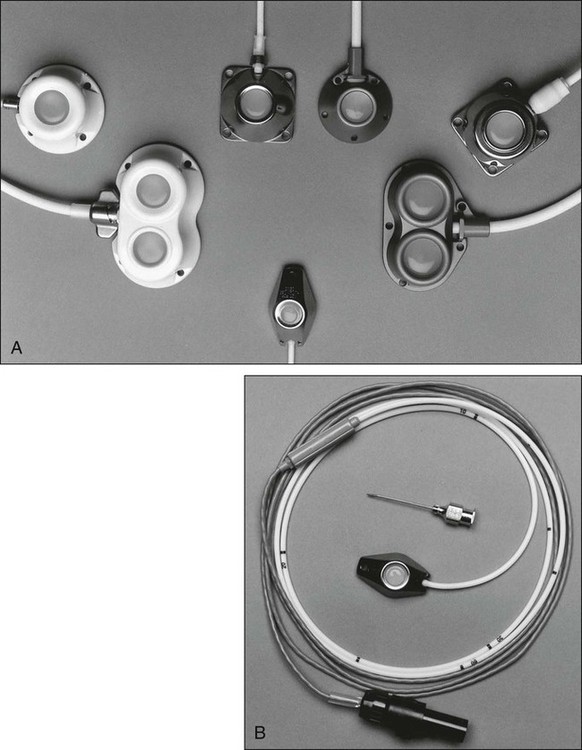
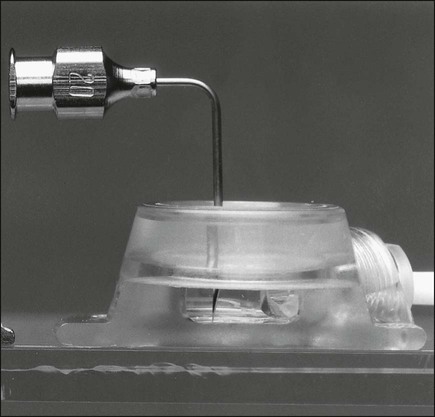
John C. Mansour and John E. Niederhuber • Three questions to ask when selecting a catheter system are: (1) Which device best meets the patient’s therapy and lifestyle needs? (2) How is the device most safely inserted and maintained? (3) What are the potential immediate and long-term complication risks? • Types of central access systems are the traditional central line for short-term use, tunneled central lines for long-term use, surgically implanted infusion ports, and peripherally inserted central catheters. • Vascular access devices can be placed using a number of anatomic sites to access the superior vena cava or inferior vena cava: the subclavian vein, internal jugular vein, external jugular vein, and femoral vein. • Insertion can be performed via the Seldinger (closed) technique or by operative exposure of the vein (open technique). • Short-term complications include vascular laceration, arterial puncture, pneumothorax (2%), hemothorax, and air embolus (overall placement complications should be <5%). • Long-term complications include catheter exit site or tract infection, catheter-associated sepsis, cardiac arrhythmias, catheter colonization, catheter thrombus (~30%), fibrin sheath, extravasation, occluded catheter, and shearing of the catheter. • Factors increasing the risk of catheter-associated infection include prolonged duration of indwelling time, multiple-lumen catheters, femoral locations, non–catheter-related bacteremia (in a neutropenic patient), the number of times the system is accessed, difficult catheter placement, and poor technique in catheter or port-site care. Most patients with cancer need a long-term form of central venous access rather than a traditional short-term central line. Surgically tunneled central lines were developed to increase the distance between the skin entrance site and the puncture of the vein. The hypothesis was that by increasing this distance, the life span of the central access would be increased by decreasing the incidence of infection and thrombosis. Tunneled central lines are commonly referred to by the name of the first brand that was marketed—Hickman. Other examples include Broviac, Quinton, and Groshong (Fig. 26-1). These polymeric silicone rubber venous access catheters are placed via a subcutaneous tunnel that is described in detail later in this chapter. Clinical studies have supported the hypothesis that increasing the distance between the catheter exit site in the skin and the hole in the vein decreases the incidence of externally derived infection.1,2 Studies suggest that the incidence of bloodstream infections associated with tunneled catheters is approximately 1 to 2 per 1000 catheter days.3 The frequency of bacteremia among nontunneled catheters has been reported at between 1.0 and 13.0 per 1000 catheter days.6–6 Implantable ports consist of a small injection reservoir with a self-sealing membrane placed entirely beneath the skin. There is no external catheter. An internal catheter runs from the reservoir into the subclavian or internal jugular vein to provide central access. The internal catheter is essentially identical to those used for tunneled central lines. A noncoring (Huber) needle can pass directly through the skin into the reservoir for infusion or aspiration. The self-sealing rubber cap on the reservoir prevents leakage from the reservoir after withdrawal of the Huber needle. The gauge of the noncoring needle—not the catheter—typically limits flow through the port system (Fig. 26-2). The ports can also be used for continuous drug infusion, as shown in Figure 26-3. The theoretical concern that bacteria more easily traverse the short distance between the skin and the “neo-vein” or reservoir and cause increased rates of infection does not prove true.7 Sterile technique and site care lead to an infection risk comparable with that of tunneled catheters. With adequate care, the rate of infection could be fourfold to fivefold less than that for tunneled catheters.3 The low rate of infection and extravasation make infusion ports ideally suited for patients with cancer who need long-term single-lumen access and a low-maintenance catheter. However, experience has shown that patients with prolonged periods of neutropenia or significant risk of cutaneous eruptions might not be good candidates for port devices. The visible lump of the port could bother extremely thin patients; however, the port on the anterior chest wall is easily hidden from plain view for most people. Also known as a peripherally inserted central catheter (PICC line), the long-line central access vascular access device is becoming increasingly popular. The catheter is inserted into a brachial, cephalic, or antecubital vein and advanced into the subclavian vein or higher. These lines can be placed simply and easily in the outpatient office setting and are well tolerated by patients, with minimal risk. However, many patients with cancer have poor-quality arm veins after undergoing multiple peripheral infusions and are therefore poor candidates for this technique. The 50% risk of catheter-related thrombosis is the greatest drawback to more widespread use of PICC lines in patients with cancer. This problem is a result of the presence of a long length of catheter within the vein and to the catheter tip in the relatively low-flow subclavian vein. Advancing the catheter tip into the SVC can reduce the incidence of thrombosis by more than half.8 Accurate placement of the catheter tip in the SVC can be complicated by the large displacement of the catheter tip (up to 8 cm) with normal arm range of motion.9 Providing patients who are undergoing treatment for cancer with appropriate vascular access requires not only a thorough knowledge of available devices but also technical expertise in the procedures for placing these catheters. Although these procedures are sometimes viewed as routine, the risks of poor technique can be devastating for the patient. Before undertaking the procedure, the physician should carefully consider everything from the site of insertion to the dressing to be used at the end of the procedure (Table 26-1). Table 26-1 General Guidelines for Catheter and Port Use The most frequent site for insertion of vascular access devices in the oncology population is the subclavian vein. Clavicular fracture or a previous median sternotomy can alter the anatomy of this location. For a patient with such a history, an alternative site should be considered. Even for patients with standard venous anatomy, the acute angle at the confluence of the subclavian and internal jugular veins at the brachiocephalic vein can complicate the passing of the guide wire into the SVC. A higher incidence of pneumothorax, hemothorax, and catheter malposition occurs among inexperienced operators, and a higher incidence of vein stenosis occurs with subclavian vein placement than with internal jugular placement.10 A subclavian artery puncture during line placement can be difficult to control because of the position of the artery posterior to the clavicle. A catheter placed on the anterior chest wall is more comfortable and easier to cover with clothing, however, than is a line in the neck. Studies suggest that providing a single dose of prophylactic antibiotic to cover common skin flora before inserting the vascular access device reduces central line infection. However, it is difficult to determine how this small benefit affects antibiotic resistance and subsequent infections. Use of central venous catheters impregnated with antibiotics could be more effective in dealing with infectious complications and will be discussed later in this chapter.11 A sterile surgical field with mask, gown, cap, gloves, and a large sterile drape should be used to minimize the risk of line infection.12 The skin of the entire anterior neck and chest should be prepared with chlorhexidine, which is superior to povidone-iodine or alcohol in limiting line infections.13,14 The choice to use ultrasound guidance to identify the vein during cannulation should be addressed before beginning the procedure. Less-experienced operators will likely benefit from the use of ultrasound guidance as an adjunct to the anatomic landmarks technique.15,16 Ultrasound can decrease the incidence of arterial puncture and placement failure. Although a few reports exist in the literature regarding the advantage of these techniques, such superiority is often judged when compared with high rates of complications using the landmark approach as the control group. The operator must also decide where to position the catheter tip within the central vein. Catheters positioned with the tip in the right atrium will function longer as a source for aspirating blood samples than will those with the tip positioned in the SVC.17,18 A case review of thrombosed catheters documents that the position of the tip of the catheter at the time of thrombosis seems to be the most important contributing factor.19,20
Establishing and Maintaining Vascular Access
Choosing the Right Device
Surgically Tunneled Central Lines
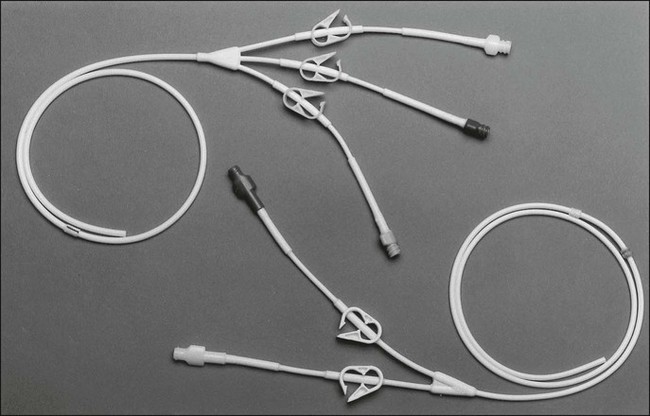
Surgically Implanted Infusion Ports
Long-Line Central Access
Inserting Vascular Access Devices
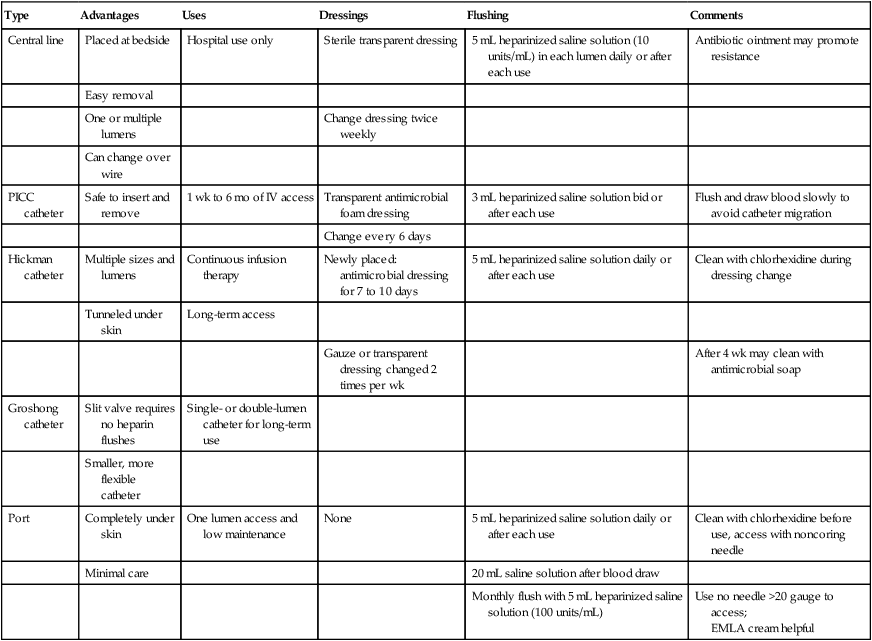
Type
Advantages
Uses
Dressings
Flushing
Comments
Central line
Placed at bedside
Hospital use only
Sterile transparent dressing
5 mL heparinized saline solution (10 units/mL) in each lumen daily or after each use
Antibiotic ointment may promote resistance
Easy removal
One or multiple lumens
Change dressing twice weekly
Can change over wire
PICC catheter
Safe to insert and remove
1 wk to 6 mo of IV access
Transparent antimicrobial foam dressing
3 mL heparinized saline solution bid or after each use
Flush and draw blood slowly to avoid catheter migration
Change every 6 days
Hickman catheter
Multiple sizes and lumens
Continuous infusion therapy
Newly placed: antimicrobial dressing for 7 to 10 days
5 mL heparinized saline solution daily or after each use
Clean with chlorhexidine during dressing change
Tunneled under skin
Long-term access
Gauze or transparent dressing changed 2 times per wk
After 4 wk may clean with antimicrobial soap
Groshong catheter
Slit valve requires no heparin flushes
Single- or double-lumen catheter for long-term use
Smaller, more flexible catheter
Port
Completely under skin
One lumen access and low maintenance
None
5 mL heparinized saline solution daily or after each use
Clean with chlorhexidine before use, access with noncoring needle
Minimal care
20 mL saline solution after blood draw
Monthly flush with 5 mL heparinized saline solution (100 units/mL)
Use no needle >20 gauge to access;
EMLA cream helpful
Choosing Insertion Location
Preparing to Place the Vascular Access Device
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Establishing and Maintaining Vascular Access