The definitions of the T, N, and M categories correspond to the FIGO stages. Both systems are included for comparison. The classification applies to endometrial carcinomas and carcinosarcomas (malignant mixed mesodermal tumours). There should be histological verification with subdivision by histological type and grading of the carcinomas. The diagnosis should be based on examination of specimens taken by endometrial biopsy. The FIGO stages are based on surgical staging. TNM stages are based on clinical and/or pathological classification. The regional lymph nodes are the pelvic (hypogastric [obturator, internal iliac] (3), common (5) and external (4) iliac, parametrial (2), and sacral (6)) and the para‐aortic nodes (7). Notes 2Positive cytology has to be reported separately without changing the stage. 3The presence of bullous oedema is not sufficient evidence to classify as T4. The pT and pN categories correspond to the T and N categories. Note
UTERUS ENDOMETRIUM (ICD‐O‐3 C54.0, 1, 3, 8, 9, C55)
Rules for Classification
Anatomical Subsites (Fig. 424)
Regional Lymph Nodes (Fig. 425)
TNM Clinical Classification
T – Primary Tumour
TNM
Categories
FIGO Stages
Definition
TX
Primary tumour cannot be assessed
T0
No evidence of primary tumour
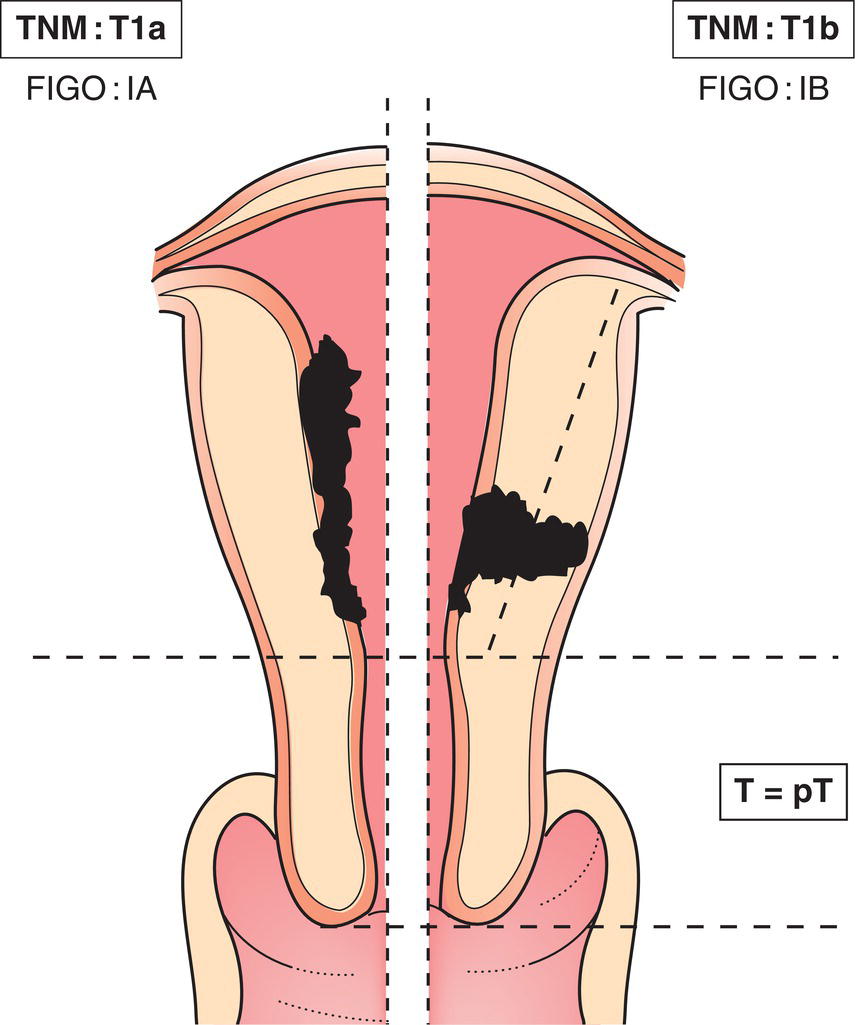
T1
I*
Tumour confined to the corpus uteri1 (Fig. 437)
T1a
IA*
Tumour limited to the endometrium or invading less than half of myometrium
T1b
IB
Tumour invades one half or more of myometrium
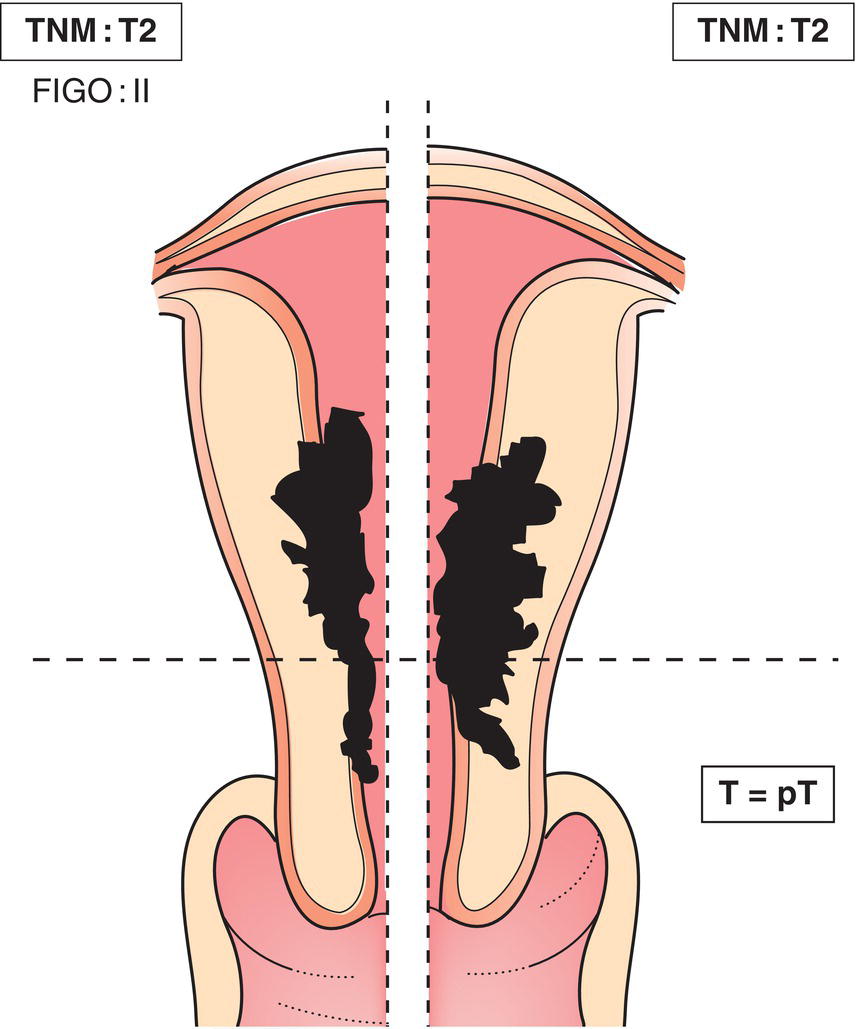
T2
II
Tumour invades cervical stroma, but does not extend beyond the uterus2 (Fig. 438)
T3
III
Local and/or regional spread as specified below
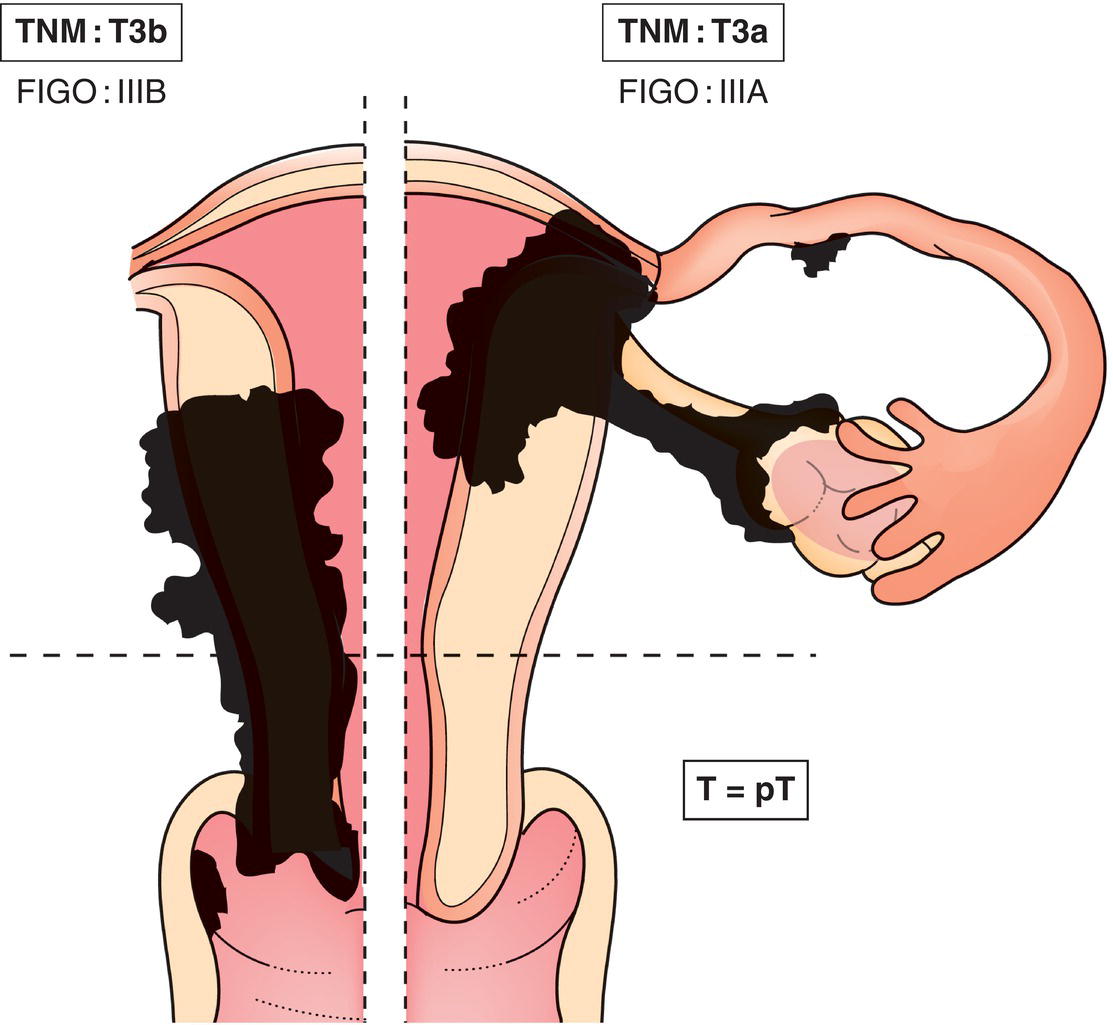
T3a
IIIA
Tumour invades the serosa of the corpus uteri or adnexae (direct extension or metastasis) (Fig. 439)
T3b
IIIB
Vaginal or parametrial involvement (direct extension or metastasis) (Fig. 439)
N1
IIIC
Metastasis to pelvic or para‐aortic lymph nodes (Fig. 441)
IIIC1
Metastasis to pelvic lymph nodes
IIIC2
Metastasis to para‐aortic lymph nodes with or without metastasis to pelvic lymph nodes
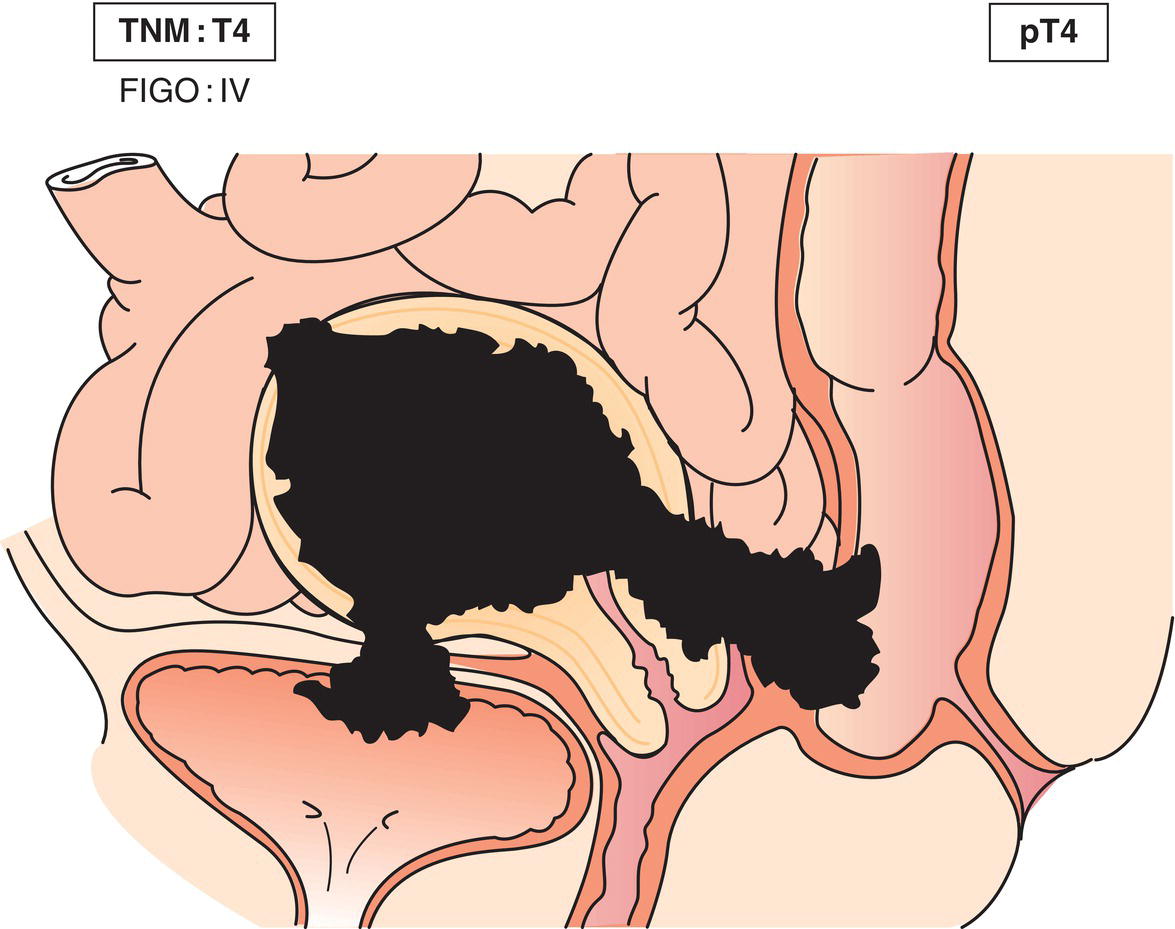
T4M1
IVAIVB
Tumour invades bladder/bowel mucosa3 (Fig. 440)Distant metastasis
1Endocervical glandular involvement only should now be considered as stage I.
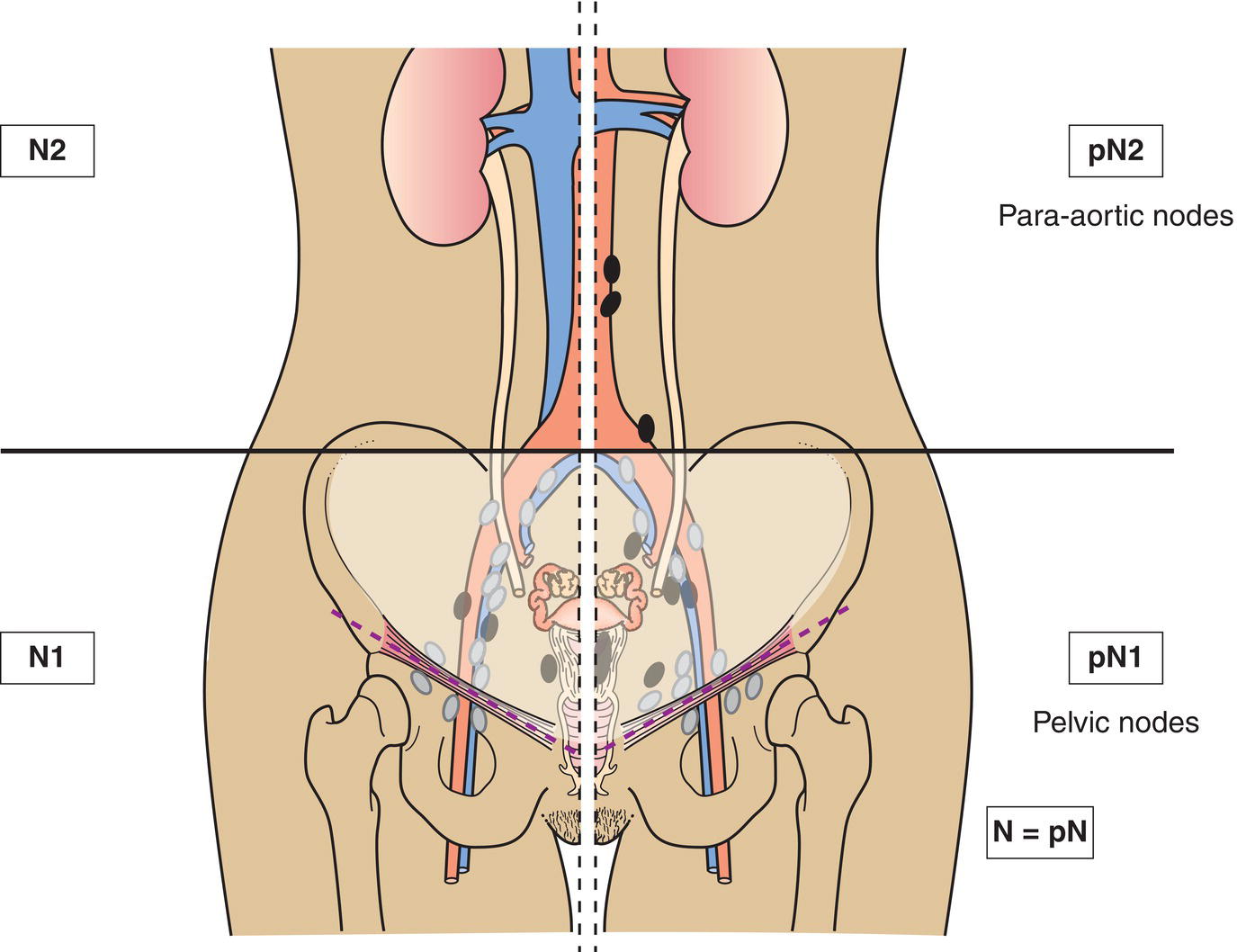
N – Regional Lymph Nodes
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
N1
Pelvic lymph node metastasis
N2
Para‐aortic lymph node metastasis
M – Distant Metastasis
M0
No distant metastasis
M1
Distant metastasis (excluding metastasis to vagina, pelvic serosa, or adnexa, including metastasis to inguinal lymph nodes, intra‐abdominal lymph nodes other than para‐aortic or pelvic nodes)
pTNM Pathological Classification
pM1
Distant metastasis microscopically confirmed
pM0 and pMX are not valid categories.
pN0
Histological examination of a pelvic lymphadenectomy specimen will ordinarily include 6 or more lymph nodes. If the lymph nodes are negative, but the number ordinarily examined is not met, classify as pN0.
Summary
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree