15 Upon completion of this chapter, the reader will be able to: • Understand the traditional emphases of emergency department (ED) care and the efforts in progress to address the ED needs of the elderly. • Describe the differences between older adults’ and younger adults’ needs for emergency services, and how to address the more complex needs of the elderly. • Identify specific geriatric emergencies, and discuss their management, focusing especially on whether to treat on site, to transfer to the ED (and if important, which ED), or directly hospitalize. • Describe the optimal linkages between the primary care provider (PCP) and the ED or emergency physician (EP) in the transitioning of the care of specific geriatric emergencies. • Navigate your own site-specific systems-based practice area (the places where you mainly do your clinical work and the EDs and hospitals available to you), and describe your criteria for choosing—in your own region—one ED or hospital relative to another for specific geriatric emergencies. • Know your own region’s arrangements for emergency transfer to the different levels of stroke and trauma care, especially your region’s level 1 trauma center(s) and stroke center(s)] and the precise clinical criteria for their use in trauma and stroke emergencies. • Detail the identification and initial management and the potential roles of the ED in the following geriatric emergencies, and apply the same principles of selective and often urgent use of the ED to the many other conditions in this book when emergencies occur: shortness of breath especially in chronic obstructive pulmonary disease (COPD); syncope with and without risk factors; trauma especially of the head; acute stroke; sepsis; hypo- and hyperthermia. The current model of emergency care, developed by the Committee on Trauma of the American College of Surgeons in 1962, was intended to rapidly detect clear presentations of acute illness and injury requiring usually a single expedited intervention. In the ED the best care of a previously unknown patient (triage, history, physical, medication reconciliation, stabilization, laboratory testing, imaging, acute consultation, initiation of definitive treatment, documentation of evaluation and actions, a preliminary diagnosis, and disposition to the appropriate level of care) optimally occurs in minutes to under 6 hours. This system is not designed for the interwoven medical complexities, slowly evolving presentations, and convoluted social concerns that must simultaneously be addressed for optimal management of the old.1,2 The constant interruptions suffered by the EP (more than twice as many per hour as primary care physicians (PCPs) in one study) and the distraction of managing multiple patients simultaneously (more than three at a time, more than half of the time)3 underscores the difference in the orientation of the ED and primary care settings: the ED is episodic, disease (and hospital) oriented, and urgent, whereas the primary care setting tries for continuity, complexity, care in the long term, and is dominantly subacute, and—ideally—interacts a lot with services out in the community. A defining component of primary care,4 continuity of care decreased markedly from 1996–2006 in the United States. This decrease was associated with a drop in patient satisfaction, an increase in medical errors, duplication of services, unwanted treatments, polypharmacy, and decreased autonomy, and undermined quality and outcomes.5 The Institute of Medicine recommends that all participants in health care, including nursing and rehabilitation facilities, fully coordinate their activities and integrate communications; this would clearly improve elderly care.6 A study of PCPs’ and emergency physicians’ (EPs’) ability to communicate and coordinate health care discovered haphazard communication and poor coordination, and that this situation undermines effective care and results in poor patient satisfaction and duplication of testing and treatment.7 The use of hospitalists to care for admitted patients results in more direct and immediate communication at the start of the hospitalization. Efforts at coordination generally fall to the diligence and training of the professionals themselves. Such direct contact can make a life and death difference. The aging of the United States population influences all segments of health care but especially the use of the ED.8 Elders do have greater needs for emergency care than other age groups.9 Currently, 20 million older Americans utilize EDs annually.10 Studies overwhelmingly agree this high level of use by older adults is appropriate.11,12,13 The proportion of Emergency Medical Services (EMS) use in elders increases from 27% for age 65 to 84 to 48% among those 85 and older.14,15,16 Elders require more ED staff time and resources, receive more medications, and have higher rates of admission to both the hospital and critical care units.17,18 From 33% to 50% of elder ED visits result in hospitalization, which is up to 4.6 times higher than rates seen in younger adults.19,20 Older adults are likely to have a PCP. Most do consult their PCP prior to ED use and are referred to the ED by their PCP. The one exception to high ED use by older adults may be the rural setting, where there is a disproportionately lower rate of ED use by older adults.19 The strain placed by older adult utilization of already overcrowded EDs calls for a review of both the appropriateness and patterns of PCP ED referral as well as the model of ED systems of care.20,21,22 Comorbidities, polypharmacy, lack of access to care, lack of mobility, poor social support, and frailty all contribute to the vulnerability, with increased morbidity and mortality of our older patients. Fifty-one percent of “social admit” elderly patients were found to have an acute medical problem: infections in 24%; cardiovascular issues in 14%; a neurologic event in 9%; gastrointestinal problems in 7%; pulmonary problems were noted in 5%; and another 5% with fracture, anemia, acute renal failure, or uncontrolled pain.22,23 Patients sent to the ED for lack of social support suffered a 1-year mortality of up to 34%.24 In the first 3 months after an index ED visit, 5% of discharged elder ED patients will die, 20% will require hospital admission, 20% require another ED evaluation, and from 10% to 48% suffer decline in functional abilities.25,23,26 This high incidence of poor outcomes despite PCP follow-up suggests a complexity of need that far out spans the episodic ED visit.27,28 These outcomes suggest the underlying issue is not the acute event for which the ED was designed, but a quietly ongoing process. Thus a substantial proportion of elders would likely be better served in non-ED settings and with active follow up, coordinated by their PCP,29,30 who ideally should be vigilant for continued deterioration of older patients who attended the ED. This is one of six core competencies required in all physicians before they are certified to graduate by any residency program. SBP is defined by the Accreditation Council of Graduate Medical Education (ACGME) as: an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value.31,32 Seventy-one percent of the U.S. population can access a general comprehensive ED within 30 minutes, and 98% has access within 60 minutes. Access to a teaching hospital ED is more difficult, with 16% access in 30 minutes and 44% within 60 minutes.33 Such aspects can compromise the success of therapies for acute myocardial infarction, stroke, and sepsis. At least one rural study of three communities confirms that the more limited access of rural elders can be addressed using preplanned transport methods for acute emergencies, and by being well prepared to provide emergency care on site. In fact, there were probable advantages for these communities relative to nonrural settings.34 Many attempts to optimize ED care for the old have been made; chief among these are geriatric service lines and development of a geriatric ED (GED). In addition to incorporating the Affordable Care Act’s (ACA) focus on maximizing resources in the Medicare population, a further goal is to appropriately triage those requiring inpatient care, and to identify—and effectively implement—services for those who can be discharged. 35,36,37 GEDs have the following characteristics: 1. Enhanced ED staffing and administration: geriatrically trained registered nurses (RNs), pharmacists, social workers, specialist geriatricians, and care coordinators. Geriatrician ED consults have resulted in avoidance of admission for 85% of the older patients evaluated.8 Moderate improvements in the provision of physical and occupational therapy are also noted. 2. Screening: GEDs utilize screening to shift to being proactive rather than reactive. Screenings identify high risk individuals, decrease never-events, and identify need for specific services. Linkages to care for the problems identified are crucial; these generally involve primary care and community services.36 3. Case management: This is reported to improve the health, social, and service utilization outcomes arising from ED visits. Core components were reviewed as to their influence on effectiveness of interventions.37 More than eight of these key components produced a trend toward better outcomes: a validated risk stratification tool in a full geriatric assessment, significant nursing involvement in clinical evaluation, leadership roles, initiation of care and disposition planning from the ED, and having post-discharge follow-up mechanisms in place. 4. Staff education: In view of their recognized lack of geriatric-specific training,38 many training programs and curricula have been developed for EMS providers, ED nurses, and EPs.39–43 The three most common complaints in elder ED patients are: chest pain, shortness of breath, and abdominal pain.44,45 The differential of each of these obviously includes life-threatening emergencies. The most frequent medical diagnoses made in older ED patients are: ischemic heart disease, congestive heart failure, cardiac dysrhythmias, syncope, acute cerebrovascular accidents, pneumonia, abdominal disorders, dehydration, and urinary tract infections.46 Surgical emergencies in ED elders are primarily due to injuries sustained in a fall. Injuries are the seventh leading cause of death in the elder population.8 Falls are a critical event in this population (see separate chapter) with the cause being as significant as the damage, due to high recurrence rates. A is for Airway compromise, the inability to move air through the mouth, nose, and upper airway into the lungs, as seen in stridor, mucosal edema, unconsciousness, anaphylaxis, and foreign body. B is for Breathing and includes evaluation of respiratory rate. Danger exists at the extremes of <10 breaths/min or 30 and over breaths/min, or if the O2 saturation is <93% on room air. C is for Circulation and includes signs of decreased organ perfusion such as diaphoresis, new altered mental status, and cyanosis. Shock can be heralded by pulse <50 beats/min or >120 beats/min, or by a systolic BP <90 mm Hg. D has been added for (neurologic) Disability and is noted by new decreased mental status, Glasgow coma scale47 <13, or stroke-like symptoms. Exacerbations are most often triggered by a viral or bacterial infection48 but can also be triggered by cold weather, narcotic use, CHF, or anemia, among other triggers. It is essential to be able to differentiate between a mild exacerbation, which could be treated in the office, and a more severe one that requires transfer to the closest ED. The most life-threatening components of an exacerbation are hypoxemia and hypercarbia.49 Hypoxia and hypercarbia can present similarly with symptoms such as headaches, agitation, confusion, lethargy, and in severe cases, can lead to seizures or coma. Impending respiratory collapse will be manifested by the signs above plus tachypnea, tachycardia, hypertension, accessory muscle use, pursed lips, and altered mental status. The retention of CO2 heralds acute respiratory failure. The idea that oxygen can induce hypercarbia is largely a myth.50 Oxygen should not be withheld from patients with hypoxemia. However, do not apply high flow oxygen (defined as 8–10 L/min); rather titrate oxygen treatments, which reduces mortality, hypercapnia, and acidosis in acute exacerbations of COPD.51,52 Unless you can apply positive pressure or intubate the patient, maintain SpO2 between 88% and 92% as this was found to reduce mortality by 58%.53 Spirometry—to identify airflow obstruction—should be obtained in COPD patients with altered respiratory symptoms.54 • Oxygenation: Initial measurement of oxygen saturation and, if available, arterial blood gas can serve to give a quick assessment of severity of the exacerbation. • Pulmonary function tests: If patient is able to comply, obtaining a FEV1 or PEFR can help determine severity of the exacerbation. FEV1 is preferred but is rarely readily available in an acute setting. PEFR of <100 L/min, FEV1 <1 L, along with worsening function on sequential testing despite treatment, are all indicative of a severe exacerbation.49,53 • Ancillary testing: A chest x-ray can help identify underlying triggers of the exacerbation such as pneumonia or CHF. An ECG can help rule out ischemia or arrhythmias, such as multiple atrial tachycardia (MAT). Complete blood counts, electrolyte panel, and D-dimer should be performed when clinically indicated but should not be used to assess severity of a particular exacerbation. • Oxygenation: Administer O2 by nasal cannula, face mask, or by the most appropriate method. • Bronchodilators: Short-acting beta 2 agonists such as albuterol55 and anticholinergic agents such as ipratropium are both equally effective in acute COPD exacerbations and have been shown to lead to shorter stays in the ED and improved outcomes when used concomitantly.56 Long-acting beta 2 agonist or long-acting anticholinergic agents have no role in acute COPD exacerbations. • Corticosteroids: Administration of either IV or PO steroids during an exacerbation can help prevent return of symptoms after an exacerbation but do not prevent hospitalization in an acute setting. This is likely due to the onset of action of up to 6 hours from administration.57 It is prudent to give steroids to a patient who is going to be discharged from the office. There is no difference in outcome or onset of action in using IV versus PO steroids. • Antibiotics: Most common pathogens are streptococcus pneumonia, hemophilus influenza, and moraxella catarrhalis. Antibiotics should be given if concomitant infection is suspected from symptoms such as increased sputum or fever.48 • Noninvasive positive pressure ventilation (NPPV): Indicated for moderate to severe exacerbations as determined by worsening tachypnea >25 breaths/min, dyspnea with accessory muscle use, moderate to severe acidosis (pH<7.35), or hypercapnia (PaCO2 > 45mm Hg).57 If a patient is deemed to require NPPV, he/she should be transferred to the nearest ED as soon as possible. Patients in respiratory distress that undergo NPPV have better short-term mortality, decreased intubation rates, and decreased length of hospital stay.58 • Mechanical ventilation: if a patient continues to deteriorate despite all the above interventions, endotracheal intubation is the next required therapy. This should always be determined by and performed in an ED or ICU setting. The 2008 American College of Emergency Physicians Clinical Policy: Critical Issues in the Evaluation and Management of Patients Presenting With Syncope,59 recognizes the extremely low yield of non-directed testing in syncope evaluation.59 On admitted syncope patients, the most commonly performed ED studies are ECG (99%), cardiac markers (95%), and CT head (63%). Markers and CT head affected diagnosis or management in less than 5% of cases and were diagnostic in <2%.60 Although orthostatic blood pressure readings are obtained in about a third of patients, these evaluations affected diagnosis in up to 26%, management in up to 30%, and determined etiology in from 15% to 21% of patients. Obtaining an ECG and a hematocrit is warranted for most cases of syncope, with further testing normally being low yield. For suspected cardiogenic syncope, a chest x-ray and cardiac enzyme panel may be warranted. However, unless there exists a strong suspicion of neurologic cause or if head trauma is involved, a head CT is rarely warranted. Generally, purely vasovagal or orthostatic hypotension syncope (or drug induced orthostasis) with a correctable cause has no increased risk for future adverse events.49,61 If a clear etiology of the syncope cannot be determined, the patient should be risk stratified as low risk for adverse events. You should determine who can be discharged home with follow-up, who will need admission to an inpatient setting for further workup, and who requires ED intervention. Several clinical criteria and clinical decision rules (CDRs) exist to aid with risk stratification; unfortunately, there is no particular set of criteria that has been shown to be superior, and most have been proven to be inadequate to estimate risk in certain clinical settings.49,61 The San Francisco Syncope Rule62 has five predictors of adverse events: (1) history of CHF; (2) hematocrit <30; (3) ECG changes consisting of any morphologic changes not seen on prior ECG, any dysrhythmias, or nonsinus rhythm either on strip or on monitor; (4) shortness of breath by history; and (5) systolic BP < 90 mmHg. If ANY of these criteria is met, the patient is considered high risk and warrants further evaluation. These rules have shown a 96% sensitivity and 68% specificity for serious outcomes defined as death, MI, arrhythmia, PE, stroke, SAH, hemorrhage, or any condition requiring return to the ED at 7 and 30 days.3 However, the sensitivity and specificity of these rules have been shown to decrease significantly in the elder population.63 A different CDR, the OESIL score (Osservatorio Epidemiologico sulla Sincope nel Lazio), takes into account age >65, known CV disease, abnormal ECG, and lack of a presyncopal prodrome as high risk predictors—the higher the score, the higher the predicted mortality at one year. This tool had a sensitivity of 95% and specificity of 31%.64
Emergency care
Primary care and the emergency department
Epidemiology
Systems-based practice (sbp)
Access to the ED
The “geriatric emergency department” (GED)
Common emergencies in geriatrics
“the ABCs”
COPD exacerbations
Investigation
Treatment: Interventions that can be performed in an outpatient setting
Treatment: Interventions that require transfer to the closest ED
Syncope
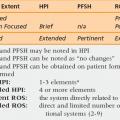
Management of syncope