Endocrine Cancers
Jaydira del Rivero
Antonio Tito Fojo
I. THYROID CARCINOMA
The incidence of thyroid cancer is rising in both men and women. The National Cancer Institute has estimated that 62,450 new cases of thyroid carcinoma are diagnosed in the United States annually, accounting for approximately 1,950 deaths. The incidence of thyroid carcinoma is now about 9 per 100,000, with approximately 2.7 to 3.1 times as many women as men affected. The peak incidence occurs at age 35 for women and age 44 for men. The incidence rates for thyroid cancer in men and women were 6.1 and 18.2 per 10,000 in the population, respectively, between 2006 and 2010. The incidence of thyroid cancer is increasing—in women at a rate >5% per year. With the mortality rate also up by one-third in the last decade, it has been argued that the increasing incidence is real and not due to better screening/detection. Thyroid carcinoma is now over twice as common in the United States as it was 10 years ago, and it is now the fifth most common cancer in U.S. women. The 5-year survival rate of all people with thyroid cancer is about 98%.
B. Etiology and prevention4
In most patients, the cause of thyroid carcinoma is unknown, but the best-established risk factor is head and neck radiation exposure during childhood for diseases such as Hodgkin lymphoma or an enlarged thymus; hereditary factors, family history of thyroid cancer, and history of goiter and/or preceding autoimmune thyroid disease are implicated in some patients as the cause of the increased risk of thyroid cancer. Autoimmune thyroid disease is more prevalent in women and this may explain why thyroid cancer is more common in women than in men. Thyroid cancer has been observed 20 to 25 years after radiation exposure among atomic bomb survivors, and in some regions of Japan the incidence of thyroid cancer in screened populations is as high as 0.1%—10-fold greater than expected on the basis of U.S. incidence rates. In cases of accidental radioisotope exposure, expeditious use of potassium iodide can block the thyroid uptake of radioactive iodine (RAI).
Some cases of thyroid cancer are associated with familial syndrome. Medullary thyroid cancer (MTC) occurs in patients with multiple endocrine neoplasia syndrome types 2A and 2B (MEN2) and in familial MTC (FMTC) and accounts for 3% to 5% of all thyroid cancer. MEN2 and FMTC are autosomal dominant syndromes caused by a germline mutation of the RET proto-oncogene that
affect 1 in 30,000 individuals. In these syndromes, prophylactic thyroidectomy should be undertaken in at-risk individuals at young ages. Somatic RET mutations also occur in approximately 50% of sporadic MTC.
affect 1 in 30,000 individuals. In these syndromes, prophylactic thyroidectomy should be undertaken in at-risk individuals at young ages. Somatic RET mutations also occur in approximately 50% of sporadic MTC.
C. Histologic types5
The most common types of thyroid carcinoma are as follows.
1. Differentiated thyroid cancer (88%)
More than 90% of all thyroid cancers are a subtype of differentiated thyroid cancer (DTC), with papillary thyroid cancer (PTC) the most common type (80% to 85%). PTC is generally unilateral but it can also be multifocal within a lobe. Histologic subtypes of PTC that have a worse prognosis include tall cell variant, columnar cell variant, and diffuse sclerosing variant. A worse prognosis is also seen with highly invasive variants of follicular cancer. The latter are characterized by extensive vascular invasion and invasion into extrathyroidal tissues or extensive tumor necrosis with many mitoses. Other poorly differentiated aggressive tumor histologies include trabecular, insular, and solid subtypes. Genetic alterations in the mitogen-activated protein kinase (MAPK) signaling pathway are found in at least 75% of PTC cases, with a BRAFV600E mutation found in approximately 45% of PTC. Activating mutations in the RAS oncogenes occur in approximately 10% of cases. RET rearrangements are found in approximately 25% and upregulation of vascular endothelial growth factor (VEGF) signaling is also common in metastatic disease.
Follicular thyroid cancer (FTC) is the second most common DTC (10% to 15%). FTC typically disseminates hematogenously, with metastasis to both lung and bone more common in advance disease. Both RAS point mutations and mutations on chromosome 3 (PAX8-PPAR mutations) have been described in FTC. Hürthle cell cancer (HCC; 3%) also referred as oxyphilic or oncocytic thyroid cancer is a histological variant of FTC that often behaves more aggressively, and has been subsumed under the FTC classification rather than being considered a unique histotype. DTCs are derived from thyroglobulin (TG)-producing follicular cells (thyrocytes), often secrete TG and are typically initially RAI responsive. Hence, TG can be used as a tumor marker in antithyroglobulin antibody-negative patients.
MTC is a calcitonin-producing tumor derived from thyroid parafollicular or C cells, which derive from the neural crest. MTC presents worldwide as part of an autosomal dominant inherited disorder with about 20% to 25% of cases and as sporadic tumor in about 75% of cases. Sporadic tumors tend to be solitary, whereas familial tumors tend to be bilateral and multifocal. Activating mutations of the RET proto-oncogene are characteristic, with germline activating RET mutations as seen in FMTC
and MEN2 a predisposing factor. MTC most often produces both immunoreactive calcitonin and carcinoembryonic antigen, and these can be used as tumor markers.
and MEN2 a predisposing factor. MTC most often produces both immunoreactive calcitonin and carcinoembryonic antigen, and these can be used as tumor markers.
3. Anaplastic thyroid cancer (2%)
Anaplastic thyroid cancer (ATC) is a rare, aggressive malignancy that accounts for 2% to 5% of all thyroid cancers. In several countries, the prevalence of ATC has decreased dramatically due in part to increased dietary iodine and better management of DTC. Furthermore, up to 50% of patients have a concurrent history of DTC. ATC patients have a median survival of 3 to 7 months and account for a significant portion of thyroid cancer deaths. Disease specific mortality is nearly 100%, with only 10% overall survival 1 year from diagnosis. As a result, improved therapies are needed. Approximately 90% will have locoregional or distant metastases at time of diagnosis; however, most deaths result primarily from systemic disease.
4. Thyroid lymphoma (5%)
Thyroid lymphomas are uncommon and represent cancers of lymphoid tissues, as discussed in Chapters 22 and 23.
5. Thyroid sarcoma (<1%)
Thyroid sarcomas are also rare and should be treated in accordance with their underlying histology, as discussed in Chapter 17.
6. Squamous cell carcinoma of the thyroid (<1%)
Rarely, squamous cell cancers arise in the thyroid; they are best treated as primary squamous cell carcinomas of the head and neck (see Chapter 6).
1. Cell types/histology
Prognosis varies by thyroid cancer subtype. PTC is the subtype with the best survival, and mixed PTC/FTCs have similar, generally favorable biologic and prognostic behaviors with less than 15% mortality at 20 years. Even patients with lung metastases have a 20-year survival rate exceeding 50% with a 10-year survival of nearly 93% to 98%. FTCs have a somewhat worse prognosis than cancers with papillary elements, with 10-year survival of 85%. Recent studies have shown that FTCs with vascular invasion have a relatively worse prognosis, whereas FTC patients without vascular invasion do almost as well as PTC patients. MTCs often occur with regional nodal and distant metastases and can occur in early stages of the disease in MTC, with 10-year survival after surgical resection of MTC at 40% to 60%. Patients with ATC have an abysmal prognosis, with a median survival of only 4 months and a historical 10% survival 1 year from diagnosis.
2. Other factors
Prognosis is worse if tumor size is >4 cm, patient age >40 years of age and/or male gender, distant metastases are present, and/or DNA content is aneuploid. DTC tends to metastasize first to
lymph nodes, then to lung, and somewhat less commonly bone, with 5-, 10-, and 15-year survivals of 53%, 38%, and 30%, respectively. Other sites of metastases in DTC include subcutaneous structures, liver, and also brain. In contrast to most other cancers, limited regional lymph node metastasis of DTC does not influence survival substantially, and radiation-induced DTC is not associated with a worse prognosis. Several systems are used to predict outcomes in DTC, including, for example, the MACIS scoring system (metastases, +3 if metastases; age, ≤39 years of age = 3.1, >40 = age in years × 0.08; completeness of resection, +1 if primary resection is incomplete; invasion, +1 if pathologically invasive; and size, 0.3 × largest dimension in centimeters) with median prognosis estimated on the basis of the total score as indicated in Table 14.1.
lymph nodes, then to lung, and somewhat less commonly bone, with 5-, 10-, and 15-year survivals of 53%, 38%, and 30%, respectively. Other sites of metastases in DTC include subcutaneous structures, liver, and also brain. In contrast to most other cancers, limited regional lymph node metastasis of DTC does not influence survival substantially, and radiation-induced DTC is not associated with a worse prognosis. Several systems are used to predict outcomes in DTC, including, for example, the MACIS scoring system (metastases, +3 if metastases; age, ≤39 years of age = 3.1, >40 = age in years × 0.08; completeness of resection, +1 if primary resection is incomplete; invasion, +1 if pathologically invasive; and size, 0.3 × largest dimension in centimeters) with median prognosis estimated on the basis of the total score as indicated in Table 14.1.
E. Diagnosis and staging
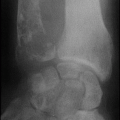
Generally, thyroid nodules >1 cm should be evaluated, since they have a greater potential to be clinically significant cancers, and neck ultrasound is an important supplemental approach. Occasionally, thyroid nodules <1 cm require evaluation because of suspicious ultrasound findings, associated with lymphadenopathy, head and neck irradiation, or a family history of thyroid cancer. Because most thyroid tumors spread primarily by local extension and regional nodal metastasis, assessment of the extent of disease in the neck is critical. With any palpable thyroid nodule, further evaluation with thyroid-stimulating hormone (TSH) and thyroid ultrasound needs to be performed. If a nodule is seen on ultrasound and TSH is normal or high, a fine needle aspiration (FNA) needs to be performed. If TSH is subnormal, a radionuclide thyroid scan should be performed either with 99mTc pertechnetate or 123I to see if it is hyperfunctioning. Hyperfunctioning nodules are benign and patients with them should be treated for hyperthyroidism. Up to 30% of FNAs are indeterminate; therefore, a definitive diagnosis is often not made until the nodule is resected. A new gene expression classification assay was able to predict benign pathology
when FNA cytology is indeterminate (e.g., BRAF, RAS, RET/PTC, Pax8-PPAR, galectin-3). If the cytology reading reports follicular neoplasm, a lobectomy or total thyroidectomy should be considered. Surgery should also be considered if the reading is reported as suspicious for PTC or Hürthle cell neoplasm. Chest radiography should be performed before surgery to rule out macroscopic pulmonary metastasis. If there is any clinical or laboratory suggestion of bone or other metastases, skeletal radiographs, computed tomography (CT) scan, positron emission tomography (PET) scan, and/or a radionuclide bone scan should be considered on a case-by-case basis.
when FNA cytology is indeterminate (e.g., BRAF, RAS, RET/PTC, Pax8-PPAR, galectin-3). If the cytology reading reports follicular neoplasm, a lobectomy or total thyroidectomy should be considered. Surgery should also be considered if the reading is reported as suspicious for PTC or Hürthle cell neoplasm. Chest radiography should be performed before surgery to rule out macroscopic pulmonary metastasis. If there is any clinical or laboratory suggestion of bone or other metastases, skeletal radiographs, computed tomography (CT) scan, positron emission tomography (PET) scan, and/or a radionuclide bone scan should be considered on a case-by-case basis.
TABLE 14.1 MACIS Prognostic Scoring System for Thyroid Cancer | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Also worthy of comment is that PET imaging should be used judiciously in thyroid cancer. In ATC, PET can be very helpful; however, some DTCs do not image well via PET. In DTC, PET avidity tends to correlate with more aggressive tumor behavior.
Patients with thyroid carcinoma are typically euthyroid; however, elevated TSH with increased thyroid peroxidase antibodies may be seen with Hashimoto thyroiditis, which may coexist in 20% of patients with thyroid lymphoma and also sometimes in DTC.
The most widely accepted tumor staging system, the TNM system, uses tumor size and extent, lymph node involvement, and distant metastasis. An ATC is considered stage IV (A, B, or C), and there are no TNM stage III or IV patients with DTC who are younger than 45 years. This staging system is suboptimal in thyroid cancer, prompting use of algorithms such as the MACIS system discussed above.13
F. Treatment
The therapeutic approaches utilized in thyroid cancer depend on the histologic type, extent of disease, patient symptoms, and rate of disease progression. Careful management of disease residing in the neck so as to protect airway, esophagus, and other critical structures is also of paramount importance.
1. Differentiated thyroid cancer14
a. Surgery. Total thyroidectomy is recommended for a DTC lesion >1 cm, taking into considering that with DTC the incidence of disease in the contralateral lobe is 20% to 87%. It is also recommended in lesions that extend beyond the thyroid, or in patients with prior exposure to ionizing radiation to the head/neck area. Further, total thyroidectomy is conducive to RAI surveillance, and simplifies follow-up in patients with high-risk disease. Total thyroidectomy with modified neck dissection is often preferred for those who have lateral cervical lymph node involvement. Unilateral lobectomy with en bloc resection of tumor maybe considered for a DTC <1 cm or follicular lesion with no evidence of multicentric disease. Mortality consequent to thyroidectomy in DTC is extremely low. Complications include recurrent laryngeal nerve damage
in 2% of patients and hypoparathyroidism that is lifelong in 1% to 2% of patients.
in 2% of patients and hypoparathyroidism that is lifelong in 1% to 2% of patients.
b. TSH suppression. TSH suppression via administration of “supra-therapeutic” levothyroxine is an essential component in the treatment of high-risk DTC, as residual cancer cells are usually initially responsive to TSH growth stimulation. Levothyroxine (T4, usual dosage range 125 to 200 µg by mouth daily) is administered to keep the TSH level suppressed below 0.1 mIU/L in high-risk (macroscopic tumor invasion, incomplete tumor resection, distant metastases) to intermediated-risk patients (microscopic invasion of tumor into the perithyroidal soft tissues, cervical lymph nodes metastases, tumor with aggressive histology or vascular invasion). For low-risk patients, the goal is to maintain TSH below the lower limit of normal 0.1 to 0.5 mIU/L. However, suppression of TSH below 0.1 mIU/L imposes long-term adverse effects on bone and can negatively impact quality of life, sometimes producing symptoms of thyrotoxicosis. Angina can also be provoked by suppressive dosages of levothyroxine, as can tachycardia or sometimes even frank cardiac arrhythmia, so care must be used in the selection of patients in whom the risks of aggressive TSH suppression is justified.
c. Adjuvant therapy/radiotherapy—RAI. Treatment with RAI is used to ablate normal residual thyroid tissue, treat micrometastases, and decrease cancer-related death as well as tumor recurrence and development of distant metastases. Destruction of residual normal thyroid tissue after thyroidectomy with RAI (131I) is termed radioactive remnant ablation (RRA). RRA is different from “RAI therapy”; in RAI therapy, larger doses of RAI are used to attempt to destroy persistent cancer, whereas RRA is used to eliminate residual normal thyroid tissue remaining after primary surgery. When ablation is carried out postoperatively, it is usually done 4 to 6 weeks after thyroidectomy. RRA allows for better subsequent imaging with RAI when looking for metastasis and also improves the utility of TG in the detection of residual thyroid cancer (as remnant thyroid tissue is destroyed). Successful remnant ablation is usually defined as an absence of visible RAI uptake on a subsequent diagnostic RAI scan or an undetectable stimulated serum TG RRA doses of 30 mCi to 100 mCi generally show similar rates of successful remnant ablation. RAI ablation is recommended for patients with known distant metastases, gross extrathyroidal extension of the tumor regardless of tumor size, primary tumor size >4 cm even in the absence of other concerning features.
Treatment with RAI (131I) is usually recommended for patients with DTC and known postoperative residual disease,
patients with distant metastases, and/or patients with locally invasive lesions. For patients with nodal metastases that are not large enough to excise, a dose of 100 to 175 mCi of RAI is commonly given. Locally invasive cancer that is not completely resected is often treated with 150 to 200 mCi of RAI while patients with distant metastasis are treated with 200 to 250 or even 300 mCi. The potential exception to this schema is lung metastasis; a dose of up to 80 mCi of RA whole body retention by dosimetry at 48 hours is generally used to avoid radiation-induced pulmonary fibrosis or empiric treatment with 100 to 200 mCi.
patients with distant metastases, and/or patients with locally invasive lesions. For patients with nodal metastases that are not large enough to excise, a dose of 100 to 175 mCi of RAI is commonly given. Locally invasive cancer that is not completely resected is often treated with 150 to 200 mCi of RAI while patients with distant metastasis are treated with 200 to 250 or even 300 mCi. The potential exception to this schema is lung metastasis; a dose of up to 80 mCi of RA whole body retention by dosimetry at 48 hours is generally used to avoid radiation-induced pulmonary fibrosis or empiric treatment with 100 to 200 mCi.
Effective and safe use of RAI treatment requires that tumor cells are capable of concentrating iodide (i.e., DTC), and appropriate patient preparation to raise TSH levels by either temporarily withholding thyroid hormone replacement or via administration of recombinant TSH. In the former situation, because of its long half-life, T4 is discontinued and T3 is initiated for a period of 6 weeks prior to the scan, with all thyroid medication withheld in the 2-week period prior to RAI administration. Ideally, a TSH level of 25 to 30 µm/mL is required for successful ablation or radiotherapy. Alternatively, recombinant TSH can be used to stimulate thyroid cell uptake of RAI in the absence of T4 withdrawal; this approach maintains better quality of life but adds considerably to expense. A low iodine diet is also required for RAI efficacy, as dietary iodine can compete with RAI for uptake in normal thyrocytes and tumor and thereby reduce RAI therapeutic efficacy. Compliance with a low iodine diet is assessed via measurement of 24-hour urinary iodine excretion.
Patients receiving high dose RAI (150 to 300 mCi) must be treated at centers with special lead-lined containment rooms, with monitoring of treated patients to assure compliance with environmental radiation safety regulations and patient and population safety. The duration of hospitalization depends on the dose given, the post-therapy method of transportation home, and contact of patient with the general public. Potential side effects of RAI include temporary bone marrow suppression (this can last weeks or even months with repeated high RAI dosage), transient nausea, sialoadenitis/dry mouth (with possible permanent cessation of salivary flow), skin reaction over the tissue concentrating the radioiodine, and pulmonary fibrosis. The use of very high cumulative RAI doses (usually when approaching 1,000 mCi) has also rarely been associated with acute myelogenous leukemia, as well as rarely with bladder and breast cancers. Scintigraphy should be performed 4 to 10 days after RAI therapy to assess uptake of RAI by tumor and to detect residual carcinoma perhaps not otherwise seen using other imaging approaches.
d. Radiotherapy—local approaches including external beam radiotherapy. External beam radiation therapy in DTC is used infrequently except as a palliative treatment for locally advanced, unresectable disease in the neck that does not concentrate iodine. External beam radiotherapy is also used for localized painful bony metastasis, for other local disease that could lead to fractures, neurological or compressive symptoms that are not amenable to surgery; for example, vertebral, CNS, or pelvic metastases, or subcarinal lymph nodes. Stereotactic radiosurgical approaches are also used in patients with recurrent cancer at previously irradiated sites and when tumors are proximal to critical radiation-sensitive tumors.
e. Systemic therapies. Several putative VEGFR inhibitors have been shown to have activity in well-differentiated thyroid cancers and two—sorafenib and lenvatinib—have received Food and Drug Administration (FDA) approval on the basis of randomized phase III trials. Sorafenib is an inhibitor of several protein tyrosine kinases (VEGFR and PDGFR) and some intracellular serine/threonine kinases (e.g., C-Raf, wild-type and mutant B-Raf). Safety and effectiveness were established in a randomized trial involving 417 participants with locally recurrent or metastatic, progressive DTC that had not responded to RAI treatment. The sorafenib dose was 400 mg twice a day. The median progression-free survival (PFS) was 10.8 months with sorafenib compared with 5.8 months with placebo (p < 0.0001). Partial responses were observed in 12.2% of patients receiving sorafenib compared with 0.5% in the placebo arm (p < 0.0001). The most common side effects with sorafenib were diarrhea, fatigue, alopecia, hand-foot skin reaction, rash, weight loss, anorexia, nausea, gastrointestinal and abdominal pains, and hypertension. TSH, a potential promoter of thyroid cancer, may increase while on sorafenib, requiring adjustment of replacement therapy. Lenvatinib is an inhibitor of the VEGF receptor 2 (VEGFR2). The approval of lenvatinib was based on a multicenter, double-blind, placebo-controlled trial that enrolled 392 patients with locally recurrent or metastatic RAI-refractory DTC and radiographic evidence of progression within 12 months prior to randomization. Patients received lenvatinib 24 mg orally per day. Median PFS was 18.3 months in the lenvatinib arm and 3.6 months in the placebo arm (p < 0.0001). Objective response rates were 65% and 2% in the lenvatinib and placebo arms, respectively. No statistically significant difference in overall survival between the two arms was demonstrated. The most common adverse reactions were hypertension, fatigue, diarrhea, arthralgia/myalgia, anorexia, weight loss, nausea, stomatitis, headache, vomiting, proteinuria, palmar-plantar
erythrodysesthesia (PPE) syndrome, abdominal pain, and dysphonia. Adverse reactions led to dose reductions in 68% of patients receiving lenvatinib and 18% of patients discontinued lenvatinib for adverse reactions. Thus, it is not clear whether the recommended dose will be tolerable, and the extent of efficacy thus remains uncertain.
erythrodysesthesia (PPE) syndrome, abdominal pain, and dysphonia. Adverse reactions led to dose reductions in 68% of patients receiving lenvatinib and 18% of patients discontinued lenvatinib for adverse reactions. Thus, it is not clear whether the recommended dose will be tolerable, and the extent of efficacy thus remains uncertain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree