Sarcomas are heterogeneous group of tumors that arise from tissues of mesenchymal origin. Current options for patients with advanced disease are limited, and only 2 drugs have been approved for these diseases over the last decade. Although several drugs are currently under development for soft-tissue sarcoma as a whole, improved understanding of sarcoma biology has led to the emergence of subtype-specific targeted therapy. This article reviews recent clinical data on emerging therapies for soft-tissue sarcoma.
Key points
- •
Despite significant progress in our understanding of the biology underlying the clinical heterogeneity of soft-tissue sarcomas (STS), only a few subtypes of sarcoma can currently be treated using rationally selected therapies.
- •
Inhibition of tumor angiogenesis has proved to be a rational target in STS, but much remains to be done to derive predictive markers.
- •
Alternative strategies to target angiogenesis are currently under evaluation in clinical trials.
- •
More work is needed to identify predictive markers not only in sarcomas but also in other solid tumors.
- •
Future trials should include pretreatment and posttreatment tumor biopsies to allow the identification of predictive factors if the drug is found to be active in a subset of patients, and to enable hypothesis-generating translational research, which will help plan the following generation of studies in STS.
Introduction
Sarcomas are heterogeneous group of tumors that arise from tissues of mesenchymal origin. As a whole they are rare tumors and account for only 1.5% of cancers, and the classification of the World Health Organization identifies more than 50 different subtypes. Molecular studies have shown these different subtypes to be biologically different, therefore suggesting that sarcomas are in fact a constellation of very rare diseases, some being even rarer than others. From the clinical perspective sarcomas are divided into soft-tissue sarcomas (STS), bone sarcomas, and gastrointestinal stromal tumors (GIST). GISTs and bone sarcomas are discussed elsewhere in this issue. This article addresses only emerging therapies for STS, although there are some areas of overlap between the 3 tumor types in terms of drug development.
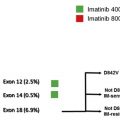
STS represent both the largest and most heterogeneous group of tumors among sarcomas. The most common subtypes include liposarcomas and leiomyosarcomas, each representing 20% of STS, but this group also includes rarer subtypes such as synovial sarcoma or even rarer entities such as alveolar soft-part sarcoma (ASPS) or epithelioid sarcoma. Although our knowledge of STS biology has grown considerably over the last few years, such progress has thus far had limited impact on patient management. Management of localized disease relies on complete surgical excision with adequate tumor-free margins followed by radiotherapy. Treatment of advanced disease is based on systemic therapy using doxorubicin, ifosfamide, dacarbazine, and trabectedin used either sequentially or in combination. Gemcitabine has also been shown to have some activity in leiomyosarcoma, either alone or combined with docetaxel or dacarbazine. Pazopanib was recently approved for the treatment of patients with advanced pretreated STS excluding liposarcoma. This review discusses emerging therapies for sarcomas, arbitrarily divided into broad-spectrum approaches for drugs or compounds that have shown clinical activity but for which the precise mode of action remains to be elucidated, and subtype-specific approaches whereby drugs are used to treat some sarcoma subtypes based on current understanding of sarcoma biology ( Fig. 1 ).
Introduction
Sarcomas are heterogeneous group of tumors that arise from tissues of mesenchymal origin. As a whole they are rare tumors and account for only 1.5% of cancers, and the classification of the World Health Organization identifies more than 50 different subtypes. Molecular studies have shown these different subtypes to be biologically different, therefore suggesting that sarcomas are in fact a constellation of very rare diseases, some being even rarer than others. From the clinical perspective sarcomas are divided into soft-tissue sarcomas (STS), bone sarcomas, and gastrointestinal stromal tumors (GIST). GISTs and bone sarcomas are discussed elsewhere in this issue. This article addresses only emerging therapies for STS, although there are some areas of overlap between the 3 tumor types in terms of drug development.
STS represent both the largest and most heterogeneous group of tumors among sarcomas. The most common subtypes include liposarcomas and leiomyosarcomas, each representing 20% of STS, but this group also includes rarer subtypes such as synovial sarcoma or even rarer entities such as alveolar soft-part sarcoma (ASPS) or epithelioid sarcoma. Although our knowledge of STS biology has grown considerably over the last few years, such progress has thus far had limited impact on patient management. Management of localized disease relies on complete surgical excision with adequate tumor-free margins followed by radiotherapy. Treatment of advanced disease is based on systemic therapy using doxorubicin, ifosfamide, dacarbazine, and trabectedin used either sequentially or in combination. Gemcitabine has also been shown to have some activity in leiomyosarcoma, either alone or combined with docetaxel or dacarbazine. Pazopanib was recently approved for the treatment of patients with advanced pretreated STS excluding liposarcoma. This review discusses emerging therapies for sarcomas, arbitrarily divided into broad-spectrum approaches for drugs or compounds that have shown clinical activity but for which the precise mode of action remains to be elucidated, and subtype-specific approaches whereby drugs are used to treat some sarcoma subtypes based on current understanding of sarcoma biology ( Fig. 1 ).
Broad-spectrum approaches
Cytotoxic Agents
Although very few cytotoxic agents remain in the development pipeline of the bigger pharmaceutical companies, several smaller pharmas are still developing “optimized” versions of older cytotoxic or newer cytotoxic agents. Several drugs are currently being developed for the treatment of advanced sarcomas, including eribulin, TH302, and INNO-206. The development of palifosfamide, a new formulation of the active metabolite of ifosfamide, one of the few drugs considered active in STS, was halted in spring 2013 following the interim analysis of a randomized phase III trial (Ziopharm press release, March 26, 2013).
Eribulin mesylate (HALAVEN and formerly E7389) is a synthetic analogue of halichondrin B, which acts as an inhibitor of microtubule dynamics. Schöffski and colleagues treated 128 patients with advanced STS with eribulin mesylate. As did previous European Organization for Research and Treatment of Cancer (EORTC) Soft Tissue and Bone Sarcoma Group studies, this phase II study comprised 4 cohorts: adipocytic sarcoma (n = 37), leiomyosarcoma (n = 40), synovial sarcoma (n = 19), and a cohort of other sarcomas (n = 32). The primary end point was 12-week progression-free survival (PFS) in each cohort (this arbitrary outcome measure is based on the work of Van Glabbeke and colleagues showing that active agents in second line provide a 12-week PFS rate of 40% or more). Fifteen of 32 (47%), 12 of 38 (32%), 4 of 19 (21%), and 5 of 26 (19%) of patients in the adipocytic, leiomyosarcoma, synovial sarcoma, and “other” sarcoma cohorts were progression-free at 12 weeks. Based on these results, a phase III trial comparing eribulin with dacarbazine is currently enrolling patients with liposarcoma and leiomyosarcoma.
TH-302 is a 2-nitroimidazole prodrug of the DNA alkylator, bromo-isophosphoramide mustard. TH-302 is designed to be activated and to release bromo-isophosphoramide mustard under conditions of severe hypoxia. In a phase I/II trial in patients with advanced STS, Ganjoo and colleagues found that TH-302 at 300 mg/m 2 could be safely administered with doxorubicin. In the phase II part of the study, 60 patients with various subtypes of advanced STS were enrolled. The response rate (RR) was 29% (17 of 58 evaluable patients) and the median PFS was 6.7 months, both of which are higher than expected for doxorubicin alone. The Sarcoma Alliance for Research through Collaboration is currently running a phase III trial of doxorubicin alone versus doxorubicin combined with TH-302 in the United States and other parts of the world.
INNO-206, or aldoxorubicin, is a doxorubicin conjugate whereby doxorubicin is attached to an acid-sensitive linker that binds covalently to cysteine-34 in circulating albumin. The proposed mechanism of action is that following intravenous injection, aldoxorubicin binds to albumin, which accumulates in tumor sites where the acidic environment will cleave the linker and release doxorubicin. The main advantage is to allow accumulation of doxorubicin in tumors while preserving normal tissues, with the aim of increasing the therapeutic index of doxorubicin. In a phase I/II trial, the maximum tolerated dose was determined to be 350 mg/m 2 . Three of 16 patients (19%) had a partial response (PR) while 10 had stable disease (SD) as their best response. Aldoxorubicin is currently being evaluated in comparison with doxorubicin as first-line chemotherapy in a randomized phase II trial.
Targeting Angiogenesis
As illustrated by the recent approval of pazopanib, inhibition of tumor angiogenesis is a viable therapeutic option in the management of STS. Sunitinib and sorafenib were evaluated in several phase II trials conducted in parallel with the initial pazopanib phase II trial conducted by the EORTC. Although 2 phase II trials failed to demonstrate significant activity for sunitinib, in the phase II trial reported by Maki and colleagues, the median PFS and the 3-month progression-free rate with sorafenib were quite similar to those found with pazopanib by the Europeans, but because of different trial designs these results were considered insufficient to declare the compound active as a single agent. Other phase II trials have since been reported and have shown similar results in terms of PFS, although the RR varied from 0% to 15%, likely reflecting disease heterogeneity. Sorafenib was also evaluated in the treatment of sarcomas combined with other treatment modalities such as chemotherapy, radiotherapy, and/or surgery. A phase I trial lead by the Grupo Espanol de Investigacion de Sarcomas reported the feasibility of ifosfamide (6 g/m 2 every 3 weeks) combined with sorafenib (400 mg twice a day), and 5 of 12 patients in this study achieved (SD) for 5 months or more. In a phase II trial, D’Adamo and colleagues tested the combination of sorafenib and dacarbazine, and observed a 10% RR and 29% clinical benefit rate (complete response [CR] + PR + SD >18 weeks) in patients with advanced synovial sarcoma and leiomyosarcoma. In this study, 4 of 4 patients with malignant peripheral nerve sheath tumors (MPNST) had progressive disease (PD) as their best response. Overall, these observations suggest that sorafenib has activity in a subset of patients with STS. However, the benefit of combining this agent with chemotherapy remains to be demonstrated. Of note, the pathologic RR seen in preoperative trials combining sorafenib with chemoradiation does not appear to differ much from that observed with chemoradiation alone. Likewise, 3 phase Ib trials (2 in Europe and 1 in Australia) are investigating the feasibility of sunitinib combined with radiation, but none of them have as yet reported any results. Aside from evaluation of these tyrosine kinase inhibitors, several studies are currently ongoing, exploring the role of bevacizumab in combination with various chemotherapy regimens as well as radiotherapy. In adult sarcoma patients, Verschraegen and colleagues recently reported the results of a phase Ib trial of bevacizumab in combination with gemcitabine and docetaxel (GD). In this trial, bevacizumab and docetaxel were given at relatively low (and fixed) doses of 5 mg/kg and 50 mg/m 2 every 2 weeks, whereas the dose of gemcitabine was increased from 1000 mg/m 2 (on day 1 every 2 weeks) by 250-mg/m 2 increments. Encouraging efficacy was seen in this study, with an RR of 31.5% (11 of 35 evaluable patients) in presumably treatment-naïve patients. A phase II trial in patients with selected advanced sarcomas (leiomyosarcoma, undifferentiated pleomorphic sarcoma, pleomorphic liposarcoma, rhabdomyosarcoma, and angiosarcoma) previously treated with zero or one previous regimen has completed accrual, while a phase III trial comparing GD with GD without bevacizumab is currently recruiting patients with advanced uterine leiomyosarcomas. Other studies are also currently ongoing in pediatric patients with advanced sarcomas. Of interest, the first phase II trial evaluating bevacizumab in STS combined doxorubicin and bevacizumab. In this study the high rate of grade 2 to 4 cardiac toxicity (6 of 17 patients) contrasted with an RR (12%) that did not seem to be different from that of the single agent doxorubicin. Studies combining bevacizumab and radiotherapy have shown promising results in terms of pathologic response.
Brivanib, a small tyrosine kinase inhibitor targeting vascular endothelial growth factor receptor (VEGFR) and fibroblast growth factor receptor (FGFR) kinases, was assessed in several tumor types in a large, multicohort phase II trial, using an independent randomized discontinuation design in each cohort. Two hundred fifty-one patients with sarcomas were enrolled in this study (leiomyosarcoma, n = 60; liposarcoma, n = 61; angiosarcoma, n = 20; other sarcomas, n = 110). One hundred thirty-three patients and 35 patients came off study for progression or other reasons, respectively, within the first 12 weeks. Seven patients (3%) had a PR and continued on open-label brivanib while 76 patients who had SD at 12 weeks were randomized. Median PFS was 2.6 months for patients in the brivanib arm versus 1.4 months in the placebo arm. This study met its primary end point for patients with FGFR2-positive tumors (median PFS 2.8 vs 1.4 months; hazard ratio = 0.58, P = .08, prespecified α of 0.1).
Other approaches targeting the tumor vasculature are currently being evaluated. One such approach is the development of vascular targeted agents using NGR peptide. NGR-hTNF is human tumor necrosis factor α targeted to the tumor vasculature using NGR peptide. Several studies have shown promising activity of this agent in combination with various chemotherapy regimens, and a phase II trial of NGR-hTNF alone or combined with doxorubicin is currently under way in unselected STS. Similarly, several studies with inhibitors of angiogenesis, either alone (axitinib, angiotensin-(1-7), pomalidomide, tivozanib, MORAb-004) or combined with chemotherapy (cisplatin + AVE8062), are ongoing or have completed accrual and await reporting.
Targeting the PI3K-Akt-mTOR Pathway and IGF1R
Numerous translational and preclinical studies have suggested an important role for the PI3K-Akt-mTOR pathway in sarcomagenesis as well as in the prognosis of STS. Of note, aside from PTEN (phosphatase and tensin homologue) loss, genetic events involving the PI3K-Akt-mTOR pathway have been found to be relatively rare in sarcomas. Barretina and colleagues reported PIK3CA mutations in 6 of 207 patients (3%), including 4 of 21 (18%) with myxoid round-cell liposarcoma. These data have provided the rationale for testing the clinical utility of inhibitors of the PI3K-Akt-mTOR pathway in patients with sarcomas. So far only rapalogs (analogue of rapamycin: ridaforolimus, temsirolimus, and sirolimus also known as rapamycin), which are inhibitors of mTORC1 (and not mTORC2), have been tested in clinical trials, and overall the results have been disappointing.
Ridaforolimus (MK8669, deforolimus, or AP23573) was assessed in a phase II study on 212 patients with advanced pretreated STS who were stratified into 4 groups: leiomyosarcoma (n = 57), bone sarcoma (n = 54), liposarcoma (n = 44), and other STS (n = 57). Ridaforolimus was administered as an intravenous infusion, 12.5 mg daily for 5 days every 2 weeks. The primary end point was clinical benefit rate (CBR), defined as CR, PR, or SD for more than 16 weeks. The CBR was 29.5% in patients with liposarcoma, 33.3% in patients with leiomyosarcoma, and 21.2% in the group with other STS. The median PFS was similar in the different cohorts, ranging from 14.3 to 16.1 weeks. No predictive biomarkers have emerged. Based on these results suggesting an essentially cytostatic effect, a randomized, placebo-controlled, phase III study (SUCCEED) evaluating ridaforolimus as maintenance therapy for patients with advanced STS who achieved SD or PR with first-, second-, or third-line chemotherapy was launched. In total, 711 patients were enrolled, 364 in the placebo arm and 347 in the ridaforolimus arm. This trial demonstrated a small but statistically significant benefit for ridaforolimus in terms of PFS (median PFS 17.7 weeks vs 14.6 weeks, P <.001), but no impact on overall survival. Moreover, the side effects were not negligible, especially stomatitis, thrombocytopenia, and pneumonitis, which occurred in 9%, 10%, and 3% of ridaforolimus-treated patients versus less than 1% each with placebo. Finally, as in many previous trials, no preselective biomarkers to assess the role of this targeted therapy were required. Merck Sharp & Dohme submitted an application for approval from the Food and Drug Administration, which was rejected.
Temsirolimus, which is approved for the management of patients with clear-cell renal cell carcinoma and mantle cell lymphoma, was evaluated in single-arm phase II trial that enrolled 41 patients. Despite the choice to perform the study in a first-line advanced disease setting, the RR was low (5%) and the median PFS was short: 2.0 months (95% confidence interval 1.8–3.5).
Activity of sirolimus was assessed in combination with metronomic oral cyclophosphamide in a single-arm, open-label, phase II trial. Forty-nine patients with advanced sarcomas (41 STS, 8 bone sarcomas) were enrolled in this study. Only 1 patient had a PR (RR 2%), and the median PFS and overall survival were 3.4 months and 10 months, respectively.
Richter and colleagues reported preliminary results of a phase II trial of everolimus in sarcomas, GIST, and ASPS. Two of 15 patients (13%) in the sarcoma cohort had SD, and no data were reported for the ASPS cohorts. However, the findings are in line with those of other rapalogs reported previously.
Based on these disappointing results the future of mTOR inhibitors in the management of STS remains uncertain. Great hope was set on combinations with chemotherapeutic agents (gemcitabine) and with other targeted agents (anti–insulin-like growth factor receptor 1 [IGF1R] monoclonal antibodies). However, here again the results reported thus far have been disappointing. Two phase Ib studies combining rapalogs and IGF1R inhibitor suggested interesting activity in sarcomas (either bone or soft tissue, or both). In one of these studies, everolimus 10 mg daily was given orally, combined with intravenous figitumumab every 3 weeks, to 21 patients. One patient with solitary fibrous tumor had a PR and 11 patients remained on study for more than 3 months. In another phase Ib study, Naing and colleagues assessed the safety profile of cixutumumab combined with temsirolimus. In this study, 2 patients with Ewing sarcoma had a CR and 3 other patients had tumor shrinkage of less than 30% per RECIST (Response Evaluation Criterion for Solid Tumors) lasting from 8 to 27 months. The most frequent drug-related adverse events were mucositis, hyperglycemia, hypercholesterolemia, and thrombocytopenia. The most recently reported study is an open-label phase II study of temsirolimus combined with the IGF1R monoclonal antibody cixutumumab (formerly IMC-A12), which was a 3-strata study: IGF1R-positive STS (arm A), IGF1R-positive bone sarcomas (arm B), and IGF1R-negative sarcomas (arm C) (bone and soft tissue). The primary objective was PFS at 12 weeks independently assessed in each cohort using a Simon 2-stage design. Four hundred eighteen patients were screened and 174 enrolled in the study: 57 in arm A, 54 in arm B, and 63 in arm C. The 12-week PFS rates were 32%, 35%, and 42% for cohorts A, B, and C, respectively, and were therefore close to the predefined threshold for activity based on the EORTC criteria. A total of 10 PRs were seen, mostly in patients with bone sarcoma (5 Ewing sarcoma, 3 osteosarcoma, and 1 chondrosarcoma), with only 1 patient with solitary fibrous tumor achieving a PR in the STS arm. Another finding of this study is that the primary chosen biomarker (ie, IGF1R expression) does not seem to predict activity in STS, although it does seem to provide some predictive information in bone sarcomas. Although this study met its primary end point, the future of IGF1R inhibitors in the management of sarcomas is uncertain, as most pharmaceutical companies have stopped the development of such compounds.
Histone Deacetylase Inhibitors
Inhibition of histone deacetylase (HDAC) provides a novel approach for cancer treatment. HDAC deacetylates histones as well as other substrates relevant to cancer therapy, including the chaperone protein HSP90 and tubulins. HDAC inhibitors were shown to have activity in preclinical models of translocation-related sarcomas (synovial sarcoma, Ewing sarcoma). The French sarcoma group (GSF/GETO) performed a single-arm phase II trial with panobinostat (formerly LBH589), a pan-HDAC inhibitor, in patients with advanced STS. In this study, 48 patients with advanced pretreated (median 2 lines of prior therapy) STS (liposarcoma, n = 11; leiomyosarcoma, n = 10; MPNST, n = 6; synovial sarcoma, n = 6) were treated with panobinostat given orally on Mondays, Wednesdays, and Fridays. One of the findings of this study was that 40 mg of panobinostat thrice a week was too toxic in this heavily pretreated patient population, and the dose had to be reduced to 20 mg after enrollment of the first 12 patients. From the efficacy standpoint, there were no PRs and only 6 patients (12.5%) were progression-free at 6 months. A study with vorinostat has completed accrual but only pharmacokinetic data from this study have yet been reported. Other studies are currently ongoing combining HDAC inhibitors with doxorubicin (PXD-101 and PCI-24781). Overall, despite very promising preclinical data, clinical results with HDAC inhibitors as single agents have been disappointing, and their development in solid tumors in general remains uncertain.
Hedgehog, Wnt, and Notch Signaling
Notch and Hedgehog (Hh) pathways play major roles in the development of pluricellular organisms. Their oncogenic role has emerged in recent decades.
The Hh pathway involves several actors: the Hh ligand, 2 transmembrane proteins called Patched (PTCH) and Smoothened (SMO), and transcription factors from the GLI family. In the absence of the Hh ligand, PTCH inhibits the activity of SMO. Binding of Hh ligand to PTCH relieves SMO from its inhibition by PTCH. Activated SMO leads to the release of activator forms of GLI, a zinc-finger transcription factor that then regulates the expression of several target genes involved in tumorigenesis. Most of the currently available Hh inhibitors are small-molecule inhibitors of SMO, although some agents currently in preclinical development target Hh ligands.
In humans, Notch signaling is based on 4 Notch receptors (1–4) and 5 ligands (Delta-Like-1, -3, and -4 [DLL-1, DLL-3, and DLL-4] and Jagged-1 and Jagged-2 [JAG1 and JAG2]). Both ligand and receptor are cell-membrane bound in this system. On ligand binding, the intracellular part of Notch (NOTCH-IC) is released and translocates to the nucleus, where it binds to the transcription factor named CSL. Release of NOTCH-IC is in part due to cleavage from the membrane by γ-secretase. Most of the Notch-signaling inhibitors currently in development are actually inhibitors of γ-secretase. Physiologically, Notch signaling is involved in maintenance of an undifferentiated state, cell-fate decision, and induction of terminal differentiation. Notch signaling has been reported to be involved in human tumors both as an oncogene and as a tumor suppressor, suggesting that its transforming potential may be dependent on context and dosage. This proposal seems to be true for sarcomas, as some reports have linked overexpression/activation of Notch signaling to a more aggressive phenotype (increased invasion and motility in rhabdomyosarcoma or proliferation in osteosarcoma) while others have shown that Notch signaling is downregulated by the EWS-FLI1 fusion protein in Ewing sarcoma, indicating a putative tumor-suppressing role for Notch in this disease.
Although activity of SMO inhibitors has been disappointing in chondrosarcoma, it is worth noting that the Hh pathway plays an important role in other sarcomas such as rhabdomyosarcoma or osteosarcoma. Furthermore, recent preclinical studies suggest that combination of Hh and Notch pathway inhibitors may be synergistic in some sarcoma subtypes displaying activation of both pathways. A phase I/II trial testing a combination of GDC-0449, an Hh inhibitor, and RO4929097, a γ-secretase inhibitor, was recently reported. In this study, 34 patients with sarcomas of varying histology were treated with fixed doses of GDC0449 and increasing doses of RO4929097. Although no PRs were noted, durable SD (>16 weeks) was seen in 4 patients (12%). Based on these findings, the investigators recommend further clinical development of the combination in sarcomas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree