Eosinophilic Gastrointestinal Diseases
Terri F. Brown-Whitehorn
Kernika Gupta
Ritu Verma
Jonathan M. Spergel
DEFINITIONS OF EOSINOPHILIC GASTROINTESTINAL DISEASES
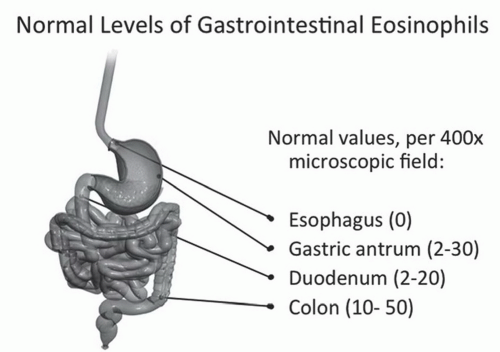
Eosinophilic Gastrointestinal Diseases (EGIDs) are allergic and/or inflammatory conditions defined by the presence of an abnormal level of eosinophils in the gastrointestinal (GI) tract, in absence of idiopathic hypereosinophilic syndrome, parasitic infection, drug reaction, and inflammatory bowel disease (IBD) or other causes of eosinophilia. It is important to remember that eosinophils can exist normally in the GI tract. The number of eosinophils varies in different parts of the GI tract, ranging from zero in the esophagus to 20 to 40 in the stomach and colon (Fig. 17-1). EGIDs are divided based on the location of abnormal eosinophils, esophagus (eosinophilic esophagitis [EoE]), colon (eosinophilic colitis [EC]), or entire GI tract (eosinophilic gastroenteritis [EG]). For all classifications of EGIDs, symptoms can include failure to thrive, dysphagia, food impaction, abdominal pain, and reflux that are nonresponsive to proton pump inhibitors (PPIs), while lower abdominal symptoms (diarrhea, bloating) being more common in EG and EC. These clinical symptoms alone are nonspecific to EGIDs, and symptoms can occur continuously or variably over time in individuals with EGIDs.
I. TYPES OF EGIDS
A. Eosinophilic Esophagitis (EoE) is characterized by the presence of 15 or more eosinophils per high power field and inflammation in the esophagus. However, eosinophils can occur in the esophagus from other etiologies including gastroesophageal reflux disease (GERD), allergic rhinitis, fungal infection, and IBD. Due to this confusion, two consensus meetings have occurred with development of agreed-upon definition with most recently published in 2011.
Eosinophilic esophagitis represents a chronic, immune/antigen mediated, esophageal disease characterized clinically by symptoms related to esophageal dysfunction and histologically by eosinophil-predominant inflammation… Eosinophilic esophagitis (EoE) is a chronic clinico-pathological disorder of the esophagus, characterized by a spectrum of symptoms referable to esophageal dysfunction that occur in association with esophageal mucosal biopsy specimens containing ≥15 intraepithelial eosinophils/high power field (HPF) in one or more biopsy specimens. The disease is isolated to the esophagus and other causes of esophageal eosinophilia must be excluded. Typically, the disease remits with treatments including dietary exclusions and/or topical corticosteroids.
EoE can affect both children and adults, with some variation in symptom presentation (detailed below). There are several consistent features: highly atopic with >70% of patients having at least one feature of atopy
(asthma, allergic rhinitis, IgE-mediated food allergies, or atopic dermatitis) and a strong male predominance 3:1.
(asthma, allergic rhinitis, IgE-mediated food allergies, or atopic dermatitis) and a strong male predominance 3:1.
B. Eosinophilic Gastroenteritis (EG) is characterized by the presence of various GI symptoms and the presence of 30 or more eosinophils present in the GI tract, most commonly in the gastric antrum or small bowel. EG affects both children and adults but tends to dominate more in males. Clinical symptoms can include abdominal pain, diarrhea, weight loss, and vomiting, which are all nonspecific to EG. The symptoms and clinical presentation are typically more severe than EoE. Other symptoms that can be a sign of severe disease include GI bleeds, anemia, and hypoalbuminemia, also nonspecific findings. These symptoms can mimic numerous other conditions such as IBD, chronic granulomatous disease (CGD), Helicobacter pylori infection, parasitic infection, idiopathic hypereosinophilic syndrome, or even hypertrophic pyloric stenosis in infants. Potential laboratory tests to consider in a workup of EG include serum IgE level, stool studies, allergy testing, IBD panel, CBC/differential, complete metabolic panel, and radiologic studies, as well as a mandatory endoscopy and colonoscopy.
C. Eosinophilic Colitis (EC) is a rare manifestation of EGIDs that is characterized by the presence of abnormal level of eosinophils in the colon, in absence of any other condition related to hypereosinophilia such as inflammatory bowel disease, parasitic infections, drug reactions, or autoimmune connective disorders. Additionally, the presence of eosinophils in the colon may be due to allogeneic bone marrow transplantation, Tolosa-Hunt syndrome, and idiopathic hypereosinophilia syndrome, all of which rarely can manifest by EC. The etiology behind EC is most obscure of all the EGIDs. In some cases, EC might be precursor of IBD as eosinophils can occur in IBD in isolation. Diagnosis is dependent on the presence of an abnormal level of eosinophils in the colon, which is dependent on what area biopsies are taken. Normal levels of eosinophils for the rectum are <10 eosinophils per high power field but can be >30 eosinophils per high power field in the cecum (Fig. 17-1). Therefore, biopsy location correlating eosinophil levels
are highly important in the diagnostic procedure for EC. Many children with EC may have complete resolution of symptoms over time without intervention, whereas others may have resolution based on removal of atopic agents defined as the possible triggers for EC. In adults, EC may resolve without intervention or after removal of atopic agents, but there is a chance for relapse despite removal of atopic agents.
are highly important in the diagnostic procedure for EC. Many children with EC may have complete resolution of symptoms over time without intervention, whereas others may have resolution based on removal of atopic agents defined as the possible triggers for EC. In adults, EC may resolve without intervention or after removal of atopic agents, but there is a chance for relapse despite removal of atopic agents.
II. PREVALENCE AND INCIDENCE
The actual incidence and prevalence of EGIDs are hard to estimate as ICD-9 diagnostic codes have only been recently established in 2008: Eosinophilic Esophagitis—530.13, Eosinophilic Gastritis—535.7, Eosinophilic Gastroenteritis—558.41, and Eosinophilic Colitis—558.42. However, estimates for EoE have been done in two ways: (1) random sampling/biopsy of local population and (2) examining the number of patients seen in local population. The major issue with the random sampling of a population is that other causes of esophageal eosinophilia have not been ruled out. In addition, the prevalence rates are related to the number of eosinophils used as the diagnostic criteria with rates as high as 1,100/100,000 when it was based on >10 eosinophils/HPF. Examination of local populations has found an estimated prevalence that is much lower, around 7 to 70/100,000, in the United States and Switzerland. This suggests that many cases of EoE are possibly being missed and we are just seeing the tip of the iceberg. To get a national estimate, we recently completed an Internet survey of all gastroenterologists and allergists in the United States and asked them to estimate the number of new patients that they see in one year. Based on their numbers and population in each state, we calculated an overall prevalence of EoE in the United States at 52/100,000 population, similar to the local estimates.
The other interesting observation seen in several centers is that there has been a large and steady growth in almost exponential fashion in the number of cases of EoE diagnosis in the last 10 to 15 years. However, recent studies have suggested that a large portion of this increase might be due to increased number of procedures and recognition of the disease.
The epidemiology of EG and EC has not been well studied, and estimates are unclear because most studies are small. Our same Internet survey of US gastroenterologists found an estimate for combination of EG and EC at 28/100,000 population, indicating these are rare diseases.
III. PATHOGENESIS OF EGIDS
Eosinophilic esophagitis has been proposed to be atopic dermatitis of the esophagus based on murine and human studies. Like several other diseases, individuals likely have a genetic susceptibility and an allergen trigger leading to recruitment of inflammatory cells and disease.
A. Genetic susceptibility
EoE is similar to most atopic diseases being multifactorial. However, EoE has a stronger genetic component with high sibling risk ratio of 80 compared to asthma at 2. Candidate gene studies have identified eotaxin-3 and thymic stromal lymphopoietin (TSLP) as being important. There have been no genetic studies done on EG or EC.
B. Allergen trigger
Both foods and aeroallergens can induce EoE. In human models, pollen exposure in patients with allergic rhinitis induces esophageal and duodenal eosinophilia but typically not to levels seen in EoE. In almost all patients (adult and pediatrics), foods have been shown to be a trigger for EoE, and removal of the food resolves eosinophilia, and reintroduction causes EoE.
C. Inflammatory cells
EoE has other inflammatory cells, such as TH2 cells and mast cells, which contribute to the symptoms and progression of the disease. Esophageal biopsies show marked TH2 inflammatory responses. IL-13, IL-4, TGF-b1, and STAT 6 are all thought to be important factors in disease pathogenesis. Periostin is induced by IL-13 and regulates eosinophil recruitment and adhesion, promoting a cycle of increased disease. Children with untreated eosinophilic esophagitis have basement membrane thickening and increased vascular activation, similar to changes seen in airway remodeling and asthma. Fibrosis and dysmotility lead to esophageal dysfunction and dysphagia in patients.
D. Atopic nature of EGID
Patients with EGID, especially EoE, are much more likely to be atopic than the general population. In the United States, 8% of adults and 10% of children have asthma, 10% to 30% of adults and 40% of children have allergic rhinitis, 3% of adults and 10% to 20% of children have atopic dermatitis, and 3% to 4% of adults and 6% of children have IgE-mediated food allergy. In comparison, 80% of EGID patients in a world-wide registry were atopic (38% had asthma, 64% had allergic rhinitis, 26% had atopic dermatitis, and 23% had IgE-mediated food allergy). Two-thirds of our pediatric patients at The Children’s Hospital of Philadelphia had atopy in our recent 14-year review. Similar high rates were seen in adults with almost 2× the rate of atopy than the general population (asthma—26%, allergic rhinitis—78%, and atopic dermatitis—3%) (Table 17-1).
1. Food allergens: The role of food allergies in EoE has been clearly defined and has fulfilled Koch’s postulate. Many studies have shown that removal of foods with an elemental diet led to resolution of all symptoms and normalization of endoscopy and biopsy. Either empiric or allergen testing-derived elimination of individual foods also leads to resolution of symptoms and endoscopic and histologic features in 70% to 80% of pediatric patients. The reintroduction of the positive foods leads to symptoms and esophageal eosinophilia returning, fulfilling Koch’s postulate that food can cause EoE.
2. Aeroallergens: Aeroallergens may play a role in EoE and EG based on several key facts. Patients with EoE are sensitized to a variety of aeroallergens. Diagnosis of new EoE cases increases during pollen seasons. Pollen can cause esophageal eosinophilia. It has been shown that pateints with allergic rhinitis have esophageal eosinophilia when they have endoscopies and biopsies during grass pollen season and that the biopsy worsened during the pollen season and normalized outside of the pollen season while the diet and medications remained unchanged. Although pollen plays a role in patients with EoE, most often it is not the only trigger. For EG, allergic patients were also shown to have an increase in eosinophils and IgE-bearing cells in the duodenum during the tree pollen season as compared with off-season.
Table 17-1 Studies Showing the Frequency of Atopic Disease (%) in Normal Population and EoE Patients | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|