3.1 Type 1 and Type 2 Diabetes Mellitus
3.1.1 Name of Disorder
Type 1 and Type 2 diabetes.
3.1.2 Clinical Definition
Type 1 diabetes is an autoimmune disease that causes the body to eventually stop producing the pancreatic hormone insulin. Type 2 diabetes is generally a result of the body becoming resistant to insulin or an inadequate insulin compensatory response.
3.1.3 How It Is Diagnosed
Clinical and laboratory studies showing elevated fasting-, postprandial-, or postglucose tolerance test glucoses. The assessment of C-peptide level and autoantibodies can help distinguish between type 1 and type 2 diabetes.
3.1.4 Nutritional Implications
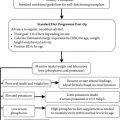
Children with diabetes follow a meal plan that is less stringent than adults because they need adequate calories, protein, vitamins, and minerals to support adequate growth. Adjusting a child’s insulin doses to a healthy, well-balanced diet is recommended as opposed to restricting carbohydrates to control blood glucose. Children with type 1 diabetes on a long-acting insulin (i.e., Lantus/Glargine) regimen and short-acting insulin (Humalog or NovoLog) regimen follow a balanced diet with carbohydrate counting. Accurate carbohydrate counting is required to determine how much short-acting insulin a child needs to cover each meal or snack. The amount of bolus insulin is determined by the child’s prescribed insulin-to-carbohydrate ratio.
3.1.5 Signs and Symptoms of Elevated Blood Glucose
- Polyuria, polydipsia, polyphagia, weight loss.
Diagnostic Parameters
- Fasting plasma glucose:
- Normal: <100 mg/dL.
- Impaired fasting glucose: 100–125 mg/dL.
- Diabetes: ≥126 mg/dL.
- 2-hour postprandial glucose:
- Normal: <140 mg/dL.
- Impaired glucose tolerance: 140–199 mg/dL.
- Diabetes: ≥200 mg/dL.
Type 1 Diabetes
Elevated blood sugar with low fasting C-peptide/insulin level and positive autoantibodies.
Type 2 Diabetes
Elevated blood sugar with high fasting C-peptide/insulin level without autoantibodies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree