Highlights
- •
The 10%-rule effectively identified metastatic sentinel nodes intraoperatively.
- •
Applying the 10%-rule per neck side must be considered.
- •
Raising the threshold is not advised, as this leads to missed metastatic nodes.
- •
More research on radioactivity in false-negative sentinel node procedures is needed.
Abstract
Background
Sentinel lymph node biopsy (SLNB) has proven to reliably stage the clinically negative neck in early-stage oral squamous cell carcinoma (OSCC). The 10%-rule, used to define sentinel lymph nodes (SLN) intraoperatively, states that an SLN is defined by gamma counts that are at least 10% of the hottest harvested lymph node (LN). However, this intraoperative rule has not yet been adequately evaluated for early-stage OSCC. This study aims to evaluate the 10%-rule intraoperatively and explore possibilities for redefining this criterion.
Methods
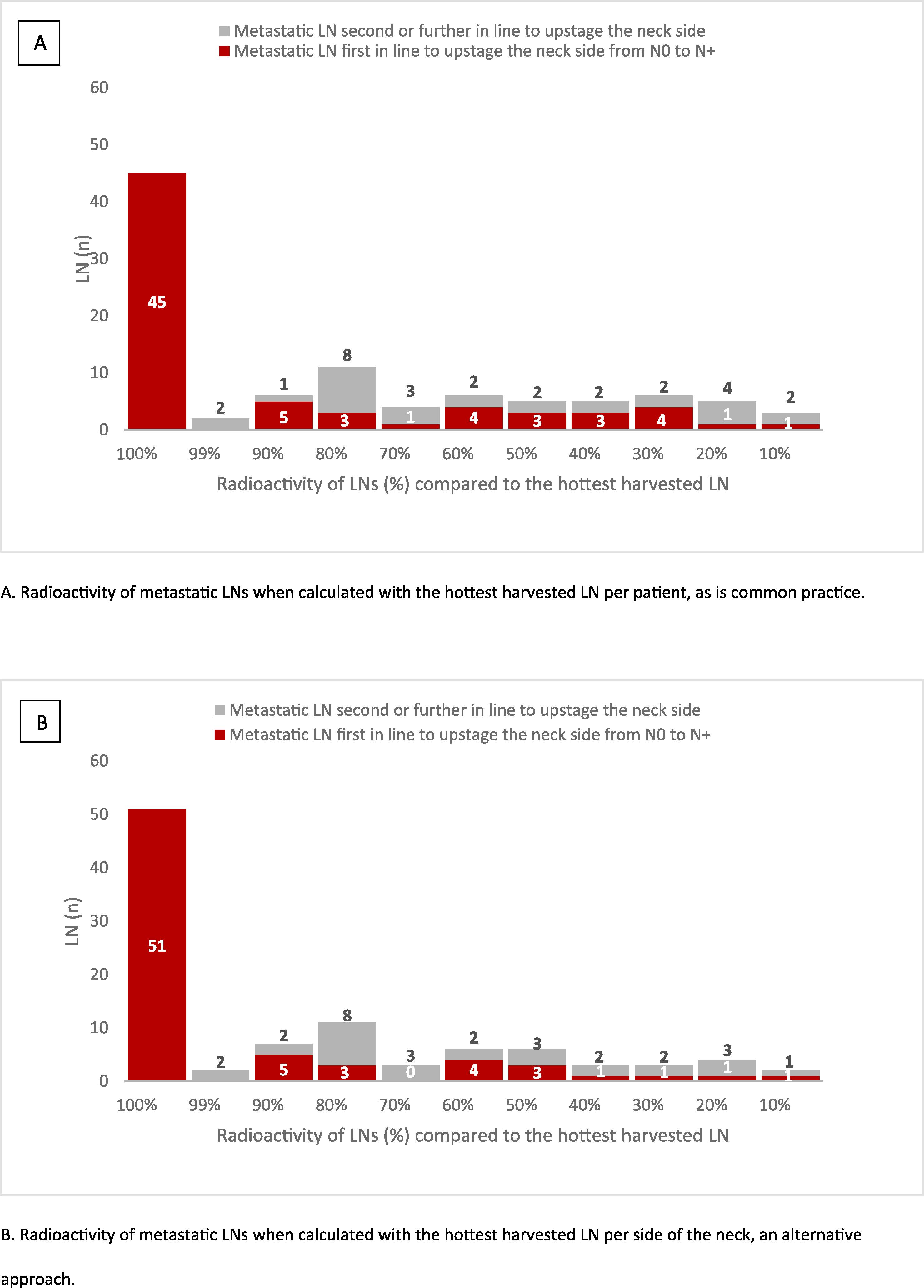
A single center retrospective study was performed between 2014 and 2023. Patients (n = 66) with clinically node-negative OSCC (cT1-3N0) and positive SLNB were included in this study. Radioactivity of all harvested LNs were measured ex-vivo. Metastatic LNs were assessed for complying with the 10 %-rule. The accuracy of alternative thresholds was evaluated. If multiple positive SLNs on one side of the neck were found, the hottest positive SLN on that side was considered the LN accountable for upstaging the corresponding neck side from N0 to N+.
Results
A total of 233 LNs were harvested, of which 98 contained metastases and 190 met the 10%-rule. Of these metastatic LNs, 70 were accountable for upstaging the side of the neck. The 10%-rule correctly staged 69 of 70 metastatic sides of the neck. By increasing the intraoperative cut-off point to 20%, 68 of 70 metastatic sides of the neck were correctly staged and 18 LNs (172 vs. 190) were not defined as SLN. Applying the 10%-rule to each side of the neck increased detection of one metastatic LN. However, this LN was not accountable for upstaging that side of the neck.
Conclusion
The 10%-rule in SLNB applies to patients with OSCC and effectively identifies metastatic SLNs intraoperatively. Applying the 10%-rule per neck side must be considered. Increasing the threshold percentage is not advisable.
Introduction
To establish an accurate treatment plan for patients with early-stage oral squamous cell carcinoma (OSCC), it is crucial to confirm the presence of cervical metastasis. The sentinel lymph node biopsy (SLNB) has proven to be a reliable procedure for detecting occult cervical metastases in early-stage OSCC and, thus, for staging the clinically negative neck .
The routine SLNB procedure starts with preoperative peritumoral injection of a 99m-technetium ( 99m Tc)-labeled radiotracer followed by lymphoscintigraphy using planar images and single photon emission computed tomography/computed tomography (SPECT-CT). Subsequently, nodal hot spots detected on SPECT/CT are designated by a nuclear physician as SLN or higher echelon node (HEN) .
Nodal hot spots marked as sentinel lymph nodes (SLNs) require surgical extirpation and subsequent histopathological analysis for the presence of occult metastasis. In general, the marked SLNs are localized during surgery through gamma-tracing using a handheld gamma probe . To define radioactive nodes detected through gamma-tracing intraoperatively as either relevant SLN or irrelevant HEN, the 10 %-rule is often used. The 10 %-rule states that an SLN is defined by gamma counts that are at least 10 times that of background and more than 10 % of the hottest harvested lymph node (LN) as measured ex-vivo . This criterion is originally adapted from the procedure in breast cancer patients . However, the 10 %-rule has not yet been adequately evaluated in OSCC and is under scrutiny due to potential excessive LN removal . In this study, we aim to evaluate the 10 %-rule for SLNB in patients with clinically node-negative OSCC and to explore possibilities for redefining the criteria for identifying SLNs during surgery.
Material and methods
Patients
A single center retrospective study was performed between December 2014 and May 2023 at the University Medical Center Utrecht, the Netherlands. The study was approved by the Ethics Committee of the University Medical Center Utrecht (no. 19-676) and conducted in compliance with the Declaration of Helsinki. Informed consent regarding the use of clinical, radiological and pathological data was waived by the Institutional Review board due to the retrospective nature of the conducted study.
Patients with clinically node-negative OSCC (cT1-3 N0, T3 only when assessed based on tumor dimensions of >2 cm and ≤4 cm with DOI >10 mm. Based on TNM Staging American Joint Committee on Cancer Union for International Cancer Control 8th Edition ) and positive SLNB were included in this study. SLNB was defined as positive when isolated tumor cells (ICTs, ≤0.2 mm), micrometastasis (>0.2 mm and <2 mm), or macrometastasis (≥2 mm) were found in one or more harvested SLNs. Clinical N0 staging was confirmed by palpation of the neck, ultrasound-guided fine needle aspiration cytology (US-FNAC), and, on indication, by magnetic resonance imaging (MRI).
Patients were excluded if radioactive emissions of harvested SLNs, as measured ex-vivo during surgery, had not been documented, the patient had recurrent primary OSCC (<5 years), a second primary squamous cell carcinoma in the head and neck region, or previous treatment of the neck.
Sentinel lymph node biopsy
The SLNB procedure in our institution was performed according to international guidelines . All patients underwent lymphoscintigraphy (LSG) using dynamic, planar static, and single photon computed tomography and CT (SPECT-CT) on the day of surgery (single-day protocol) or the day before surgery (two-day protocol). Patients received 2–4 peritumoral injections of a 99m Tc-labeled radiotracer (i.e. nanocolloid, tilmanocept). In some cases the 99m Tc-labeled radiotracer was bound to indocyanine green (ICG), administered as hybrid tracer, as described by KleinJan et al. . Based on LSG and SPECT-CT, nodal hot spots were designated by a nuclear physician as SLN(s) or HEN(s). The position of the SLNs were marked on the overlying skin using a Co-57 pen point marker and a (handheld) gamma camera . Intraoperatively, nodal hot spots were explored with a handheld gamma probe and, when ICG was used, a near infrared camera (PDE NEO II near-infrared camera; Hamamatsu, Herrsching, Germany). Radioactive emissions of harvested SLNs were quantified ex-vivo by a conventional handheld gamma probe (Europrobe; Eurorad S.A., Eckbolsheim, France). The highest counts observed over a 10-second period was recorded as radioactivity of the SLN in counts per second. Nodal hot spots were explored intraoperatively until the radioactivity in this nodal basin was less than 10 % compared to the radioactivity of the hottest harvested LN, or no residual radioactive LN could be found. Depending on the surgeon’s preference, intraoperative SLNB was performed either before or after tumor resection. Histopathological examination of the harvested SLN was performed through step serial sectioning on 5 levels with 200 µm distance between each level, hematoxylin-eosin (HE) staining, and immunohistochemistry (keratin AE1/3) if no metastasis was detected on the HE-stained slide .
Sentinel lymph nodes accountable for upstaging the corresponding side of the neck from N0 to N+
SLNB was used to determine the necessity for subsequent neck treatment (i.e. neck dissection, radiotherapy) if (occult) neck metastases were identified through this procedure. Only one metastatic SLN located at one side of the neck is needed to upstage the corresponding side of the neck from N0 to N+. Therefore, if, by SLNB, more than one SLN on a single side of the neck was found to contain metastases, the metastatic SLN with the highest radioactivity and, consequently, the highest counts as measured with the handheld gamma probe ex-vivo, was considered the SLN first in line to upstage the corresponding side of the neck from N0 to N+. These SLNs, as well as any LN that was the only metastatic LN on one side of the neck, are referred to as ‘SLN accountable for upstaging the (corresponding) side of the neck from N0 to N+’ or ‘SLN first in line to upstage the (corresponding) side of the neck from N0 to N+’.
Statistical analysis
Professional statistical software (IBM SPSS Statistics Version 29.0.1) was used to analyze all data. Radioactivity of all harvested LNs were analyzed. Additionally, for each patient all harvested LNs were assessed from highest to lowest radioactivity to analyze the rank of metastatic LNs. Metastatic LNs were also assessed for complying with the 10 %-rule. Alternative thresholds (e.g. 15 % or 20 %) were analyzed to determine the number of (metastatic) LNs harvested (classified as ‘hot LNs’, ‘metastatic SLNs’ or ‘SLNs accountable for upstaging the side of the neck’) and missed or additionally detected in comparison to the 10 %-rule (defined as ‘missed (−) or additionally (+) detected metastatic SLNs’). The number of LNs complying with the newly evaluated threshold was compared with the number of LNs complying with the 10 %-rule, defined as ‘reduced (−) or additional (+) LNs’. This analysis was conducted using the hottest harvested LN per patient as a reference, as is standard in clinical practice, to calculate the relative radioactivity of other harvested LNs without differentiating between sides of the neck. Additionally, we explored an alternative approach, analyzing different thresholds, using the hottest LN on each side of the neck as a reference to calculate the relative radioactivity of LNs on the corresponding side. All categorical data are presented as numbers (n) and corresponding percentages (%). Data for parametric continuous variables are presented as mean, and as for nonparametric continuous variables as median.
Results
A total of 66 patients with at least one metastatic SLN were included in this study, 34 males and 32 females, with a mean age of 63 years (range 28–85) at the time of operation. In the majority of the cases, the tumor was located on the tongue (46 of 66 patients), followed by floor of mouth (12 of 66 patients). Most of the patients, 46 of 66, were diagnosed with a cT2 OSCC. SLNB revealed pN1(sn) in most cases (32 of 66 patients). Yet, 7 out of 66 patients had pN3b(sn) due to extranodal extension of metastasis in the SLN. Patients and tumor characteristics are shown in Table 1 .
| Total | ||
|---|---|---|
| Patients, n | 66 | |
| Sex, n (%) | ||
| Male | 34 | (49.4) |
| Female | 32 | (50.6) |
| Mean age (range) | 63 | (28–85) |
| Tumor location, n (%) | ||
| Tongue | 46 | (69.7) |
| Floor of mouth | 12 | (18.2) |
| Buccal mucosa | 3 | (4.5) |
| Retromolar trigone | 3 | (4.5) |
| Lower jaw | 2 | (3.0) |
| Tumor side, n (%) | ||
| Lateralized | 62 | (94.0) |
| Median | 3 | (4.5) |
| Paramedian | 1 | (1.5) |
| cT, n (%) | ||
| 1 | 25 | (37.9) |
| 2 | 36 | (54.5) |
| 3 | 5 | (7.6) |
| pN(sn), n (%) | ||
| i+ | 4 | (6.1) |
| 1 | 32 | (48.5) |
| 2a | 1 | (1.5) |
| 2b | 16 | (24.2) |
| 2c | 6 | (9.1) |
| 3b | 7 | (10.6) |
| pT, n (%) | ||
| 1 | 20 | (30.3) |
| 2 | 33 | (50.0) |
| 3 | 10 | (15.2) |
| 4a | 3 | (4.5) |
Results of applying the 10 %-rule intraoperatively
In 66 patients, a total of 233 LNs were harvested, with a median of three LNs per patient (range 1–10) and a median of two nodal basins explored per patient (range 1–5). In seven patients only one SLN was identified (10.6 %). Most metastases were found in level II on the ipsilateral side of the lateralized tumor. Out of all harvested LNs, 98 contained metastasis of which 70 (71 %) were accountable for upstaging the corresponding side of the neck from N0 to N+. Out of those 70 LNs, 69 met the 10 %-rule. Therefore, one metastatic LN that was accountable for upstaging the corresponding side of the neck did not comply with the 10 %-rule. This hottest metastatic LN contained 5 % of the radioactivity compared to the hottest harvested LN (located on the same side of the neck) and was the only metastatic LN located on the ipsilateral side of the tumor. In this patient, four other LNs were harvested on the ipsilateral side, none of which harbored metastasis. This patient also had a contralateral metastatic SLN which contained 26 % of the radioactivity compared to the hottest harvested (ipsilateral) LN.
A median of one metastatic LN was found per patient (range 1–3). Radioactivity with an interval of 10 % of all metastatic LNs is shown in Fig. 1 . Among these metastatic LNs, 45 were the hottest harvested LN per patient ( Fig. 1 A). Applying the 10 %-rule per side of the neck resulted in 51 metastatic LNs classified as hottest harvested LN ( Fig. 1 B).