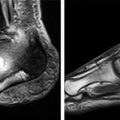
Figure 8.1
Reconstructed MRA images demonstrating the typical combination of SFA and infra-geniculate disease found in diabetic PAD. (a) Bilateral SFA occlusions with collateral reconstitution of the popliteal artery (arrow). (b) Bilateral proximal occlusions of the anterior tibial artery and multi-level occlusive disease of the left posterior tibial artery (arrow)
Treatment Options
Multiple factors need to be considered before considering revascularisation. These include clinical findings, degree of tissue loss, degree of ischaemia, the age of the patient, life expectancy, co-morbidities and the level and extent of arterial disease.
It must be ensured that all patients are on best medical therapy – this includes optimising glycaemic control and treatment of hypertension and dyslipidaemia. Optimal wound care, treatment of infection and good foot care are also vital, both pre- and post-procedure.
There are two options for revascularisation of the diabetic limb; endovascular treatment or surgical bypass. The Transatlantic Inter Society Consensus (TASC) classification system of PAD, first published in 2000 [1] and revised in 2007 [3], is based on the morphological characteristics of the arterial lesions, and was designed to guide the treatment of symptomatic patients (Table 8.1). In brief, TASC II recommendations for femoro-popliteal disease are endovascular therapy as first-line treatment for type A and B lesions and surgery for “good risk” type C lesions and type D lesions. The TASC recommendations for infra-popliteal arterial disease are endovascular treatment of type A and B lesions, and bypass for type C and D lesions. TASC II did conclude that there is growing evidence to support endovascular therapy for infra-popliteal disease.
Table 8.1
TASC classifications for infrapopliteal and femoropopliteal arterial disease
TASC infrapopliteal classifications | |
|---|---|
Type A | Single stenosis shorter than 1 cm in the tibial or peroneal vessels |
Type B | Multiple focal stenosis of the tibial or peroneal vessel, each less than 1 cm in length. |
One or two focal stenosis, each less than 1 cm long at the tibial trifurcation | |
Short tibial or peroneal stenosis in conjunction with femoropopliteal PTA | |
Type C | Stenoses 1–4 cm in length |
Occlusions 1–2 cm in length of the tibial or peroneal vessels | |
Type D | Tibial or peroneal occlusions longer than 2 cm |
Diffusely diseased tibial or peroneal vessels. | |
TASC femoropopliteal classification | |
|---|---|
Type A | Single stenosis <10 cm in length or single occlusion <5 cm in length |
Type B | Multiple lesions each <5 cm |
Single stenosis or occlusion <15 cm not involving the infrageniculate popliteal artery | |
Heavily calcified occlusion <5 cm in length | |
Type C | Multiple stenosis or occlusion totaling >15 cm with or without heavy calcification. |
Recurrent stenoses or occlusions that need treatment after two endovascular interventions | |
Type D | Chronic total occlusion of the common or superficial femoral artery (>20 cm, involving the popliteal artery) |
Chronic total occlusion of the popliteal artery and proximal trifurcation vessels. | |
Endovascular revascularisation was first performed in 1964 by Charles Dotter. Since then there has been continued development of endovascular techniques and equipment particularly for infra-popliteal disease and the indications for endovascular intervention continue to expand.
There is limited level 1 evidence comparing endovascular treatment with open bypass. The BASIL trial was published in 2005 [4] and demonstrated that at 1 year that there was no difference in amputation or overall survival between patients with severe limb ischaemia treated initially with bypass surgery or endovascular therapy. At 2 years there was a survival advantage in the bypass group and a trend towards improved amputation-free survival. BASIL comprised a heterogeneous group of patients with both above- and below-knee disease, and no sub-group analysis of diabetic patients was performed. BASIL showed vein grafts had better long-term patency than prosthetic grafts. This data has been used to suggest angioplasty for short-term revascularisation, and bypass surgery if the patient has reasonable life expectancy and suitable anatomy.
A recent study that performed propensity score analysis of 1,023 patients with CLI, of whom 262 underwent percutaneous transluminal angioplasty (PTA) and 761 surgical bypass, reported similar 5 year results for leg salvage (75.3 % vs. 76 %), survival (47.5 % vs. 47.3 %) and amputation-free survival (37.7 % vs. 37.3 %) [5].
Endovascular treatment is less invasive and has lower post-procedural morbidity. A study that used the National Surgical Quality Improvement Program database showed the composite mortality and morbidity rate of infra-inguinal bypass was as high as 19.5 % [6].
The improved durability of newer endovascular therapies, improvements in technical methodology, comparable outcomes from endovascular therapies and low procedural morbidity has led to many groups proposing an endovascular first approach for TASC C and D lesions.
There has been controversy regarding whether a failed endovascular procedure may jeopardise open surgery options. As long as an undamaged, unstented landing zone is preserved, a failed PTA does not seem to preclude future bypass [3]. Surgical options may be affected by stents at potential bypass anastomotic sites, and close collaboration between endovascular practitioners and vascular surgeons is required. Robust surveillance strategies must be in place following PTA to ensure additional treatment can be performed if required.
Endovascular Treatment
Pre-procedure
There are a number of important pre-procedural considerations. The patient needs to be able to lie flat and still for the procedure (possibly for a number of hours) and if they are unable to do this then anaesthetic support for sedation and possibly general anaesthetic may be required. Pre-procedural imaging and previous endovascular interventions must be carefully reviewed. Recent blood tests should be available, particularly renal function. Aspirin should be continued pre-procedure and has been shown to reduce the incidence of peri-procedural thromboembolic events. If the patient is on warfarin this should be stopped, aiming for an INR <1.5 before intervention is performed.
Treatment Site
The principle of any vascular intervention is to first ensure that inflow is restored (i.e., the most proximal level of disease is treated), before considering more distal intervention. Whilst much emphasis is placed on the below-the-knee (BTK) disease in patients with diabetes it is important to remember this principle and ensure that proximal iliac or femoral disease is adequately treated. It is also important to relate the severity of the clinical presentation to the planned endovascular treatment. For example, patients with intermittent claudication and combined SFA and BTK disease may derive sufficient benefit from treatment of the SFA disease alone, whereas patients with tissue loss usually require multi-level intervention.
A relatively recent concept is that of angiosome treatment, which has particular relevance to treating diabetic ulceration. The foot is divided into distinct vascular territories or angiosomes, one each from the anterior tibial (AT) and peroneal arteries (PA) and three from the posterior tibial (PT) artery. The AT supplies the dorsal side of the foot and toes, the PA supplies the lateral ankle and lateral heel, and the PT perfuses the plantar surface of the foot and the medial heel. There are small collateral vessels in the foot known as choke vessels, which are often compromised in diabetic patients. Studies have suggested that restoration of direct perfusion of the affected part of the foot, based on the angiosome concept, results in improved ulcer healing. Angiosome-targeted perfusion may not be possible due to severe disease of the target vessel. Some operators propose that, if possible, multiple vessels should be re-canalised. This technique improves total foot perfusion, and provides some insurance against subsequent blockage. We would initially try to treat the target angiosome vessel supplying the area of the foot with the ulcer or wound, but if this was not possible then we would attempt to restore flow in other vessels.
Arterial Access
We use ultrasound guidance for all arterial punctures, as this reduces access site complications. The access route depends on the planned site of intervention. Antegrade access indicates the sheath is pointing in the direction of arterial flow, and retrograde access against the arterial flow. Antegrade common femoral artery access is usually employed for infra-inguinal disease, because the straight-line approach allows more “pushability” when trying to cross lesions and is preferable when performing a very distal intervention. Antegrade access may not be possible in obese patients or those with heavily scarred groins.
Retrograde common femoral artery access and an ‘up and over’ approach enable simultaneous assessment and treatment of iliac disease, and is appropriate for treating common femoral artery (CFA) or proximal SFA disease. A contralateral approach requires longer guide-wires, catheters and balloons, and monorail systems may prove useful. A contralateral approach may not be successful in patients with very tortuous or angulated iliac arteries.
Retrograde popliteal or below knee vessel access is becoming increasingly common for the treatment of more complex cases. Dedicated micro-puncture systems and pedal access sheaths are available for such cases.
Crossing Lesions
The first stage of endovascular recanalisation is crossing the lesion. This can be achieved either intra-luminally or in the sub-intimal plane. There has been much debate over which type is preferential, but in practice, the type of lesion usually dictates the crossing technique. Stenoses are usually crossed intra-luminally and longer occlusions typically require a sub-intimal approach
To create a sub-intimal channel, a guide catheter is pointed towards the arterial wall at the proximal aspect of the occlusion and a hydrophilic guide-wire is passed into the space between the intima and media. The looped guide-wire is used to dissect a sub-intimal tract and then passed back into the true lumen at the distal end of the occlusion. Angioplasty then displaces the atheromatous and calcified intimal and medial layers to the contralateral side of the lumen, thus creating a neo-lumen. Care should be taken not to extend the created sub-intimal tract too distally, so as to preserve collaterals as well as possible distal targets for bypass. Re-entry into the true lumen may not be possible, particularly in extensively calcified vessels (reported up to 10–15 % of cases). Specialised re-entry devices are available such as the Outback® (Cordis) and Offroad® (Boston Scientific, Natick, MA, USA) devices. The Outback device is a 6F compatible catheter with a sharp, hollow 22G needle that can be directed towards and used to puncture back into the true lumen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree