [117, 118]. The intramedullary approach requires a small incision over the proximal femur, marked with a guide wire under fluoroscopy. The nail is stabilized by an interlocking screw or blade extending into the femoral neck and head [119, 120]. This design provides linear compression across the fracture, and the nail itself provides a buttress for the fracture to settle against. Nails vary in length, curvature, and diameter. Care must be taken to select the implant that will optimally reduce and stabilize the patient’s fracture [23].
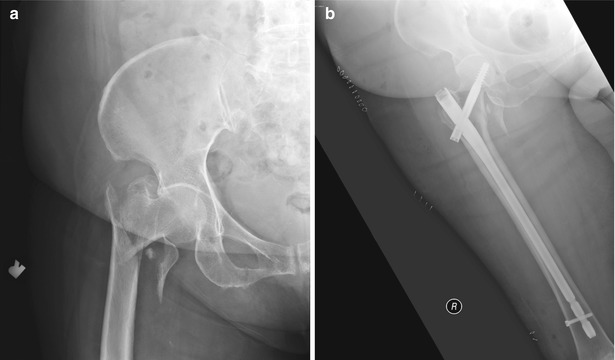
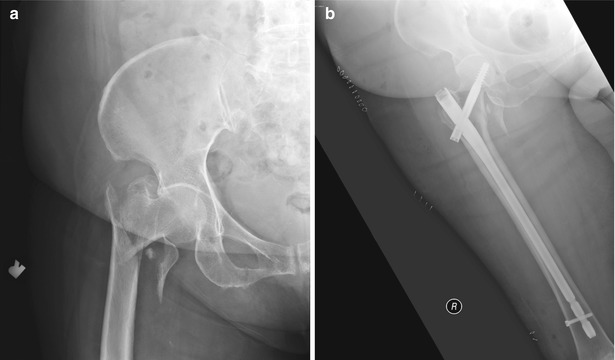
Fig. 27.5
Pre- (a) and post- (b) operative radiograph of a stable intertrochanteric hip fracture fixed with a sliding hip screw
After fixation of both stable and unstable intertrochanteric fractures, patients can begin weight bearing as tolerated with a walker or crutches [121].
Subtrochanteric Fractures
Subtrochanteric fractures are less common than femoral neck and intertrochanteric fractures, but are a significant surgical challenge. These fractures occur in the proximal femur, distal to the lesser trochanter by up to 5 cm (Fig. 27.6). In elderly patients, the majority of subtrochanteric fractures are due to a simple fall [122, 123]. Due to enormous compressive, tensile, and torsional stresses in the region, deformation of the fracture segments is common. Often the proximal segment is deformed by the action of the hip flexors and abductors. The distal segment is subject to the action of adductors and knee extensors. Furthermore, the region is poorly vascularized, posing another obstacle to successful union [23].


Fig. 27.6
AP femur X-ray of a left subtrochanteric hip fracture
A unique pattern of subtrochanteric fractures associated with bisphosphonate therapy has emerged in recent years. These are short, oblique fractures of the metaphyseal junction showing lateral cortical thickening and a medial cortical spike (Fig. 27.6). Patients can report prodromal symptoms prior to the fracture event. The proposed mechanism behind this is impaired healing of a stress reaction in the subtrochanteric region due to the bisphosphonate-induced inhibition of osteoclasts, which are normally required for fracture remodeling [124].
All subtrochanteric fractures are treated operatively unless a severe comorbidity precludes this. Operative treatment is typically with intramedullary nail (Fig. 27.7) [122, 125]. The same percutaneous approach for intramedullary nailing is used as was described for intertrochanteric fractures. Reduction is achieved under fluoroscopy and the nail inserted in the prepared canal. Most nailing systems will offer a choice of locking mechanisms, with a cephalomedullary locking device preferred in an unstable, osteoporotic fracture or any fracture without an intact lesser trochanter. A single large lag screw or 2 smaller screws directed into the femoral head may offer added protection of the femoral neck in osteoporotic patients [126]. Otherwise, a standard greater to lesser oblique trochanteric-locking screw can be placed through the nail [127].


Fig. 27.7
AP femur X-ray of an intramedullary nail for treatment of a left subtrochanteric hip fracture
Patients are made weight bearing as tolerated after fixation with an intramedullary nail. Subtrochanteric hip fractures, as with other fractures around the hip joint, are associated with significant morbidity and mortality. Although they make up a small minority of proximal femoral fractures in the orthopedic trauma unit, these fractures are typically complex to treat and may be associated with an underlying pathologic cause.
Mortality After Hip Fractures
Unfortunately, mortality after hip fracture is surprisingly high. It is clear that hip fractures are truly a surgical problem as the early mortality is almost double compared to nonoperative treatment of hip fractures [128]. Richmond et al. [129] reviewed 830 patients with hip fractures and found the highest mortality was within the first 3 months. Younger patients (age <85) also had a higher mortality, as were patients with a higher ASA classification. The in-hospital mortality was 3 %. The one year mortality rates in multiple studies are varied, but estimate a 30 % 1-year mortality. This is higher for cognitively impaired patients (50 %) and lower for cognitively intact patients (12 %) [23].
More than the fracture itself, the broken hip is a marker for declining functional and physiologic status. This is evident because the most common causes of death after hip fracture is not a complication from the broken bone, but circulatory disease, followed by complications of dementia. The risk of mortality in hip fracture patients is 3 times higher than in the general population [130].
Return to Functional Status
Return to baseline ambulatory status and living situation is dismal after hip fracture. Sixty percent of patients lose a level of ambulatory mobility at 1 year, i.e., community ambulators return as household ambulators after hip fracture surgery. Patients who are younger than 85 years, have lower ASA, or have a lower preoperative ambulatory status (low demand) are more likely to return to their baseline function [131]. Seventy-five percent of independent community ambulators are able to return to their pre-injury living status [57].
Acetabular Fractures
The dogma states that nonoperative management of displaced acetabular fractures in the elderly gives poor results. This is true for the younger population, but it is not necessarily true for the older population, that has less functional demands. Operative treatment of acetabular fractures in the elderly generally gives good results, but it is unclear whether there is an improvement over conservative management. There are currently no published data on operative versus nonoperative treatment of acetabular fractures in the elderly.
The fracture patterns in the elderly are different and often more complicated than in the younger population (Fig. 27.8). This is because of poor bone quality, which leads to more comminution and femoral head impaction, both of which can impact the ability to accurately repair these fractures [132]. In certain instances, fracture characteristics are predictive of early failure, such as impaction of the superior acetabular dome [133].


Fig. 27.8
AP pelvis X-ray of a displaced right acetabular fracture
Evaluation of these patients in the emergency department should parallel the evaluation of the hip fracture patient. Radiographic studies should include an AP pelvis and Judet (obturator and iliac oblique) radiographs, as well as a CT scan with coronal and sagittal reconstructions. The technology of 3-dimensional imaging has improved our understanding of these fractures and can be a useful teaching tool.
The decision whether to operate should be based on patient physiologic age, activity level, medical comorbidities, preexisting arthritis, and whether the operation can be preformed safely. Conservative management for most acetabular fractures in the elderly can be considered, with the exception of fracture patterns with posterior instability. Despite having relatively poor results with operative management, posteriorly dislocated or subluxated hips should be surgically stabilized [134]. Other fracture patterns, including those with medial wall protrusion into the pelvis, can be managed nonoperatively. Operations for acetabular fractures are significantly more complex than surgery for hip fractures.
Nonoperative Management
Spencer et al. [135] retrospectively evaluated 23 patients treated nonoperatively with radiographic and functional outcomes. This study is often quoted as having “poor results,” but the authors’ outcomes are not validated and the measures do not stand up to today’s standards. Letournel and Judet, the pioneers of acetabular surgery, reported on their results with operative fixation of acetabular fractures [136]. Although they did use validated functional outcomes, they only reported on 10 patients over the age of 70 years and could not make any conclusions about patients in this age group (fractures of the acetabulum).
Operative Management
Several authors have reported good results with operative management of these fractures. Carroll et al. [132] suggested an algorithm for treatment of this patient population. They recommended all patients with displaced fractures that would require less 3–4 h of operative time should be fixed with primary open reduction internal fixation. If the surgery was expected to take longer than 4 h, they recommended acute total hip arthroplasty. They reported good functional results with primary fixation of the fracture, but 30 % went onto total hip arthroplasty at 2.5 years. They did not report on a nonoperative cohort. Obviously, there is much variability in how much a given surgeon can accomplish within a 4-h window.
Leflamme et al. [137] recently reported their cohort of 21 patients stabilized using a slightly different approach, but nonetheless primary fixation of the fracture. They also reported good functional results comparable to previous studies, but reported anatomic reduction in only half of their patients, which has been correlated to functional results.
Traditional approaches and fixation methods can result in significant blood loss and potentially increased morbidity. Gary et al. [138] have reported on percutaneous fixation of these fractures. Since anatomic reduction is only possible in approximately half of the patients, this group advocates getting general alignment of the columns of the acetabulum and fixation with percutaneous screws (Fig. 27.9). In a retrospective review of 43 patients, they reported similar functional results and conversion rates to total hip arthroplasty as standard open reduction internal fixation, with fewer medical complications.


Fig. 27.9
AP pelvis X-ray of a percutaneously treated acetabular fracture
There are no studies comparing standard open reduction internal fixation to closed or limited reduction and fixation. The option of percutaneous fixation of acetabular fractures in the elderly may also provide pain relief and improved mobilization, which is critical in this population. However, objective data is lacking.
Comparison of Operative Versus Nonoperative Care
Several studies have been presented (but not published) on operative versus nonoperative care for these patients. Lucas et al. [139], in a retrospective study, reported that the 1-year mortality was less for the nonoperative group (15 % vs. 35 %) and the return to baseline living arrangements better in the nonoperative group. There was no difference in the ability of either group to return to baseline ambulation. Only 40 % of patients in either group were able to return to their baseline ambulatory status.
Ryan et al. presented data suggesting that hip function scores and general health scores are equivalent when comparing operative versus nonoperative treatment. The results continued to be not statistically significant when controlling for fracture pattern. A flaw of this study was that the conservatively treated patients were significantly older and had more medical comorbidities, which may mean they were lower demand [140].
Total Hip Arthroplasty
There are certain fracture patterns in the patient population, which are prone to failure, as defined by the need for conversion to total hip arthroplasty [133]. Some surgeons question whether the best operation for these patients should be immediate total hip arthroplasty to avoid a second surgery.
Mears and Velyvis [141] reported on 57 patients who underwent acute hip replacement, and 80 % had good-to-excellent outcomes at 8 years of follow-up. Herscovici et al. [142] reported complication rates, surgical times, blood loss, and length of stay were similar to primary fixation.
There are no reports directly comparing the spectrum of options including standard surgical treatment, percutaneous fixation, acute total hip arthroplasty, and nonoperative management.
Periprosthetic Fractures
With the increasing number of total hip and total knee replacements being performed, the incidence of periprosthetic fractures is increasing [143]. These fractures are difficult to manage secondary to poor bone quality and the presence of a prosthesis already in the bone, which may or may not be well fixed.
Preoperative workup should mirror that done for a hip fracture patient previously described. It is important to obtain operative notes from the replacement surgery in order to plan for any revision of the components if necessary.
Imaging should include radiographs of the entire extremity, being sure to include the prosthesis. If possible, it is important to compare previous radiographs of the extremity before injury to see if there are any subtle changes in the prosthesis, which would indicate loosening of the implant.
The principles of management are based on whether the prosthesis is stable or loose. Sometimes it is not possible to know whether a prosthesis is loose until testing it in the operating room, so one should be prepared to both fix the fracture and revise the prosthesis if necessary.
Fractures Around a Total Hip Replacement
The most useful classification is the Vancouver classification, which is both reliable and valid [144]. Fractures around the greater or lesser trochanters (Vancouver A) are typically minimally or non-displaced and can be managed nonoperatively [23]. If the fracture affects the stability of the prosthesis, fixation of the fracture or revision of the prosthesis is required.
Fracture at or around the shaft of the prosthesis is classified as a Vancouver Type B. Fractures can either involve a stable prosthesis (Fig. 27.10) or an unstable prosthesis. Fractures with well-fixed prostheses can undergo primary bone fixation with retention of the prosthesis (Fig. 27.11), while those that have loose prosthesis require revision.



Fig. 27.10
AP femur X-ray of a fracture around a hip prosthesis with a stable implant

Fig. 27.11
AP femur X-ray of fixation of a periprosthetic fracture
There is limited data on comparisons of techniques, but general principles include using implants with sufficient length and stability and preserving the biology of the fracture if possible [143]. There are multiple options for fixation of these types of fractures, which include plate and screw fixation [145], cable plates [146], and with or without allograft struts for support [147].
Postoperative care should involve immediate mobilization. Unfortunately, restricted weight bearing is usually necessary given the poor bone quality and limited fixation around a prosthesis.
Union rates have been reported as high as 85–100 % [148, 149]. Ricci reported 75 % of patients returned to baseline functional status [147]. Mortality after periprosthetic fracture has not been extensively studied as in the hip fracture population, but the 1-year mortality has been reported at 11 % [150].
Fractures that are distal to the prosthesis are classified as a Vancouver Type C. Without the hip prosthesis, these fractures are typically treated with an intramedullary nail. With the prosthesis in place, this is not an ideal construct as it leaves a stress riser between the nail and the prosthesis. Thus, the treatment should be with a laterally based plate that spans the hip prosthesis proximally (Fig. 27.11).
Fractures Around a Total Knee Replacement
Fractures around a total knee replacement happen twice as frequently around the femoral prosthesis than the tibial or patellar (Fig. 27.12). Risk factors for fracture include osteopenia, osteolysis (wear of the prosthesis), and technical errors such as notching of the anterior femur [23]. Treatment of supracondylar femur fractures around a total knee prosthesis is also based on whether the component is stable or unstable.
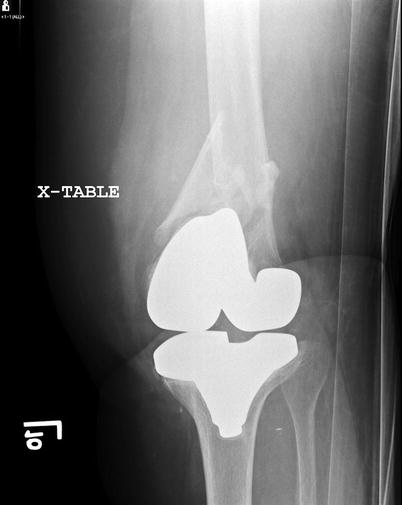
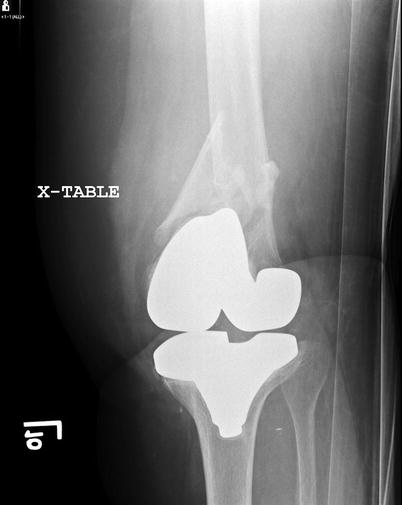
Fig. 27.12
AP knee X-ray of a periprosthetic femur fracture above a knee replacement
The goals of treatment include restoration of alignment and early return to function Non-displaced, stable supracondylar femur fractures can be managed nonoperatively in low-demand patients [151]. Operative fixation gives the advantages of immediate range of motion, earlier weight bearing, and less risk of late displacement. All displaced distal femur fractures are indicated for surgical stabilization.
Displaced fractures can be treated with either lateral locked plating (Fig. 27.13) or intramedullary nailing. Results were similar in a comparison of a small group of patients [152].


Fig. 27.13
AP knee X-ray of fixation with lateral plating of a periprosthetic femur fracture. In this instance, a second (intramedullary) plate was used for added stability
Intramedullary nailing of these fractures is challenging. Meticulous preoperative planning is necessary, as the surgeon must be familiar with the type and dimensions of the implant to ensure that the nail will pass [153]. There must also be enough bone stock in the distal segment in order to support the interlocking screws. In addition, placement of additional fixation (i.e., blocking screws) may be necessary in order to achieve and maintain alignment [23].
Lateral locked plating has also been reported to successfully treat these fractures [154]. Because of osteoporotic bone, supplemental fixation may be necessary to help avoid varus collapse (Fig. 27.13).
If the implant is loose, revision total knee surgery is required. This surgery is technically challenging and is often best accomplished by an experienced arthroplasty surgeon. Revision involves not only fixing the fracture but also ensuring stability and alignment to the knee [151].
Upper Extremity Fractures
Although upper extremity fractures in the elderly are not typically life-threatening, the resultant impairment may be so functionally debilitating that the injured patient can no longer manage independently. The majority of such upper extremity fractures may be treated nonoperatively. However, the physician must be aware of the potential consequences of prolonged immobilization on the entire limb. Locking plate technology is particularly suitable for providing stable fixation in poor bone, permitting early mobilization, and functional recovery.
Distal Radius Fractures
Distal radius fractures in the elderly are quite common. The incidence rate increases with age and is highest in patients 80 years and older. These typically occur as isolated, low-energy injuries resulting from a fall onto the outstretched hand. However, a neurovascular examination is essential, focusing on the median nerve. Preexisting carpal tunnel syndrome may be exacerbated by the energy of injury and/or the displacement of the distal radius. Concomitant progressive or severe median nerve dysfunction is an indication for urgent carpal tunnel release; in such instances, the fracture is usually stabilized with plate fixation.
The method of treatment of displaced distal radius fractures in the elderly population remains controversial. While restoration of anatomy is a goal of treatment in the younger patient, the relevance of such an approach in the elderly is unclear. A prospective, randomized study [155] comparing closed reduction and cast treatment with open reduction and internal fixation using a volar locking plate demonstrated better grip strength in the operatively treated group; however, there was no difference in wrist motion, pain, or function at 1 year between the two groups. Although 78 % of nonoperatively treated patients had a visible deformity (prominent ulnar head), none of them was dissatisfied with the clinical appearance or the result. The complication rate in the surgical group was 36 %, including tendon ruptures. Similar results have been reported retrospectively in an analogous patient population [156].
Interestingly, the patients treated surgically reported better function during the first 3 months following injury. This is not surprising, since nonoperatively treated distal radius fractures are casted for approximately 6 weeks, whereas patients may be placed into a removable splint soon after plate fixation. This highlights the importance of patient factors in the decision-making process. Older patients who are living alone may be able to retain their independence if treated surgically.
When the decision is made to operate, a number of options are available for fixation. As a rule, percutaneous pin fixation is unreliable when the bone quality is poor. Volar locking plates, in which the screws thread into the plate itself, are ideal for managing osteoporotic fractures [157]. Equivalent results may be obtained with external fixation. Surgeon experience is a principal determinant in the type of implant selected.
Distal Humeral Fractures
One of the most challenging fractures to treat are articular fractures of the distal humerus, particularly in the setting of osteoporosis. With rare exception, these fractures require surgery. A 1984 study demonstrated good-to-excellent results in 76 % of operatively treated fractures compared with 9 % for those treated nonoperatively [158]. These injuries require anatomic reduction and stable fixation in order to allow for early motion, as prolonged casting (>14 days) results in permanent stiffness. The advent of locked, pre-contoured plates has simplified the surgery to some extent. For the elderly, low-demand patient, primary total elbow arthroplasty may be a better alternative.
The initial evaluation should include an assessment of associated soft tissue injuries, such as an open fracture, and neurovascular status, with particular attention to the ulnar nerve which rests in close proximity to the elbow joint. Ipsilateral orthopedic injuries, such as fractures of the distal radius, are not uncommon; the entire limb should be examined and radiographed if necessary. History should include specific inquiry as to the pre-injury status of the elbow, since preexisting arthritis may influence the decision-making process. Radiographic evaluation must include AP, lateral, and oblique views of the elbow; these may be difficult to interpret because of fracture displacement and patient positioning. On occasion, traction views performed in the emergency department may provide additional detail regarding the complexity of the fracture. Virtually all patients with distal humeral fractures will require a non-contrast CT scan of the affected elbow as an element of preoperative planning. In the absence of an open fracture, these injuries are managed semi-electively in order to ensure that appropriate equipment is available.
Surgical repair of distal humeral fractures involves multiple steps; on many occasions, exposure includes ulnar nerve transposition and olecranon osteotomy for exposure. Surgery is performed under tourniquet control to limit blood loss and enhance visualization. Typical fixation includes a minimum of two plates in order to maximize stability and permit early motion. Locking plates have decreased the likelihood of failure of fixation. Nevertheless, complications are not uncommon and include ulnar nerve injury, stiffness, heterotopic ossification, and infection. Pain relief is fairly predictable, with one study reporting 83 % of patients having no or mild pain [159].
In the 1990s, dissatisfaction with the results of surgical repair of distal humeral fractures in the elderly using non-locking plates led Morrey to manage some of these injuries in a way analogous to femoral neck fractures – total elbow arthroplasty [160]. A more recent review of these patients at the Mayo Clinic showed an average range of motion of 24–132° and a high degree of patient satisfaction. The reoperation rate was 12 % [161]. Two distal humeral fracture studies comparing repair and total elbow arthroplasty in patients older than 65 years of age have come to similar conclusions [162, 163]. Elbow arthroplasty was associated with shorter surgical times, better elbow scores, less disability (as measured by DASH scores) than open reduction internal fixation. Range of motion was at least equivalent. However, given concerns about wear, the typical postoperative restrictions include lifting no more than 10 lb as a single lift or 2 lb repetitively with the affected arm. Consequently, total elbow arthroplasty is reserved for low-demand, elderly patients with preexisting arthritis or with comminuted low articular fractures with limited bone for fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree