that chickens would suffer from goiter after drinking shallow-well water added with potassium iodide at the iodide level of the deep-well water. Experiments in Kunming mice further showed that the weight of the thyroid in mice and the proportion of mice with goiter increased with their iodine intake of varied doses of iodine. All these findings concluded that endemic goiter in this area was consistently associated with chronic exposure to excessive iodine in its drinking water.
an annual precipitation of 560 millimeters concentrated in three months from July to September with pelting and violent rain. There is little plant coverage on its hilly top. The slope of the land is steep there, with a thin layer of the surface less than 1.4 meters of thickness composed of a mixture of sand and loam and a mixture of sand and pebble below the surface. So, iodine deficiency environment is formed there because of the following geographic features: (1) the airflow containing more iodine from the sea and ocean is blocked by the Yanshan Mountain so that little iodine is present in the rain, (2) iodine in the soil is easy to be washed away due to heavy rain in the three months and the steep slope of the land, and (3) iodine can not be adhered and deposited due to its big granule and larger holes in the soil.
Table 5.1 Comparison of iodine concentrations in the water, soil, grains and vegetables between Chengde City and Shijiazhuang City | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
quota of 14 kilograms (kg) and subsidiary food included pakchoi, pickle and wild vegetables. Protein intake of the labor force was about 80 grams (g) daily per person, which was all from plant sources. Intake of fat, carbohydrate and gross calorie were 30 g, 670 g and 13681.68 kilojoule (kJ), respectively. Vitamin B2 deficiency was common in the pupils of primary schools, and 10% of them had obvious symptoms of vitamin A deficiency. Nutritional investigation and analysis of iodine contents in staple food and vegetables showed that intake of iodine was 35.95 μg per day per person for the residents living in the suburb of Chengde City, about 23.97% of the recommended daily intake. All these conditions mentioned above led to a high prevalence of endemic goiter and cretinism in that area.
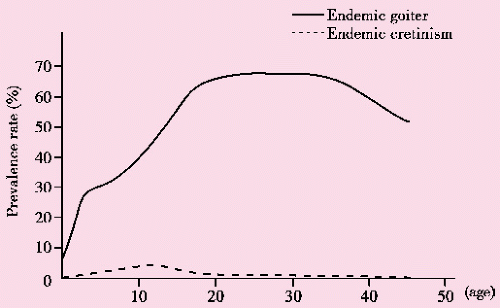
Endemic cretinism was found among all age-groups except for the 0-year group, and the peak of occurrence of the cases was in 7-year and 12-year age-groups, accounting for 81.58% (62/76) of the total cases, with an age-specific prevalence of 7.94% for 7-year and 12-year groups. All these children were born during the periods of Chinese civil war (1945-1949) and the Korean War (1950-1953). It was suggested that endemic cretinism could be related with multiple factors other than iodine deficiency, e.g., severe malnutrition and psychological trauma during pregnancy caused by wars. The distribution of endemic cretinism varied in the four villages, the highest (2.87%) in Erdaohe Village, followed by 2.40% in Lamasi Village and 1.89% in Luohantang and Shiziyuan Villages. It is worthy noting that with the same living standard and cultural background, the prevalence of endemic cretinism was lower in Luohantang and Shiziyuan Villages, a valley area with inconvenient transportation, compared with Lamasi and Erdaohe Villages that lied on the bank of a river with better transportation. Therefore, it is suggested that there existed some factors other than iodine deficiency for the occurrence of endemic cretinism.
Table 5.2 Prevalence of endemic goiter and cretinism in Chengde suburb in 1962 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 5.3 Comparison of prevalence of thyroid swelling between iodine supplementation and control groups[5] | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||
Table 5.4 Impact of iodine supplementation on the prevalence of goiter | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
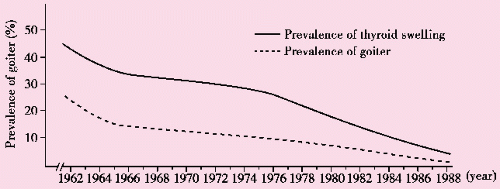
Table 5.5 Prevalences of thyroid swelling in four villages and the suburb of Chengde City in 1962-1988[6] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 5.6 Clinical types of endemic goiter in the suburb of Chengde during 1962 to 1988[6] | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
goiter reduced with age, with a coefficient of correlation r of 0.98 (P<0.01), in contrast to the previous concept that “goiter prevalence increased with age before the era with iodine intervention. This finding is consistent with a previous report entitled “Swelling Rate of Endemic Goiter in Four Villages in Outskirts of Chengde City, which indicated that all new cases of goiter were basically palpable “swelling, accounting for 91.49% of all the cases, but the cases of “goiter accounted for only 8.51% of them, all with swelling of a second degree of the thyroid. This showed that the swollen thyroid formed under iodine supplementation was not so severe as previously seen before the intervention.
Table 5.7 Intervention efficacy of iodine supplementation on goiter in general population[6] | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree