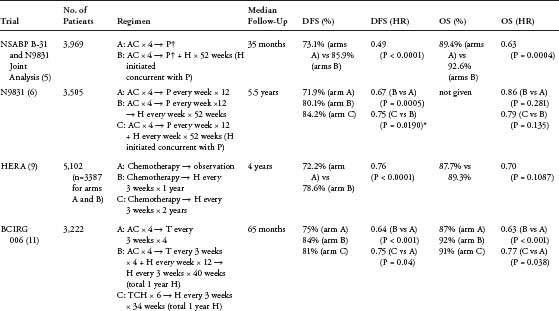
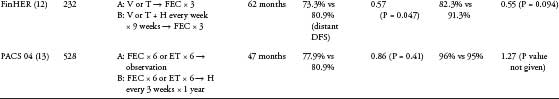
Endocrine Therapy for Early Breast Cancer Breast cancer is the most common nonskin malignancy diagnosed in women worldwide. The majority of patients with early-stage breast cancer present with hormone receptor-positive disease, and almost all of these women are offered some form of adjuvant endocrine therapy. Traditionally, tamoxifen, a selective estrogen receptor modulator, was the mainstay of adjuvant endocrine therapy in both pre- and postmenopausal women; however, recently reported large, randomized clinical trials have led to aromatase inhibitors replacing tamoxifen monotherapy for the adjuvant treatment of postmenopausal women. Questions remain as to the ideal strategy for incorporating aromatase inhibitors into the adjuvant therapy of postmenopausal women. Although 5 years of tamoxifen remains the standard for premenopausal women, there are also questions as to the role of ovarian ablation or suppression and aromatase inhibitors in designing the optimal adjuvant endocrine regimen. This article will examine the issues regarding the optimal approach to endocrine therapy in both pre- and postmenopausal women. Keywords: breast cancer, endocrine therapy, hormone receptor, estrogen receptor, adjuvant therapy Breast cancer is the most common nonskin malignancy diagnosed in women worldwide. In 2009, 192,370 new cases of invasive breast cancer were estimated to occur among women in the United States (1). As a result of improvements in early detection as well as incremental advances in adjuvant therapy, breast cancer-related mortality has declined in recent years (2). Approximately three-quarters of all patients with invasive breast cancer present with hormone receptor-positive (HR-positive) disease and almost all of these women are offered adjuvant endocrine therapy (3). In the past, tamoxifen, a selective estrogen receptor (ER) modulator, was the mainstay of adjuvant endocrine therapy in both pre- and postmenopausal women. As a result of recently reported large, randomized clinical trials, aromatase inhibitors (AIs) have replaced tamoxifen monotherapy for the adjuvant treatment of postmenopausal women. However, controversies still exist as to the optimal adjuvant endocrine regimen for both pre- and postmenopausal women. Tamoxifen A misconception that adjuvant endocrine therapy does not benefit premenopausal women was perpetuated in the past by data confounded by multiple factors including short-term tamoxifen use, the indirect endocrine effects of cytotoxic chemo-therapy, as well as the inclusion of mixed populations of HR-positive and -negative patients. The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) overview analysis clearly demonstrates that 5 years of adjuvant tamoxifen confers a survival benefit for HR-positive patients regardless of age (2). This finding led to the current standard of 5 years of tamoxifen for the adjuvant therapy of premenopausal, HR-positive breast cancer. Tamoxifen is a prodrug which must undergo extensive biotransformation into active and inactive metabolites. Several cytochrome P450 (CYP450) enzymes, including CYP2B6, CYP2B8, CYP2C8, CYP2C9, CYP2C19, CYP2C26, CYP3A4, and CYP3A5, are responsible for this in vivo conversion (4). Two minor metabolites, 4-hydroxy-tamoxifen and endoxifen (4-hydroxy-N-desmethyl-tamo -xifen), have an almost 100-fold higher affinity for the ER compared with tamoxifen (5, 6) In patients taking tamoxifen, endoxifen is detected at a 6-to 12-fold higher concentration than 4-hydroxytamoxifen, suggesting that endoxifen may be the most important metabolite for tamoxifen efficacy (7). All of the secondary metabolites except endoxifen are formed by CYP3A4/5. Endoxifen formation is almost completely dependent on CYP2D6 enzymatic activity (8). Numerous allelic variants of CYP2D6 have been described, and their incidence varies with race and ethnicity (9). The wild-type allele is designated CYP2D6*1. Variant alleles can result in enzyme production that is hyperactive or under-active, and individuals can be classified based on CY2D6 activity. People who are homologous for alleles that produce enzymes with normal activity, such as the wild-type allele, are designated as extensive metabolizers. Those who carry multiple copies of CYP2D6 alleles have high enzyme activity and are designated as ultrarapid metabolizers. People with one or two variant alleles with reduced or null activity are designated as intermediate or poor metabolizers (10, 11). Although prospective data are currently lacking, there are retrospective data suggesting that CYP2D6 polymorphisms, particularly the presence of two null alleles, lead to altered tamoxifen metabolism and potentially worse outcomes compared with extensive metabolizers (12). At the present time, routine testing for CYP2D6 prior to tamoxifen initiation in all patients is not standard practice, and current guidelines of the National Comprehensive Cancer Network Breast Cancer Panel discourage testing (13). Many of the selective serotonin reuptake inhibitors are either moderate (sertraline, duloxetine) or strong (paroxetine, fluoxetine, buproprion) inhibitors of the CYP2D6 enzyme (14). Similar to the situation with CYP2D6 alleles, although prospective data are lacking, there are retrospective data suggesting that concomitant use of strong or moderate inhibitors can lead to reduced levels of endoxifen and potentially decreased efficacy of tamoxifen (12). Because there are other commercially available agents that appear to have minimal impact on tamoxifen metabolism, such as venlaflaxine or citalopram, it is recommended to avoid concomitant use of tamoxifen with strong and moderate inhibitors of CYP2D6 enzyme. Tamoxifen has both antagonistic and agonistic effects, depending on the tissue involved which result in both adverse and beneficial side effects. In postmenopausal women, tamoxifen results in increased bone density (15, 16). In addition, tamoxifen has a beneficial effect on lipids, lowering low-density lipoproteins. It also lowers fibrinogen, homocysteine, and lipoprotein A, which may lead to an overall improved cardiovascular risk profile (17–19). Unfortunately, tamoxifen use is also associated with an increased risk of endometrial carcinomas and sarcomas, particularly in women older than 50 years (20, 21), as well as an increased risk of thromboembolic events (20). When tamoxifen is administered to a patient also receiving adjuvant chemotherapy, it is preferentially administered in a sequential fashion (chemotherapy followed by tamoxifen) based on the results of a phase III trial in which 1,588 postmenopausal women with HR-positive, node-positive breast cancer were randomized to one of three arms: tamoxifen alone; chemotherapy with cyclophosphamide, doxorubicin, and 5-fluorouracil (CAF) plus concurrent tamoxifen (CAFT); or CAF followed by tamoxifen (CAF-T) (22). Although not statistically significant, the adjusted HRs favor CAF-T over CAFT in both disease-free survival (DFS) and overall survival (OS). Multiple trials have compared varying durations of tamoxifen therapy, mostly in postmenopausal women. Trials comparing 5 years to 2 years of tamoxifen have generally favored the longer therapy arm (23, 24). Trials of longer than 5 years of tamoxifen have produced less consistent results. Although a small Eastern Cooperative Oncology Group pilot trial appeared to suggest a benefit for tamoxifen past 5 years (25) , the National Surgical Adjuvant Breast And Bowel Project (NSABP) B-14 as well as a Scottish trial did not demonstrate a benefit (26, 27). In the NSABP B-14 trial of women with HR-positive, node-negative breast cancer, there was actually a slight advantage for those patients who stopped tamoxifen at 5 years compared with those who continued tamoxifen (DFS = 82% vs 78%, P = .03, and OS = 94% vs 91%, P = .07). In contrast, recent data from the Adjuvant Tamoxifen, Longer Against Shorter trial and the Adjuvant Tamoxifen-To Offer More trial (28, 29), suggest a benefit for longer durations. Definitive reports of these two trials are currently pending. Ovarian Ablation or Suppression Multiple strategies exist to temporarily or permanently stop ovarian function in premenopausal women. Ovarian ablation (OA) techniques, such as oophorectomy or ovarian radiation, permanently eliminate ovarian function, whereas ovarian suppression techniques temporarily stop ovarian function, typically with the use of luteinizing hormone-releasing hormone (LHRH) analogues. Chronic administration of LHRH analogues, such as goserelin, disrupts the hypothalamic–pituitary– ovarian axis by binding to pituitary LHRH receptors, resulting in subsequent downregulation and desensitization of the receptors. These agents therefore lead to a “flare phenomenon” in which gonadotropin and estrogen levels initially increase, followed by their subsequent suppression to post-menopausal levels within 2 to 3 weeks (30). The major advantage of LHRH analogues compared with oophorectomy is reversibility which allows for preservation of fertility as well as potential limitation of the short and long-term adverse effects of menopause. There are limited comparative data regarding the efficacy of the various OA/OS techniques, and what are available are evaluations in the metastatic setting. A multicenter, randomized trial of goserelin versus surgical oophorectomy in premenopausal patients with HR-positive breast cancer was terminated prematurely because of poor accrual (31). With a total of 136 patients randomized, a similar failure-free survival and OS were observed, and a moderate advantage for ovariectomy could not be ruled out because of the small numbers. Using a 2 × 2 factorial design, Boccardo et al. (32) randomized 85 perimenopausal patients with HR-positive or unknown breast cancer to one of the following: surgical castration (or ovarian irradiation); goserelin; surgical castration (or ovarian irradiation) plus tamoxifen; or goserelin plus tamoxifen (GT). Although there were no significant differences in response, there was a trend favoring oophorectomy alone. Of note, tamoxifen appeared to improve the efficacy of goserelin, but not oophorectomy.Interpretation of these data is limited by a lack of power in addition to the inclusion of HR-unknown patients. At present, there are no comparative data in the adjuvant setting, and current adjuvant trial designs generally assume equivalence among the approaches. Similar to the tamoxifen data, interpretation of most of the adjuvant OS/OA trials is limited by the indirect endocrine effects of cytotoxic chemotherapy, the inclusion of mixed populations of HR-positive and -negative patients, a lack of tamoxifen in the chemotherapy arms, and a lack of an anthracycline in the chemotherapy regimens in the majority of the trials. Taxanes were not included in any of the trials. Ovarian Suppression as a Substitute for Chemotherapy Multiple trials have addressed the role of OA as a substitute for cytotoxic chemotherapy in premenopausal women with HR-positive breast cancer. In 1995, the EBCTCG published a meta-analysis evaluating the benefits of OA (33). It included eight trials with a total of 3,456 women younger than 50 years who did not receive adjuvant chemotherapy and demonstrated a clear benefit of OA with a relative reduction of 25% in the risk of recurrence and 24% in mortality compared with no adjuvant treatment. The most recent EBCTCG meta-analysis shows similar benefits for OA (2). A subsequent meta-analysis specifically examining the use of LHRH agonists has also been conducted which included 338 women and a comparison of LHRH agonists with no treatment. Among this group, a nonsignificant relative reduction in the risk of recurrence (28.4%; P = .08) and death after recurrence (17.8%; P = .49) was observed (34). Numerous studies directly comparing OA/ OS, with and without the use of tamoxifen, to chemotherapy have been performed. Six trials (the Takeda Adjuvant Breast Cancer Study with Leuprolide Acetate [TABLE] trial, a Scottish trial, the International Breast Cancer Study Group [IBCSG] VIII trial, the Zoladex Early Breast Cancer Research Association [ZEBRA] trial, a Scandinavian trial, and the German Adjuvant Breast Cancer Group [GABG] IV-A-93 trial) have compared OA/OS alone with cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) chemo-therapy alone and demonstrated similar outcomes for OA/OS and chemotherapy for patients with HR-positive disease. OA/OS is inferior to CMF in patients with HR-negative tumors. The TABLE trial randomized 589 premenopausal women with HR-positive or unknown, node-positive breast cancer to 2 years of OS with leuprolin acetate or six cycles of CMF (35). The first interim analysis of 227 patients did not reveal any differences in recurrence-free survival (RFS) or OS. A Scottish trial randomized 332 premenopausal women with stage II breast cancer to OA or CMF chemotherapy, each with or without prednisolone for 5 years (36). Although there was no difference in survival for OA compared with chemotherapy in the total group, there was a statistically significant interaction between the ER score by immunohistochemistry and treatment (P = .001) with OA being superior in ER-positive patients and inferior in ER-negative patients. The IBCSG VIII trial randomized 1063 pre-and perimenopausal patients with lymph node-negative breast cancer to goserelin for 24 months, six cycles of CMF, or six cycles of CMF followed by 18 months of goserelin (37). For the ER-positive patients, goserelin alone and CMF alone provided similar DFS (5-year DFS for both groups = 81%), whereas patients with ER-negative disease had a better DFS with CMF (88% vs 73%). Sequential therapy in the ER-positive patients led to a nonsignificant improvement in DFS compared with either therapy alone (86% vs 81%), primarily because of results in younger women (<40 years of age). The ZEBRA trial randomized 1640 pre- or perimenopausal women with lymph node-positive breast cancer to goserelin for 2 years or six cycles of CMF chemotherapy (38). After a median follow-up of more than 7 years, equivalent DFS and OS was demonstrated for the two arms. Permanent amenorrhea was noted in 65% of the patients who received CMF. The Scandinavian trial randomized 762 premonopausal patients with ER-positive tumors that were either node-positive or had a tumor size > 5 cm to OA by irradiation or nine cycles of CMF (39). There was no difference between the two groups in DFS or OS. Finally, the GABG IV-A trial randomized 771 premenopausal women with ER-positive, lymph node-negative breast cancer to goserelin for 2 years or three cycles of CMF (40). No significant difference between the two arms was detected. A total of four trials have evaluated combination endocrine therapy with tamoxifen plus OA/ OS to chemotherapy alone. Unfortunately, no trial has compared combined endocrine therapy with chemotherapy plus tamoxifen. The Breast Cancer Adjuvant Chemo-Hormone Therapy Cooperative Group trial randomized 120 pre- or perimenopausal women with HR-positive breast cancer to 5 years of OA/OS with tamoxifen or six cycles of CMF (41). There was no significant difference in DFS or OS between the two groups. The Austrian Breast and Colorectal Cancer Study Group (ABCSG) trial 5 randomized 1,034 premenopausal women with HR-positive breast cancer to 3 years of OA/OS plus 5 years of tamoxifen or six cycles of CMF (42). There was a significant difference in RFS (81% vs 76%, P = .037) and local recurrences (4.7% vs 8.0%, P = .015) and a trend toward a difference in OS, all favoring the combined endocrine therapy arm. The French Adjuvant Study Group 06 trial randomized 333 premenopausal women with HR-positive breast cancer with one to three positive lymph nodes to receive either 3 years of triptorelin plus tamoxifen or six cycles of 5-fluorouracil, epirubicin, and cyclophosphamide (FEC50) (43). There was no significant difference in DFS or OS between the two groups. Similar to the ZEBRA trial, amenorrhea occurred in 64% of the patients treated with FEC50. Amenorrhea was temporary in 58% of patients after endocrine therapy and in 31% after chemotherapy. Similarly, a smaller French trial randomized 162 premenopausal women to OA with surgery or radiation plus tamoxifen or six cycles of 5-fluorouracil, doxorubicin, and cyclophosphamide (FAC) demonstrating a significant improvement in DFS and a trend toward improvement in OS with endocrine therapy (44). There was an imbalance in the treatment arms with more patients with greater than 10 positive nodes in the chemotherapy arms. When adjusted for the number of positive nodes, there was no longer a significant DFS difference. Ovarian Suppression Following Adjuvant Chemotherapy Depending on the regimen used, permanent or temporary amenorrhea is a relatively common consequence of adjuvant chemotherapy and likely contributes to its efficacy in premenopausal women. Very young women are less likely to develop permanent amenorrhea following adjuvant chemotherapy (45). Furthermore, data suggest that very young women, younger than 35 years, with HR-positive tumors treated with adjuvant chemotherapy have a statistically significantly higher risk of relapse than older premenopausal patients, whereas younger and older premenopausal patients with HR-negative tumors have similar outcomes (46). These observations have led to the hypothesis that younger premenopausal women with HR-positive disease who do not develop ovarian failure after adjuvant chemotherapy may benefit from OS/OA. In addition to the IBCSG trial VIII discussed earlier, which did not demonstrate a benefit to OA/OS after chemotherapy, multiple other trials have conducted to evaluate the benefit of OA/OS following adjuvant chemotherapy. The Gruppo Oncologico Centro-Sud-Isole used a 2 × 2 factorial design to randomize 466 premenopausal women with node-positive breast cancer to one of four treatment arms: CMF for six cycles; doxorubicin for four cycles followed by CMF for six cycles; CMF for six cycles followed by GT for 2 years; doxorubicin for four cycles followed by CMF for six cycles followed by GT for 2 years (47). At a median follow-up of 72 months, the addition of GT to chemotherapy led to a significant improvement in DFS and a nonsignificant improvement in OS. Although the trial was not powered to detect a difference between the four arms, there was a trend favoring the anthracycline, CMF, and GT arm. A large American Intergroup trial, INT 0101 (E5188), randomized 1504 premenopausal, HR-positive, node-positive women to receive CAF alone, CAF plus 5 years of monthly goserelin (CAF-Z), or CAF plus 5 years of tamoxifen and monthly goserelin (CAF-ZT) (48). Unfortunately, as tamoxifen use in premenopausal women was not standard practice at the time of the study design, there was no arm of CAF plus tamoxifen without goserelin. With a median follow-up of 9.6 years, there was a significant benefit for the addition of tamoxifen to CAF-Z in time to recurrence and DFS, but not OS. There was no benefit for the addition of goserelin to CAF. An exploratory subset analysis in the CAF followed by goserelin arm showed a nonsignificant trend favoring the addition of goserelin to CAF in women younger than 40 years, but not for women older than 40 years. A French trial randomized 926 premenopausal women to adjuvant chemotherapy alone (choice of regimen at the discretion of the investigator) or adjuvant chemotherapy plus OA/OS (49). With a median follow-up of 9.5 years, there was no difference between the groups in DFS or OS. However, similar to the American Intergroup trial, a significant benefit in DFS for the addition of OA/OS was seen in the patients younger than 40 years with HR-positive tumors. The Zoladex in Premenopausal Patients trial was a combined analysis of 2,710 node-negative and -positive women enrolled on four randomized trials (50). All patients received local therapy, and 43% of the women received chemo-therapy with either CMF or FEC. Patients were then randomized, using a 2 × 2 factorial design, to no endocrine therapy or 2 years of tamoxifen alone, goserelin alone, or the combination of goserelin and tamoxifen. Compared with no endocrine therapy, goserelin led to a significant improvement in event-free survival (EFS) and OS. Among the HR-positive patients, there was a benefit to goserelin regardless of whether chemotherapy was administered, and the largest benefit was seen in the absence of chemotherapy. The GABG IV-B-93 trial initially randomized 465 HR-negative women to goserelin or no adjuvant endocrine therapy after three cycles of CMF (for women with zero to three positive nodes) or four cycles of EC followed by three cycles of CMF (for women with four to nine positive nodes) and later enrolled 311 HR-positive patients with one to nine positive nodes (51). With a median follow-up of 4.7 years, neither the HR-negative or -positive patients appeared to benefit from goserelin. The IBCSG 11–93 trial evaluated premenopausal patients with HR-positive breast cancer to OS/OA plus tamoxifen with or without four cycles of AC or EC (52). The trial closed early with 174 randomized patients because of a low accrual rate. After 10 years of follow-up, there was no difference in DFS or OS between the two groups. The optimal adjuvant endocrine regimen for premenopausal women with HR-positive breast cancer remains an area of significant controversy and active clinical investigation. The use of OS/OA is not without potential toxicities, including weight gain, sexual dysfunction, and hot flashes. At present, OS/OA should not yet be routinely used to replace or to complement adjuvant chemotherapy. Several ongoing trials are expected to definitively address the various roles of combining chemotherapy, OS/ OA, tamoxifen, and AIs in premenopausal patients with early-stage, HR-positive breast cancer. AIs with OA/OS in Premenopausal Women AIs as single agents are contraindicated in premenopausal women and should be used with extreme caution in women with chemotherapy-induced amenorrhea (53). The addition of AIs to OA/ OS in premenopausal women has been tested in the adjuvant and metastatic setting and continues to be evaluated in ongoing adjuvant trials. Forward et al. (54) treated 19 premenopausal women with metastatic or locally advanced breast cancer with goserelin and anastrozole; all of them had previously been treated with goserelin and tamoxifen. Of the 16 patients, 12 had a clinical benefit (75%).In the adjuvant setting, the ABCSG-12 trial randomized 1,803 premenopausal women with HR-positive breast cancer to receive 3 years of GT or anstrozole with or without zoledronic acid (55). There was no significant difference in DFS or OS between the tamoxifen and anastrozole groups. At present, an AI plus OA/OS has not been compared with tamoxifen alone (without OA/OS) in the adjuvant setting. Adjuvant Endocrine Therapy in Postmenopausal Women Within the last 10 years, numerous large, randomized trials have evaluated the role of AIs in the adjuvant therapy of postmenopausal women (Table 1). These trials have utilized three different strategies: (a) monotherapy comparisons of 5 years of tamoxifen versus 5 years of an AI, (b) sequential comparisons of 5 years of tamoxifen versus 2 to 3 years of tamoxifen followed by 2 to 3 years of an AI, and (3) extended adjuvant therapy with 5 years of tamoxifen followed by 5 years of an AI. AIs Compared with Tamoxifen The Arimidex versus Tamoxifen alone or in Combination (ATAC) trial randomized 9,366 women to 5 years of tamoxifen, anstrozole, or the combination of tamoxifen and anastrozole. The primary endpoints were DFS, safety, and tolerability. The initial analysis presented with a median follow-up of 33 months demonstrated superior DFS for the anastrozole arm compared with the tamoxifen arm, 89.4% versus 87.4%, respectively (P = .013) (56). The combination arm was not significantly different from tamoxifen alone, and this arm was not included in subsequent analyses. The incidence of contralateral breast cancer was also significantly lower with anastrozole compared with tamoxifen, with an odds ratio of 0.42 (P = .007) Anastrozole was significantly better tolerated than tamoxifen with respect to hot flashes, vaginal bleeding, venous thromboembolic events, cerebrovascular events, and endometrial cancer, whereas tamoxifen was significantly better tolerated than anastrozole with respect to musculoskeletal disorders and fractures. The ATAC trial has recently been updated with 100 months of follow-up, and the benefit of anastrozole over tamoxifen is maintained (57). The DFS was significantly longer for anastrozole compared with tamoxifen with a DFS of 74.2% in the anastrozole arm and 70.1% in the tamoxifen arm. This analysis also provided the first evidence of a “carry-over” effect of AIs with the lower recurrence rate for anastrozole being retained following therapy completion. The absolute benefit of 2.8% at 5 years (P = .002) increased to 4.8% at 9 years (P = .0001). There was not a significant OS difference between tamoxifen and anastrozole. The Breast International Group (BIG) 1–98 trial was unique in that it utilized both a mono-therapy approach as well as a sequential approach in randomizing 8,028 postmenopausal women with HR-positive breast cancer to one of four arms: 5 years of tamoxifen; 5 years of letrozole; 2 years of tamoxifen followed by 3 years of letrozole; or 2 years of letrozole followed by 3 years of tamoxifen(58). The initial analysis of this trial presented in 2005 compared the two groups assigned to initial tamoxifen (4,007 women) with the two groups assigned to initial letrozole (4,003 women). At a median follow-up of 25.8 months, letrozole significantly improved DFS compared with tamoxifen, with a hazard ratio of 0.81 (P = .003). Five-year estimates of DFS were 84% for the letrozole group and 81.4% in the tamoxifen group, leading to an absolute difference of 2.6% between the two groups. This is a similar magnitude of benefit to that observed in the ATAC trial. As compared with tamoxifen, letrozole was associated with more fractures (5.7% vs 4.0%, P < .001), but fewer thromboembolic events (1.5% vs 3.5%, P < .001), less vaginal bleeding (3.3% vs 6.6%, P < .001), fewer endometrial biopsies (2.3% vs 9.1%, P < .001), and fewer invasive endometrial cancers (0.1% vs 0.3%, P = .18). A subsequent analysis performed pair-wise comparisons between each of the sequential arms and the letrozole monotherapy arm (59). With a median follow-up of 71 months, there was no significant difference in DFS for either sequential treatment compared with letrozole alone; however, there were more early relapses among the women randomized to tamoxifen followed by letrozole compared with letrozole alone. The monotherapy analysis was also updated and demonstrated a nonsignificant difference in OS favoring the letrozole arm (HR = 0.87; 95% CI, 0.75–1.02; P = .08). Following the initial analysis of the BIG 1–98 trial, investigators were informed of the treatment assignments of the randomized patients, and 25% of the patients selectively crossed over to tamoxifen (60). A subsequent analysis using the inverse probability of censor weighting indicated a significant benefit of letrozole over tamoxifen in both DFS and OS, suggesting that the selective crossover affected the results of the intent-to-treat analysis. Results of adjuvant trials with aromatase inhibitors in breast cancer
 ABSTRACT
ABSTRACT
 ADJUVANT ENDOCRINE THER APY FOR PREMENOPAUSAL WOMEN
ADJUVANT ENDOCRINE THER APY FOR PREMENOPAUSAL WOMEN
Endocrine Therapy for Early Breast Cancer
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


