Fig. 4.1
(a) White light endoscopic image of normal esophageal epithelium. (b) Superficial squamous cell carcinoma of the esophagus (type 0–IIa). (c) Advanced esophageal squamous cell carcinoma (type 2). (d) Obstruction due to advanced esophageal cancer (type 3)
The macroscopic findings of endoscopy are very important for understanding the location, shape, and extent of ESCC, because these parameters are usually used for making decisions about treatment. The distance of the tumor from the incisor teeth is usually measured by endoscopy. The Japanese Classification of Esophageal Cancer classifies the macroscopic tumor type into six categories (types 0–5, Table 4.1, Fig. 4.2) [2]. Tumor is defined as type 0 and recognized as superficial when the invasion is limited to the submucosa. Superficial (type 0) ESCC is divided into three subtypes (0–I, 0–II, and 0–III). When the tumor invasion extends to the muscularis propria or beyond, the tumor is classified as advanced. Advanced ESCC is divided into four categories (types 1, 2, 3, and 4). When a tumor cannot be classified into any of the first 5 categories (types 0–4), it is classified as type 5.
Table 4.1
Macroscopic classification of esophageal squamous cell carcinoma
Macroscopic classification | Macroscopic subclassification | Endoscopic feature | Detailed explanation |
|---|---|---|---|
Type 0 | Superficial type | ||
Type 0–I | Superficial and protruding type | Definitely protruding lesion | |
Type 0–IIa | Slightly elevated type | Lesion with a slight elevation up to about 1 mm in height | |
Type 0–IIb | Flat type | Lesion with macroscopic elevation or depression | |
Type 0–IIc | Slightly depressed type | Lesion with a slight depression. The degree of depression is equivalent to erosion | |
Type 0–III | Superficial and depressed type | Lesion showing more distinct depression than the type Iic, and the bottom of the depression appears to extend beyond the muscularis mucosa | |
Type 1 | Protruding type | Localized protruding type | |
Type 2 | Ulcerative and localized type | The ulcerative lesion has a well-demarcated ridge | |
Type 3 | Ulcerative and infiltrating type | The ulcerative lesion has a ill-demarcated ridge circumferentially or semi-circumferentially | |
Type 4 | Diffusely infiltrating type | Lesion with wide intramural invasion, and generally without conspicuous ulcer and protrusion | |
Type 5 | Unclassifiable type | The lesion with a complicated macroscopic appearance which is unclassifiable to any of macroscopic types 0–4 | |
Type 5a | The unclassifiable lesion without previous treatment | ||
Type 5b | The lesion unclassifiable because of a changed appearance with previous treatment |
4.2 Endoscopic Detection and Differential Diagnosis of Superficial ESCC
Detection of advanced ESCC by endoscopy is easy. However, early detection of superficial ESCC is not always easy even for experienced endoscopists, because the endoscopic changes are minimal. Therefore, an ideal strategy for the early detection of ESCC is required.
4.2.1 Conventional White Light Imaging
Conventional white light images (WLI) of superficial ESCC show disappearance of the vascular network in the mucosa (Fig. 4.3a) and/or an uneven surface with a thin white coating (Fig. 4.3b) or a reddish color change (Fig. 4.3c). The presence of these features in a suspected lesion indicates the possible presence of superficial ESCC.


Fig. 4.3
(a) Superficial esophageal cancer (type 0–IIc) is clearly identified by disappearance of vascular network. (b) Superficial esophageal cancer (type 0–IIb) shows uneven surface with a thin white coating. (c) Superficial esophageal cancer (type 0–IIa) is identified as slight reddish lesion
4.2.2 Lugol Chromoendoscopy
Iodine solution (Lugol solution) stains nonneoplastic esophageal squamous epithelium dark brown (Fig. 4.4a). In contrast, neoplastic lesions do not stain (Fig. 4.4b) [3]. Thus, Lugol chromoendoscopy is a useful method for detecting and identifying the lateral extension of ESCC. However, it causes unpleasant side effects including chest pain and discomfort in those who undergo endoscopic examination and occasionally causes allergic reactions including flushing, asthma, and iodine shock. Sodium thiosulfate solution is useful in reducing these adverse symptoms. Intravenous administration of steroids before examination is sometimes effective in preventing allergic reactions.
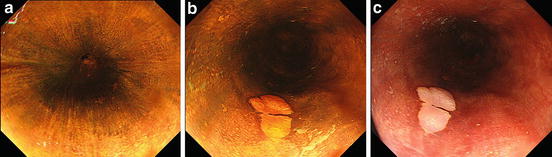
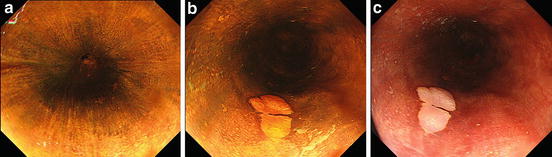
Fig. 4.4
(a) Normal esophageal epithelium is stained as dark brown by Lugol chromoendoscopy. (b) Cancerous lesion is clearly revealed as Lugol-voiding lesion after Lugol staining. (c) Definite cancerous lesion shows pink color change after Lugol staining
After staining with Lugol solution, superficial ESCC shows a pink color change (Fig. 4.4c). Shimizu et al. [4] reported that when used as a diagnostic index for high-grade intraepithelial squamous neoplasia and SCC, the pink color sign has sensitivity and specificity of 91.9 and 94.0 %, respectively. Ishihara et al. [5] also reported that its sensitivity and specificity for diagnosis of high-grade intraepithelial neoplasia or invasive cancer were 88 and 95 %, respectively.
In some cases, multiple Lugol-voiding lesions (multiple LVLs) could be detected in the entire esophagus (Fig. 4.5) [6, 7]. This phenomenon was explained by the “field carcinogenesis” theory [8], in which multiple neoplastic lesions develop not only in the esophagus but also in the head and neck region and lung and so on. The patients with multiple LVL in the background esophageal mucosa are at risk of multiple cancers in the upper aerodigestive tract.
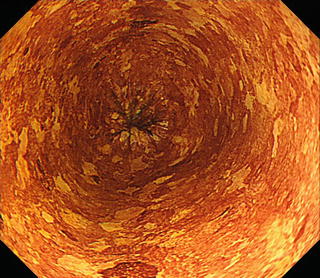
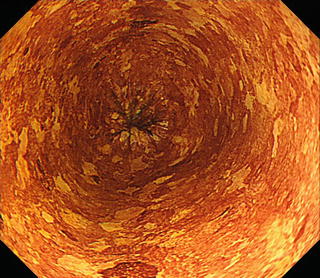
Fig. 4.5
Multiple Lugol-voiding lesions (multiple LVLs)
4.2.3 Equipment-Based Image-Enhanced Endoscopy (IEE)
Equipment-based IEE can accurately diagnose high-grade intraepithelial neoplasia and superficial ESCC with minimal invasion of the esophagus.
Among the types of equipment-based IEE, narrow-band imaging (NBI) [9, 10] has been found to provide a highly accurate diagnosis of superficial ESCC. The NBI system uses two narrow-band wavelengths of 415 and 540 nm, corresponding to the peaks of absorption of hemoglobin. Therefore, thin blood vessels such as capillaries in the epithelium or mucosal layer can be seen more distinctly by NBI than by conventional WLI. Under NBI observation, most of the area of a superficial ESCC is seen as brownish (Fig. 4.6a, b) [11, 12]. In addition, the morphological changes of the intrapapillary capillary loop (IPCL) have been recognized as a useful parameter for ESCC diagnosis and for evaluation of depth of invasion of ESCC [13]. With magnification, irregularities in the IPCL are also more clearly identified by NBI than by conventional WLI (Fig. 4.6c, d) [11, 12].
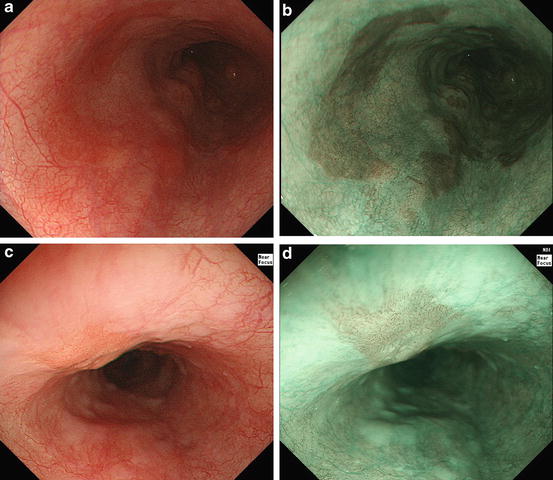




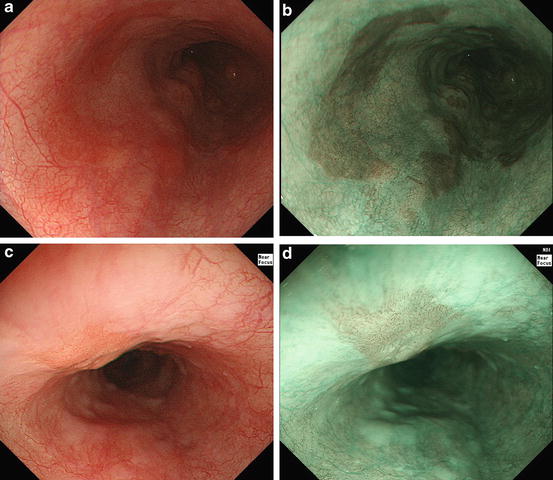
Fig. 4.6
(a) Slight reddish color changed is identified but its margin is unclear. (b) Well-demarcated brownish area is clearly identified. (c) Magnifying white light images shows irregular microvascular pattern. (d) Narrow-band image enhanced the irregular microvascular pattern compared to conventional white light image
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree