Infiltration by lung tumor of adjacent anatomic structures including major vessels, main bronchi, and chest wall not only influences the oncologic severity of the disease but also increases the technical complexity of surgery, requiring extended resections and demanding reconstructive procedures. Completeness of resection represents in every case one of the main factors influencing the long-term outcome of patients. Technical and oncologic aspects of extended operations, including resection of Pancoast tumors and chest wall, bronchovascular sleeve resections, and en bloc resections of major thoracic vessels, are reported in this article.
Infiltration by lung tumor of adjacent anatomic structures including major vessels (pulmonary artery [PA], superior vena cava [SVC], aorta, and supra-aortic vessels), main bronchi, and chest wall not only influences the oncologic severity of the disease but also increases the technical complexity of surgery, requiring extended resections and demanding reconstructive procedures. Completeness of resection represents in every case one of the main factors influencing the long-term outcome of patients.
Although increasing experience in the last years has contributed toward improving the results of such complex operations, the diffusion of some of these interventions to multiple institutions still remains limited, due to the concern for higher perioperative complication and mortality rates.
Technical and oncologic aspects of extended operations, including resection of Pancoast tumors and the chest wall, bronchovascular sleeve resections, and en bloc resections of major thoracic vessels, are reported in this article.
Pancoast tumors
Pancoast tumor was first described in 1924 as a tumor of the apex of the lung with chest wall infiltration above the second rib and clinical signs of nerve injury such as pain, Horner syndrome, and muscle atrophy of the hand. Due to the involvement of the apex of the lung, invasion of the lower part of the brachial plexus, first ribs and vertebrae, subclavian vessels, and stellate ganglion may be present at the time of diagnosis, justifying the associated symptoms. More recently, to simplify the inclusion criteria of patients in multimodality treatment protocols a renewed definition of Pancoast tumor has been proposed, including all tumors that invade the parietal pleura or the chest wall at the level of the second rib or above, regardless the presence of neurologic symptoms ( Fig. 1 ).

These tumors may present at variable clinical stages ranging from IIB to IV, but patients amenable to surgical resection are usually limited to the T3–T4, N0–1 subgroup. Due to the particular location of the tumor and the complex anatomy of the area involved, Pancoast tumor represents a major surgical challenge, as suggested by the increased rates of incomplete resections, local recurrences, and perioperative morbidity reported in many experiences, especially in the early era of surgical treatment.
Historical Notes
The first successful surgical treatment of a superior sulcus tumor followed by postoperative radiation was reported by Chardack and MacCallum in 1956. Until that time, Pancoast tumors had been unvaryingly considered as an unresectable and incurable type of lung cancer, and definitive radiotherapy with palliative intent represented the best standard of care, although no long-term success had been reported with this therapeutic approach.
In the same year, Shaw and colleagues successfully performed a radical resection of a superior sulcus tumor in a patient previously undergoing radiotherapy with palliative intent, who presented postirradiation resolution of pain and reduction of tumor size. Based on this encouraging result, Shaw standardized this treatment strategy for the following period, observing improved local control and longer survival when compared with historical controls.
The surgical approach used consisted in an extended posterolateral thoracotomy, allowing good exposure of the posterior chest wall. As a result of the Shaw experience, the administration of induction radiotherapy followed by en bloc resection became the treatment strategy of choice for this type of tumor until the 1980s. In particular the advantages of preoperative administration of radiotherapy have been emphasized, based on the possibility to verify the marked tumor regression on the surgical specimen. The posterior incision proposed by Shaw represented the sole surgical approach used for Pancoast tumors until the early 1990s, when innovative anterior approaches were introduced that allowed for safer control of the subclavian vessels.
Although no randomized study comparing radiotherapy alone with radiotherapy plus surgical resection has been conducted, a large number of reports appeared between the 1970s and 1990s showing improved survival with the radiosurgical approach. A recent review considering 23 studies that analyze the results of radiotherapy plus surgery for Pancoast tumors has reported a mean 5-year survival rate of 36.5%. This rate was clearly higher than that (6.2%) reported in the 18 studies analyzing the results of radiotherapy alone.
Modern Multimodality Treatment Strategy
The treatment strategy for superior sulcus tumors has further changed since the late 1990s, when the introduction of trimodality regimens based on the preoperative association of chemotherapy to irradiation appeared able to produce a clear improvement of results in terms of local control and long-term prognosis. Several studies published in the last decade, reporting the use of induction chemoradiotherapy followed by surgery with radical intent, have confirmed a significant increase in complete resection rates, pathologic response rates, and long-term survival.
The largest study reporting the results of multimodality treatment for Pancoast tumors was published by the Southwestern Oncology Group (SWOG) in 2007. This trial included 110 patients with N0–1 disease undergoing an induction regimen of concurrent chemotherapy (cisplatin and etoposide) and radiotherapy (45 Gy) followed by surgery and postoperative boost of chemotherapy with the same scheme. The treatment was well tolerated, with low morbidity and mortality rates. In 88 operated patients, the complete or near complete pathologic response rate was 61% and the complete resection rate was 94%. Overall actuarial 5-year survival was 44%, and was 54% in patients showing complete response. The main limitation of this study was the heterogeneity in the surgical treatment, due to the large number of participating institutions.
In another North American study by Kwong and colleagues, the administration of a higher dose of radiotherapy in the trimodality treatment allowed favorable results even with less restrictive criteria in the selection of patients. This series included 36 patients, 14% of whom presented with N3 disease or single brain metastasis, undergoing a preoperative platinum-based chemotherapy concurrent with 45-Gy large-field radiotherapy followed by 14.2-Gy small-field boost radiotherapy. A complete pathologic response was observed in 40% of these patients, and the complete resection rate was 97%. Despite the more advanced stage of the patients, 5-year survival was 50% and was not influenced by the occurrence of brain relapses.
In a German experience published by Marra and colleagues including 31 operated patients, an aggressive multimodality treatment was used for patients with advanced stage (N2–3 disease in 29% of cases, T4 in 19% of cases). Induction regimen consisted of 3 cycles of chemotherapy with cisplatin and etoposide followed by concurrent chemoradiotherapy (one course of cisplatin/etoposide plus 45 Gy hyperfractionated accelerated irradiation). This unique multimodality approach resulted in a high complete or near complete response rate (69%) with radical (R0) resection achieved in all patients. Overall 5-year survival was 46%, with significantly better results in patients showing response to induction therapy and with N0–1 disease. A 6.4% postoperative mortality was reported.
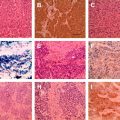
A high pathologic response rate has been also reported in a recent large series (72 patients) published by Pourel and colleagues, with a less aggressive induction chemoradiotherapy regimen (cisplatin and etoposide plus 45 Gy radiotherapy). In this study the tumoral tissue was found to be completely replaced by necrosis and desmoplastic fibrosis induced by the preoperative treatment in 39.5% of patients. The reported 5-year survival reached 51% with a 98% complete resection rate.
Similar pathologic response rate was achieved in a study of the Japanese Clinical Oncology Group, with a 5-year survival rate of 56% despite the inclusion of N2 patients. Results of the main trimodality treatment series are reported in Table 1 . Improvements in survival obtained with trimodality treatment are principally explained by the decrease of local recurrences. The incidence of recurrent disease at thoracic level has been observed as less than 30% after trimodality regimens, in comparison with 70% and more after radiotherapy and chemotherapy alone, and 40% with concurrent chemoradiotherapy alone.
| Authors, Year | No. of Operated Patients | Stage | Inclusion/Exclusion Criteria | Treatment | Complete Resection (%) | Pathologic Complete Response (%) | 5-Year Survival (%) | Median Survival (mo) |
|---|---|---|---|---|---|---|---|---|
| Kwong et al, 2005 | 36 | IIB–IV | N2, M1 incl. | CT/RT (59.2 Gy) + S | 97 | 40 | 50 | 31 |
| Marra et al, 2007 | 31 | IIB–IIIB | N2–3 incl. | CT+ CT/RT (45 Gy) + S | 100 | 69 | 46 | 54 |
| Rusch et al, 2007 | 88 | IIB–IIIB | N0–1 only | CT/RT (45 Gy) + S + CT | 94 | 61 | 44 | NR |
| Kunitoh et al, 2008 | 57 | IIB–IIIB | N2 incl. | CT/RT (45 Gy) + S | 68 | 21 | 56 | NR |
| Pourel et al, 2008 | 72 | IIB–IIIB | N2 incl. | CT/RT (45 Gy) + S | 98 | NR | 51 (3 y) | 36.5 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree