Outline
The so called “Qapqal Disease” is botulism caused by botulinum, an epidemic for many years in Qapqal Autonomous county of Xinjiang province, China. However, the incidence of this disease has been limited in the Xibo Nationality, and the disease is characteristerized by a strict seasonal feature and a specific regional distribution but a relatively high mortality rate with unknown pathogens and epidemic factors. In 1958, through a series of epidemiological investigations, it was found that this disease was related to taking or tasting “Misonghuhu” (a semi-finished product of flour paste made out of wheats), which was further confirmed by bacteriological tests and animal experiments with “Misonghuhu”. These investigations vividly demonstrated the significance of using the right investigation methods and explorative field observations to identify the etiology of an unknown disease in an outbreak of epidemic.
There had been a lethal disease that occurred many years ago without a confirmed diagnosis in the ethnic minority groups in Qapqal Xibe Autonomous County of Xinjiang Province, China. Because this disease usually occurred in spring-ploughing seasons, it had a serious impact on local agriculture and livestock farming production. It had been asserted that this disease only occurred in the Xibe ethnic minority group, and the population of the Xibe ethnic minority was only about 8, 800 in 1958. Therefore, this disease with an unknown origin led to a panic among local ethinic-minotiry officials and residents. In April 1958, we started to conduct a field investigation there to identify the etiology that may help put the epidemic under control.
1. Qapqal Xibe Autonomous County belongs to Yili Kazak Autonomous Prefecture, and it is located in the west border of Xinjiang province and has an adjoining boundary to the Soviet Union. It is large geographically but sparsely populated by multi-ethnic minority groups, among which the population of Uygur was the most populated, followed by Kazak and Xibe ethnic minority groups. The remaining ethnic minority groups were quite few. Uygur and Kazak people earned their living mainly on livestock farming, while Xibe people earned their living on both agriculture and livestock farming, but many residents were state employees at that time. The Yili horse raised in the farm in its next county was a famous horse nationwide. The Xibe people were considered the descendants of Man ethnic minority who were sent to defend the borders in Xinjiang province 193 years ago (counted back from 1958). Populated at two districts in Qapqal county, Xibe people were not living in any other places. They had the same living habits by breeding pigs, cows and chickens and sleeping on the hypocaust as those of people living in Northeast China.
Local officials and residents called this epidemic disease as “Qapqal Disease”, “New Disease” (not seen before 1949) or “Encephalitis” and knew that it had an onset only in the spring. We had not seen the first case in the very year we had arrived until we went to and stayed in the field for one month. Through searching and reading hospital records of previous years, examining more than ten people with a past history of this disease, discussing with medical workers and referring to survey responses from patient family members and other residents, we had some impressions of this disease, which included diplopia, dizziness, mild headache, blurring of vision, difficulties or even disability in lifting head and eyelids, coarse voice and difficulties in swallowing. It was asserted that the patients had no fever or irregular low fever, and the disease conditions were various in the levels. Some cases could be cured through treatment, but some cases remained mild blurring of vision or difficult in lifting head. Severe cases even died in two or three days since the onset of the disease but they still had a clear consciousness before dying.
Before arriving at the field, we had considered several possibilities including botulism or other poisoning diseases, forest encephalitis, tick-borne paralysis, viral nervous system diseases and myasthenia gravis.
Each country in Qapqal county was a big village with relatively centralized inhabitants. We went to visit several countries and observed terrain and terrain features. There were all big pasture lands with small hill areas that were located at least 40 kilometers away from forests. Medical insect professionals conducted investigations of ticks, mites and mosquitos on animals, inside the living rooms and outdoors. According to clinical features and primary epidemiological data of this disease, tick-borne paralysis, forest encephalitis and other viral nervous system diseases were excluded easily. In addition, myasthenia gravis was also basically excluded.
2. It was suggested from indirectly acquired clinical data that it partly complied with botulism. However, we were quite confused by several questionable pieces of evidence and some contradiction in following primary information:
a) There was always only one case occurred in a family;
b) The onset was always only in spring, because it was never recorded in the literature that botulism had such a seasonal feature.
c) There was no evidence that suspicious food or food products may have possibly lead to botulism that had never been found in the families with the disease over the years.
d) The mortality rate seemed not to be in accordance with botulism, since it was generally regarded that over 80% cases with botulism would die.
Until the investigation in 1958, it had never been reported of any cases with confirmed botulism in China. Therefore, epidemiological investigation would focus on the distribution characteristics of and suspicious food (or other possible causes) leading to this disease. Meanwhile the epidemiological investigation analyzes all possible causes that may help distinguish botulism from other poisoning diseases similar to botulism.
Natural history of the disease: we collected clinical and epidemiological data from door to door in about 2/3 families in the No. 6 country with the most incident cases of this disease and encouraged
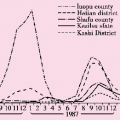
people to recall all incidence and mortality histories of this disease in the past nine years since 1949. Having discussed with local senior medical workers and officials of special prefectures, counties and countries, we understood that there had been some incidence and mortality of this disease during the regime of the old governance before 1949, and this disease was sometimes called “infectious disease”. In epidemic seasons of this disease, soldiers had even been dispatched to guard river banks of Yili to prohibit Xibe people to come cross the river to Yili (the original Yili City was named as Yining City later). Therefore, this was not a new disease. According to incomplete statistics, 38 out of a total of 88 cases with this disease had died, and the mortality rate was 43.2%. Between 1949 and 1957, “Qapqal Disease” occurred each year (see Table 2.1 ), and in 1949, 1953 and 1955, the disease occurred relatively frequently. In one year with the highest disease incidence, the number of cases was as high as 24, and in one year with the highest mortality, the number of deaths was 13. However, these were inaccurate figures, because there was no local disease registration system by then.
people to recall all incidence and mortality histories of this disease in the past nine years since 1949. Having discussed with local senior medical workers and officials of special prefectures, counties and countries, we understood that there had been some incidence and mortality of this disease during the regime of the old governance before 1949, and this disease was sometimes called “infectious disease”. In epidemic seasons of this disease, soldiers had even been dispatched to guard river banks of Yili to prohibit Xibe people to come cross the river to Yili (the original Yili City was named as Yining City later). Therefore, this was not a new disease. According to incomplete statistics, 38 out of a total of 88 cases with this disease had died, and the mortality rate was 43.2%. Between 1949 and 1957, “Qapqal Disease” occurred each year (see Table 2.1 ), and in 1949, 1953 and 1955, the disease occurred relatively frequently. In one year with the highest disease incidence, the number of cases was as high as 24, and in one year with the highest mortality, the number of deaths was 13. However, these were inaccurate figures, because there was no local disease registration system by then.
Table 2.1 The situation of morbidity and mortality of “Qapqal Disease” over the years (based on incomplete statistics) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree