Mexico; in Europe, some disease with the same characteristics of this disease occurred in the middle of this century; in some developed countries, such as the United States, Britain, France, and Japan, there were some sporadic cases. In China, a large-scale epidemic occurred in the southern region of Xinjiang province between 1986 and 1988, and its prevalence intensity and involvement of areas and duration were the largest worldwide to date[3]. In September 1986, this epidemic started from Luopu County in Hetian prefecture. At that time, there was no specific laboratory diagnostic method, except for serological methods of exclusion tests that ere used to establish the diagnosis of non-A and non-B hepatitis in combination of the findings of enteric transmission and epidemiological studies. However, because there were no effective preventive measures, the number of cases rapidly increased, leading to continuous epidemic progresson and a large-scale epidemic involving three prefectures (states), 23 counties and cities that lasted for 20 months. In addition, small-scale epidemics occurred in Liaoning, Jilin, Hebei, Shandong, Inner Mongolia and other provinces or autonomous regions, mostly sporadic cases.
and clinical observations were conducted on families with and without the disease [5]. In the investigated population, the ratio of clinical infection to sub-clinical infection was 1:2.56, but, for children younger than 9 years old, this ratios was 1:13. Clinicaltype cases were mainly confined to young adults, but the infection of hepatitis E in children had no difference from that in adults but was mainly of the sub-clinical type. The infection rate of sub-clinical type in families with the incidence of this disease was higher than families without the incidence (Table 8.2, Table 8.3 ). This indicated that affected children were more susceptible to hepatitis E with the subclinical type, but their attack rate of the clinical type was significantly lower than the rate of adults.
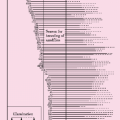
Table 8.1 Prevalent rates of major symptoms and signs in cases with acute hepatitis E* | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 8.2 Age distribution of infection frequency of hepatitis E in different groups* | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
incidence were collected. Using immunoelectronic microscopy method to examine the virus particles, we investigated the role of virus particle excreted in the stools of patients (Table 8.4 ) [6]. The duration of excretion of virus particles varied from 3 to 12 days among all cases. There were 17 of 60 specimens (28.3%) showing positive results in the excretion of virus particles. The peak of virus discharge was between 1 – 4 days before the onset of the disease and one week after the onset of the disease. Subsequently, positive detection rates decreased along with the disease incidence course, and there were no virus particles discharged two weeks after the onset of the disease. Based on these facts, the infectious phase of this disease was between the end of latency phase and two weeks after the onset of this disease, and the isolation phase was defined from the onset date to 2-3 weeks after the onset of this disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree