Fig. 18.1
Capsule containing the sleeve and the stent positioned over-the-wire to be inserted
Besides providing effective weight loss, the Endobarrier™ has proven to be a valid option for diabetes mellitus treatment. Its main indication is for diabetic obese patients, especially grade I moderate obese with difficult control diabetes [2, 3]. Other possible options include morbid obesity with bariatric surgery contraindication or prior to surgery to ensure effectiveness or decrease complications. Initial studies began in 2005 in Chile, then in Netherlands and Brazil. The device now has clinical approval for 12 m implant in Chile, Europe, Israel and Australia. Approval will be granted for clinical use in Brazil, Argentina and Colombia this year and is currently under an FDA trial in US. Prototypes are under evaluation in trials in Chile for 2 and 3 year implant time.
The aims of the procedure include a rapid improvement in the plasma glucose and HbA1c levels, reduction in diabetes medicine intake, decreased appetite, and increased satiety and weight loss.
The Endobarrier™ is endoscopically placed, under direct and fluoroscopic visualization, using a “push” technique. Removal is also achieved endoscopically, with the aid of foreign body forceps. The procedure is designed to be ambulatory and carried out in endoscopy units.
18.2 Technique
Initial access to the stomach and duodenum is achieved using a standard gastroscope.
The implant is delivered using an over-the-wire catheter system, contained within a capsule at the distal end of the catheter.
The end of the catheter at the tip of the capsule has an atraumatic ball, which helps prevent trauma to the intestinal wall during sleeve deployment.
The capsule is positioned over-the-wire into duodenal bulb (Figs. 18.1 and 18.2
). After that, the ball with the sleeve is extended into duodenum and proximal jejunum up to 60 cm with X-ray guidance (Fig. 18.3).
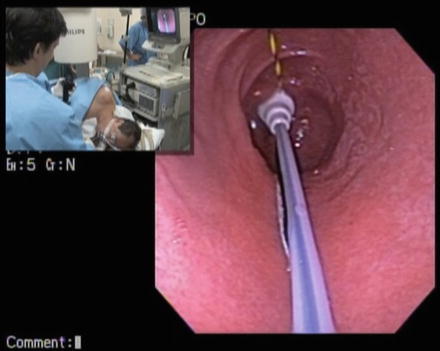
Fig. 18.2
Proper position of the capsule inside duodenal bulb and about to begin the sleeve expansion
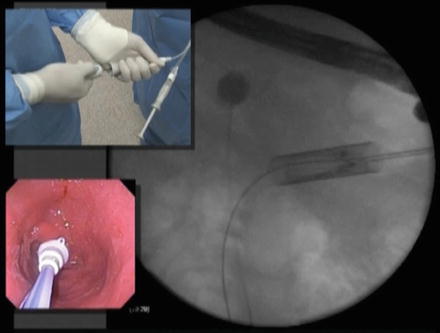
Fig. 18.3
Ball with the sleeve being extended into duodenum and proximal jejunum up to 60 cm with X-ray guidance
After full extension of the sleeve, the ball is released and the anchor deployed in the duodenal bulb 0.5–2 cm distally from the pylorus (Fig. 18.4).
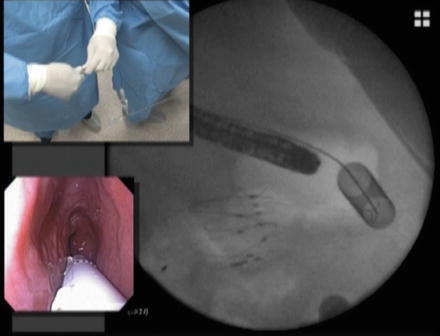
Fig. 18.4
After full extension of the sleeve, the ball is released and the anchor deployed in the duodenal bulb 0.5–2 cm distally from the pylorus
The anchor is self-expanded, and has barbs that will penetrate the tissue to prevent movement. To confirm correct positioning of the sleeve and patency, 60 ml of contrast is flushed.
The catheter is detached form the sleeve and removed from the bowel, leaving the implant in place. Endoscopy view confirms a proper opening of the stent (Fig. 18.5). Figure 18.6 explains the implant in a graphic way.

Fig. 18.5
Endoscopy view confirms a proper opening of the stent
Fig. 18.6
Graph illustration of the Implant
After implant, the liner (the sleeve) will prevent the ingested food to get in touch with the proximal bowel mucosa like a biliopancreatic limb of a gastric bypass (Figs. 18.7 and 18.8)
Fig. 18.7
Graph illustration on how the device prevents the food to reach the duodenum and proximal jejunum wall
Fig. 18.8
Graph illustration on how the device compares with a biliopancreatic limb of a gastric bypass
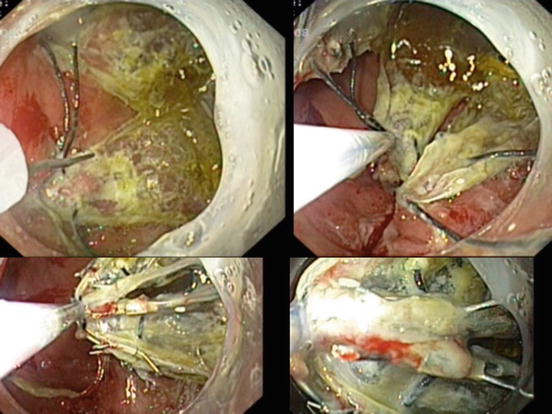
Retrieval at 1 year is accomplished by means of attaching a flexible hood on the endoscope tip and positioning it inside the duodenal bulb. Then, the anchor is collapsed by grabbing one of the proximal drawstrings using a custom grasper (Fig. 18.9)
Fig. 18.9
Retrieval by means of attaching a flexible hood on the endoscope tip and positioning it inside the duodenal bulb. Then, the anchor is collapsed by grabbing one of the proximal drawstrings using a custom grasper
The collapsed anchor is then withdrawn into the protective hood, and the entire device withdrawn from the GI tract along with removal of the endoscope [4] (Fig. 18.10). A second-look confirms that there is no active bleeding or damage to the mucosa or perforation of the duodenal bulb, stomach, and esophagus