Fig. 14.1
Variety of EMRs. (a) EMR with a ligation device (EMR-L). A lesion is suctioned and ligated with O-ring before resection. (b) EMR using a cap-fitted endoscope (EMR-C). A lesion is suctioned into a transparent hood and resected by the snare. (c) Endoscopic esophageal mucosal resection (EEMR)-tube method. A long transparent silicon overtube is used for suctioning the lesion. (d) Two-channel EMR method. A forceps is used for grasping and pulling the lesion
EMR with a ligation device (EMR-L) requires an O-ring used for esophageal varices ligation (Fig. 14.1a) [14]. In this technique, after suctioning a lesion and ligating it with the O-ring to create a pseudopolyp, endoscopic resection is performed just below the O-ring using a snare. Although submucosal injection before the resection is conventionally desirable in order to avoid unexpected perforation, endoscopic resection using a ligation device without submucosal injection seems to be also acceptable especially for early Barrett’s neoplasia [15].
In EMR using a cap-fitted endoscope (EMR-C), a transparent hood attached to the tip of the endoscope is used (Fig. 14.1b) [16]. After opening a semilunar snare along the rim of the hood, an elevated lesion by submucosal injection is suctioned into the hood and resected by the snare. In this technique, setting the snare along the rim of the hood can be difficult and time-consuming that it sometimes makes the operator irritated.
In endoscopic esophageal mucosal resection (EEMR)-tube method, a long transparent silicon overtube is used (Fig. 14.1c) [17]. After submucosal injection, the lesion is suctioned by the overtube introduced over the endoscope and tightened by a snare preliminarily introduced through the side channel of the overtube. Resection should be done after confirming that the muscular layer is not involved because a diameter of the overtube is much larger than any other EMR caps.
A grasping and pulling technique using a two-channel endoscope is called two-channel EMR method (Fig. 14.1d) [18]. A grasping forceps from one working channel is passed through a snare introduced from the other channel. The elevated lesion by submucosal injection is grasped with the forceps and tightened with the snare at the bottom of the grasped mucosa. Again, resection should be done after confirming that the muscular layer is not involved within the ligated tissue.
Because the size of snares is limited in these EMRs, available size of en bloc resection is also limited [3, 4, 19, 20]. Expected maximal size of one specimen is thought to be approximately 2 cm. Besides, the resectable size is also limited by the diameter of the O-ring in EMR-L, the hood in EMR-C, and the overtube in EEMR-tube. Furthermore, in case of having severe fibrosis under the lesion, it usually becomes quite difficult to resect the lesion by these EMRs because a snare is easily slipped from the target. Accordingly, early esophageal cancer 1 cm or less without fibrosis would be suitable for a candidate of EMR in usual clinical settings.
14.4 Endoscopic Submucosal Dissection (ESD)
This epoch-making technique is composed of four steps: marking around the lesion after chromoendoscopy, submucosal injection, circumferential mucosal incision, and dissection of the submucosal connective tissue (Fig. 14.2). Because the operator can determine the extent of resection and dissect the submucosal tissue under the direct vision, ESD can offer reliable en bloc, margin-free resection irrespective of the size or presence of submucosal fibrosis.
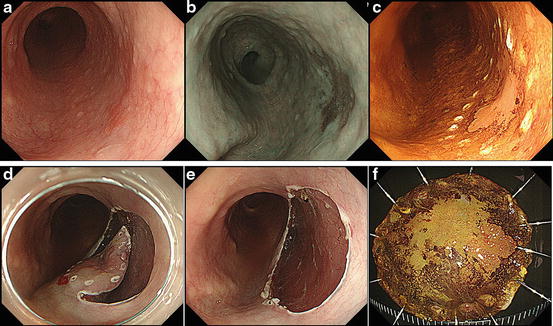
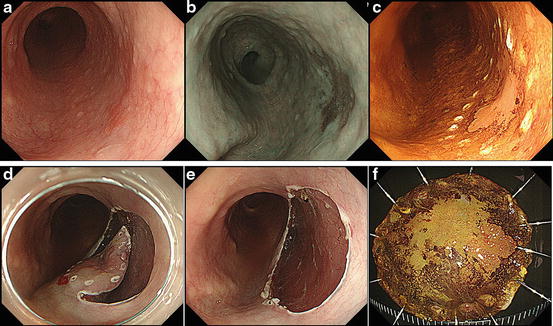
Fig. 14.2
Representative case of esophageal endoscopic submucosal dissection (ESD). (a) Conventional image of squamous cell carcinoma. A reddish lesion is located on the posterior wall of the esophagus. (b) Image-enhanced endoscopy by narrow-band imaging. The lesion can be visualized more clearly compared to the conventional image. (c) Markings are placed around the lesion with an appropriate margin. (d) Circumferential mucosal incision except for one lateral side and subsequent submucosal dissection is made from the upper side. (e) Resection wound after ESD. (f) An en bloc resection enables precise histological assessment (esophageal squamous cell carcinoma, pT1-a, 18 × 14 mm, ly0, v0, pHM0, pVM0)
14.4.1 Details of Practical Skill
Among various electrocautery knives specialized for ESD, pointed tip-type knives would be suitable especially for esophageal ESD due to the narrow lumen and the thin wall of the esophagus (Fig. 14.3) [21–23].
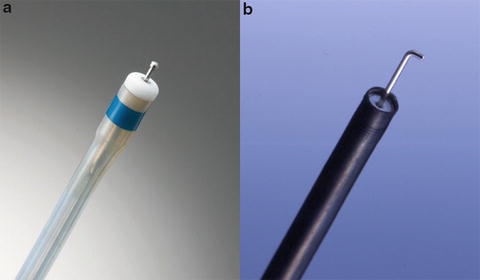
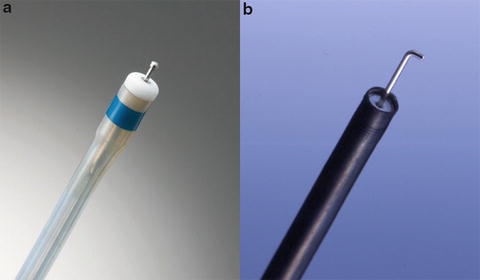
Fig. 14.3
Pointed tip-type knives. (a) Dual knife. (b) Hook knife
Successful resection requires accurate endoscopic diagnosis of a tumor extent. Although promising image-enhancement endoscopy techniques have been introduced, conventional chromoendoscopy using iodine spraying would be still most useful in determining the extent of the lesion. Using a tip of the knife, markings are made 2–3 mm outside the lesion at intervals of approximately 3 mm.
In creating a submucosal fluid cushion, an injection needle is gently advanced into the submucosa at the outside of markings, and a fluid colored with a small amount of indigo carmine, which is helpful to visualize the submucosa, is injected into the submucosa to make sufficient submucosal space for incision and dissection. Hypertonic or viscous injection fluid such as Glyceol™ (Chugai Pharmaceutical Co., Japan; consisted of 10 % glycerine, 5 % fructose, and 0.9 % sodium chloride) or hyaluronic acid solution is desirable for long-lasting submucosal cushion. Injection directly through the cancerous area should be avoided in order to prevent cancer cell implantation in the deeper layer.
The mucosa 1–2 mm outside of markings is usually cut with cutting current using specific knife. Right after partial mucosal incision, initial submucosal dissection should be made along the incision line with coagulation current. To make sure the end point of submucosal dissection, it is better to cut the anal side of the lesion first and subsequently continue the procedure from the oral side.
It is very important to conduct submucosal dissection under direct vision using transparent hood. The knife should be moved parallel to the plane of the muscular layer during submucosal dissection to avoid muscular injury or perforation. Repeat submucosal injection, mucosal incision, and submucosal dissection step by step until end of the procedure.
14.5 Management of Complications
14.5.1 Bleeding
Unlike gastric ESD, the rate of postoperative bleeding is relatively low (0–2 %) [24–27]. In case of minor bleeding, hemostasis using the retracted tip of the knife is firstly attempted. When it is difficult to stop bleeding or it bleeds massively, hemostatic forceps should be used. After the retrieval of the resected specimen, the resection wound should be carefully inspected to check for visible vessels. And every thick exposed blood vessels should be coagulated, avoiding excessive thermal damage.
14.5.2 Perforation
Perforation should be paid more attention especially in esophageal ESD. Because the esophagus has no serosa, exposure of the muscular layer may cause pneumomediastinum [28, 29]. Indeed, pneumomediastinum was found by CT scan in a half of treated cases after esophageal ESD, although fortunately these were almost subclinical [28]. Damage of the muscular layer might lead to delayed perforation, which could become fatal mediastinitis. Therefore, it is necessary to follow up the patient carefully, especially after perforation, muscular injury, and severe thermal damage. In case of perforation, patients are treated at rest with fasting and administered antibiotics until a fever and inflammation are relieved. Generally, emergency endoscopy for the purpose of detection and closure of a perforation site is not indicated because it may be not only ineffective but also a cause of spread of mediastinitis.
14.5.3 Postoperative Stricture
The risk of postoperative stricture is particularly higher in esophageal ESD (Fig. 14.4) [10, 11]. Because the probability of stricture mostly depends on the resected size, a lesion over three-fourths of circumference is relative indication of ESD as previously mentioned. Several attempts to prevent postoperative stricture have been tried [30–35], e.g., prophylactic endoscopic balloon dilatation and local injection or oral administration of steroids. Preclinical trials are also considered such as adipose tissue stem cell transplantation [36] or cultured cell sheet transplantation [37, 38], but there has been no decisive method so far. Further investigation would be necessary to overcome this problem.
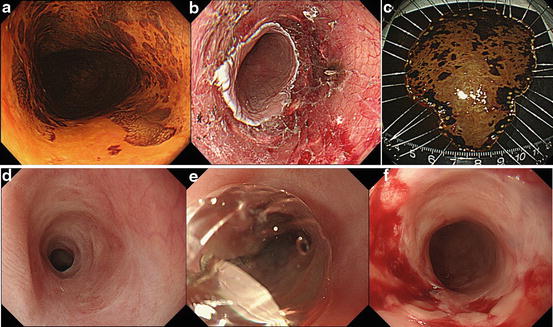
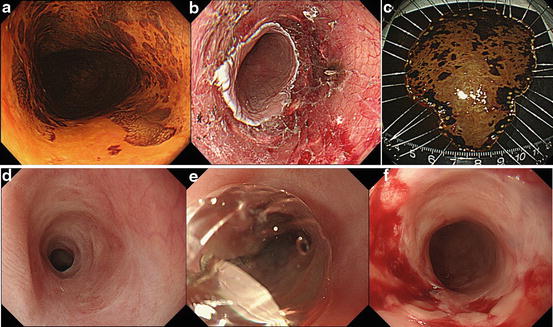
Fig. 14.4
Severe stricture after extensive resection. (a) Superficial cancer extending a whole of circumference. (b) Since resection wound become circumferential, steroid solution is injected into remaining submucosa in order to prevent severe stricture. (c) Complete margin-free resection is achieved. (d) Even after steroid injection, severe stricture has been developed a few weeks later. (e) Endoscopic dilatation using CRE™ balloon dilator (Boston Scientific Co., USA). (f) Mucosal and submucosal fissure after balloon dilatation. It took nearly half a year to have stable condition with multiple balloon dilatation
14.6 Outcomes of ESD for Esophageal Squamous Cell Carcinoma
14.6.1 Short-Term Outcomes
Favorable treatment results have been reported from high-volume centers particularly in Japan [24–27]. In short-term outcomes such as a technical feasibility of esophageal ESD, over 90 % of complete resection rate is obtained, whereas the rates of major complications such as delayed bleeding or perforation keep below 2 % in leading centers for ESD. Even if complication occurred, it can be managed conservatively and thus hardly becomes a life-threatening condition. Technically, ESD for the lesion near the esophagogastric junction is sometimes difficult and time-consuming because intraoperative bleeding from abundant collecting vessels occurs frequently. The lesion located in the cervical esophagus, one of natural constrictions, is also difficult to resect because of poor visualization. Furthermore, the risk of aspiration pneumonia becomes extremely high by reflux of fluids (e.g., blood, rinsing water, submucosal fluid). In that case, ESD with general anesthesia should be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree