Fig. 8.1
This is a case of a 93-year-old female who was referred to our hospital for the treatment of a gastric tumor that by biopsy was group 3. Conventional endoscopy revealed a circumferential, slightly elevated lesion in the gastric antrum, which was resected by ESD as an expanded indication. Pathological diagnosis was 110 × 65 mm, type 0–IIa, adenocarcinoma, T1a, ly0, v0, HM0, and VM0
Therapeutic Efficacy of Endoscopic Resection
The resected specimen should be handled according to the rules described in the Japanese classification [2] (Table 8.1).
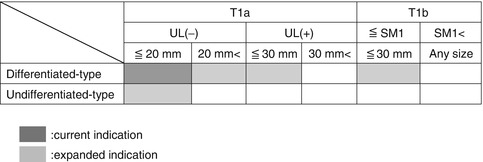
Table 8.1
Indication for ESD: current and expanded indications
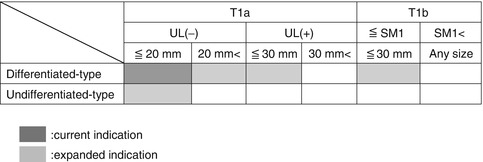
Curative tumor resection was previously defined as en bloc resection of a differentiated-type tumor, ≦2 cm in size, pT1a, negative horizontal margin (HM0), negative vertical margin (VM0), and no lymphovascular infiltration (ly(−), v(−)).
Following the expanded criteria for ESD in EGC, resection is considered curative when all of the following conditions are fulfilled:
En bloc resection, HM0, VM0, ly(−), v(−)
(a)
Tumor size ≧2 cm, histologically of a differentiated type, pT1a, UL(−)
(b)
Tumor size ≦3 cm, histologically of a differentiated type, pT1a, UL(+)
(c)
Tumor size ≦2 cm, histologically of undifferentiated type, pT1a, UL(−)
(d)
Tumor size ≦3 cm, histologically of differentiated type, pT1b (SM1,<500 μm from the muscularis mucosae)
Follow-up abdominal ultrasonography or computed tomography (CT) scan and annual or biannual endoscopy are still recommended in all cases of curative resection meeting the expanded criteria.
Summary
The expanded criteria for ESD are now being employed as more endoscopists become skillful in performing ESD. As the procedure is offered to more patients, further studies on clinical efficacy and safety following the expanded criteria are warranted [13].
Device for ESD [14–16]
Knives for ESD
Knives used for ESD have been conventionally classified into needle type or insulated tip type based on the design, shape, and method of use. At present, various knives are available including those designed for use in areas in which the approach is difficult or knives which increase the safety intraoperatively. However, use of this wide range of knives requires an adequate understanding of the properties of each to allow their application under appropriate conditions.
The ESD knives currently available in Japan are described and classified below into (1) needle type, (2) IT-knife type (insulation-tipped type), (3) non-IT-knife type, and (4) scissors forceps type (Table 8.2, Fig. 8.2).

Table 8.2
High-frequency knives for ESD
Needle Knife type | Flush knife (DK2618JB/DK2618JN, Fujifilm Co.) |
Flex knife (KD-630 L, Olympus Co.) | |
Triangle Tip Knife (KD-640 L, Olympus Co) | |
Dual Knife (KD-650 L/KD-650Q, Olympus Co) | |
Hook Knife (KD-620LR/KD-620QR, Olympus Co.) | |
IT-knife type | IT-knife, IT-knife-2, IT-knife-nano (KD-610 L/KD-611 L/KD-612, Olympus Co.) |
Non-IT-knife type | Mucosectom (DP-2518, PENTAX Co.) |
SAFE knife (DK2518DV1, Fujifilm Co.) | |
Swanblade (DC-D2618, PENTAX, Tokyo) | |
Scissors forceps type | Clutch Cutter (DP2618DT, Fujifilm Co.) |
SB knife and SB knife Jr. (MD-47706/MD-47704 and MD-47703, Sumitomo Bakelite Co.) |

Fig. 8.2
Knives for ESD. Upper left, Flush knife; Upper right, Hook Knife; Center left, IT-knife-2; Center right, Mucosectom; Lower left, Clutch Cutter; Lower right, Flex knife
Needle Type
Short needle is the representative type in this category (although Needle Knife (Olympus Co., Tokyo Japan), which has a long sharp non-covered needle, was originally used for ESD). This knife enables the endoscopist to perform ESD with direct visualization of the area to be cut. Both incision and dissection can be done using this device. Among the short-needle type, Flush knife (Fujifilm Co., Tokyo, Japan) is used routinely in our hospital. The Flush knife has a water-jet function that makes additional submucosal injection possible. It also has two kinds of tip types (needle or ball-chip), and four kinds of knife lengths are available at 5 mm intervals (1.0–3.0 mm). The endoscopist should take into consideration both which organ (i.e., esophagus, stomach, colon) and the location of the lesion in choosing the suitable tip type and protruding length to be used for treatment. In our hospital, the Flush knife with a needle type tip, 2.0 mm in length, is employed for gastric ESD.
The other category is the hook type, represented by the Hook Knife (Olympus Co., Tokyo, Japan). The distal L-shaped hook has a rotatory function allowing for incision and dissection in longitudinal and lateral directions. This is done by simply turning the handle to point the tip of the hook in the desired direction. Moreover, the Hook Knife also enables the operator to “hook” tissue and pull away from the muscle layer, as its name suggests. This method minimizes the risk of perforation especially in cases of severe fibrosis as cutting is done away from the muscle layer. The drawback of using this knife, however, is that the amount of tissue that can be hooked at a time is limited prolonging procedure time.
IT-Knife Type
IT-knife and IT-knife-2 (Olympus Co., Tokyo, Japan) are the main knives used for gastric ESD. The ceramic insulator attached at the tip of the needle-shaped knife does not conduct electricity thereby minimizing invasiveness and reduces the risk of perforation. It allows lateral cutting from a vertical approach. To perform steady submucosal dissection, the ceramic globule and the sheath should be positioned properly on the surface of the incision or area to be dissected. It is said that procedure time is shorter when using IT-knife effectively because the contact area between the blade and surface is increased due to “line” touch (understandably, needle type attach in a point), and tension can be applied during the dissection due to non-electrical conductivity of the tip. The downside of this knife is its high coagulation capacity causing tissue carbonization or charring which eventually prevents proper tissue contact and adequate depth dissection (see below “high-frequency generator”).
Recently, the IT-knife-nano was developed, with a compact ceramic tip and small disklike structure of the backside electrical blade. It is expected to work effectively in difficult cases particularly with severe fibrosis.
Non-IT-Knife Type (Insulator Processing)
Mucosectom (HOYA PENTAX Co., Tokyo, Japan) is a knife wherein the tip and the lateral sides are covered by an insulator. In addition, the blade has a rotatable function enabling adjustments in the direction of dissection. This knife can be used as a secondary knife rather than a primary knife, reserving its use in cases where the position of the knife is perpendicular to the muscle layer and area of dissection especially in cases of severe fibrosis.
Scissors Forceps Type
This device was developed combining the design concepts of the conventional knife like Needle Knife and IT-knife type. The Clutch Cutter (Fujifilm Co., Tokyo, Japan) is representative of this category. These knives have the capability to grasp and cut tissue in direct view. Moreover the Clutch Cutter can also be used to perform hemostasis.
A large variety of ESD devices have now been developed and launched by several companies. Each knife has some unique characteristics in terms of sharpness for incision/dissection and capacity to do hemostasis. Therefore, the endoscopist should be cognizant of the knife features which will guide choosing the tool or device to be used in a particular situation.
Endoscope
The endoscope for ESD should have the following:
1.
Flush function
The water-jet function is important to clear the mucus from the lesion or to find the bleeding point. Clear water with small amount of dimethicone is used in our hospital.
2.
Channel (size, number)
The internal diameter of scope is a minimum of 2.8 mm considering the external diameter of each device. For the purpose of removing the smoke or mucus during the procedure, a 3.2 mm diameter channel is more desirable. A two-channel scope enables us to perform efficient suction (one channel for the device, another for suction) and effective dissection (one channel for the device, another for injection).
3.
Flexure point
The maximum angle of the scope is an important factor in approaching the lesion.
The multi-bending function means that the second flexure point is set at the posterior side of the first, which enables an approach to any lesion.
4.
Outside diameter
In general, big external diameter means multi-function (water-jet function, 2-channel, etc.). However, for lightening patients’ pain, using the small scope is better.
Small scope also has a small turning circle, which is useful when dissection is performed by handling the endoscopic arm, particularly in the curve.
In our hospital, a 9.9 mm endoscope with water-jet function (Olympus GIF Q260J) is used as our standard. Then if a close approach is difficult, the multi-bending scope (Olympus GIF 2TQ260M) is used.
Distal Attachment
A transparent tip hood is necessary for manipulation in ESD. It exerts tension on the submucosal layer and aids in easy entry into the submucosa. In addition, stable knife operation is possible during the procedure with good visibility even under conditions of body motion, breath movement, and heartbeat by holding down the front mucosa or holding up the lesion.
During the procedure with distal attachment, frequent use of an anti-fouling composition is important. Particularly when ST hood is used, because of its narrow vision, it is effective.
In our hospital, cylindrical hood (Olympus Co D-201-11804) and ST hood (Fujifilm Co DH-15GR)/Short ST hood (Fujifilm Co DH-15GR) are used depending on the situation.
High-Frequency Generator (HFG)
A high-frequency generator (HFG) is an appliance designed for incision or coagulation of tissue. It uses heat-generated high-frequency electrical current applied to the tissue. Incision results from a vapor explosion of cellular membrane caused by continuous delivery of low-voltage current resulting in rapid generation of heat, whereas coagulation results from shrinkage of tissue and evaporation of moisture using intermittent, high-voltage current.
The details with regard to the energy setting of the HFG were discussed previously [14, 17]; however, in general, the configuration mode should be arranged per organ (i.e., esophagus, stomach, colon) and per knife or forceps devices.
Regarding the current density, if it is high, large amount of heat is made, and the incision capacity increases. If it is low, coagulation capacity increases. Meanwhile, current density is influenced by contact area. For example, a point attach (Flush knife, Flex knife) has high current density; on the contrary, a line attach (IT-knife) has low current density. Therefore, if the same output waveforms are used, the needle type point has more incision capacity, and IT-knife has more coagulation capacity (the tissue carbonizes easily). Thus, if the same device is used, current density would also change depending on the method of attaching the tissue.
In our hospital, the HFG VIO 300D (ERBE Elektromedizin GmbH, Tübingen, Germany) is being used during ESD. The following are the HFG settings we use for gastric ESD during the different procedural steps: mucosal marking, forced coagulation mode, 30 w, and effect 4; mucosal incision, Endocut I mode, cut duration 3, cut interval 2, and effect 2; and submucosal dissection, forced coagulation mode, 45 w, and effect 4.
In the next section, among the expanded indications, ESD for EGC with gastric ulcer and for undifferentiated adenocarcinoma is described.
Endoscopic Resection for EGC with Gastric Ulcer
Before Endoscopic Resection
In principle, open gastric ulcer with EGC should be cured by antisecretory medication such as proton pump inhibitor (PPI) or H2 receptor antagonist (H2 blocker) if ESD is kept in mind as the first choice. (In this sentence, open gastric ulcer is defined as active (A) and healing (H) stages, not including the scar (S) stage according to the classification proposed by Sakita and Fukutomi [18].) One of the reasons is, particularly in the acute phase, it is difficult, almost impossible to assess the details of tumors (invasion depth, the extent, etc.) because of modifying factors like inflammatory reaction and edema. Another reason is that the specimen is easily torn by submucosal dissection because the tissue connection is too weak, particularly in the acute ulcer phase. Antisecretory medication is also effective to prevent ulcer relapse of EGC with scar.
In cases of gastric ESD at Northern Yokohama Hospital from July 2007 through March 2013, 38 differentiated adenocarcinomas had endoscopic ulcer findings on the first endoscopy (recurrent cancers were excluded). Thirteen carcinomas were found with the open ulcer. Every patient received medication therapy of PPI or H2 blocker and follow-up endoscopy was performed to assess the ulcer stage (improvement/no change/exacerbation). Regarding cases with open gastric ulcer (n = 13), as the median interval between the first and follow-up endoscopic examinations was 81.6 days (range 28–152), a change in ulcer stage was observed with improvement for 12 patients (92.3 %) and exacerbation for 1 patient (7.7 %). The case with unhealed ulcer is described separately below.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree