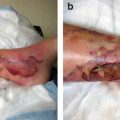
Fig. 9.1
Phases of opportunistic infections in allogeneic hematopoietic stem cell transplant recipients. NK natural killer, HHV6 human herpesvirus 6, EBV Epstein-Barr virus, PTLD posttransplant lymphoproliferative disease. [Reprinted from Tomblyn M, Chiller T, Einsele H, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: A global perspective. Biol Blood Marrow Transplant. 2009;15:1143–1238 with permission from Elsevier.]
The number of pathogens resistant to commonly used antibiotics has been increasing in both the general and nosocomial patient populations in recent years. Several factors have contributed to this increase, including the widespread use of antibiotics, increased number of immunocompromised hosts, and introduction of new antibiotics (Jones 2001). Before deciding on antimicrobial treatment, knowledge of the patient’s immune defect or defects, history of previous and recent infections, and history of recent antibiotic use is very important. Selection of the initial antimicrobial therapy should be driven by the pathogen or pathogens and their antimicrobial susceptibility.
At our institution, the treatment approach for a cancer patient with an infectious process is often a multidisciplinary one. Collaborative interaction among members of different departments and specialties, including primary oncologists, emergency room physicians, infectious disease specialists, clinical pharmacists, intensive care unit (ICU) personnel, pulmonary physicians, surgeons, interventional radiologists, and other specialists is imperative in the fight against infectious processes that can jeopardize patients’ well-being and affect the course of their cancer treatment.
Pneumonia in Patients with Cancer
Epidemiolog y
In 2005, pneumonia, along with influenza, was the eighth leading cause of death in the United States, the sixth leading cause of death in individuals over the age of 65 years, and the leading cause of death among infectious diseases. In cancer patients, the lung is a common site of infection, and pneumonia is the leading overall infectious cause of death.
Definitions
The typical pneumonia history and presentation of cough with or without sputum production, fever, dyspnea, and chest pain or examination finding of abnormal focal chest signs may or may not be present in a cancer patient who is immunocompromised. A profoundly neutropenic patient with a pulmonary infection may have minimal or no signs, symptoms, or physical findings of pneumonia or pulmonary infiltrates on chest radiographs.
Pneumonia is categorized according to four types .
1.
Hospital-acquired pneumonia (HAP): occurs 48 h or more after admission.
2.
Ventilator-associated pneumonia (VAP) : develops more than 48–72 h after endotracheal intubation.
3.
Healthcare-associated pneumonia (HCAP): develops in a patient with specific risk factors such as the following:
Hospitalization for 2 or more days within the prior 90 days
Residence in a nursing home or extended-care facility
Chronic dialysis within the last 30 days
Home wound care within the last 30 days
Home infusion therapy (including antibiotics)
Family member with multidrug-resistant (MDR) pathogen infection
Chemotherapy within the last 30 days
4.
Community-acquired pneumonia (CAP ): does not fit the criteria for HCAP, HAP, or VAP. At our institution, this may be pneumonia in a patient undergoing surveillance, an employee with no patient contact, or a visitor.
In the MD Anderson EC, 88 % of patients diagnosed with pneumonia have HCAP, whereas only 12 % have CAP. Recent chemotherapy, radiation therapy, or any other cancer therapy is considered a risk factor for HCAP. In comparison with patients with CAP, 82 % of whom receive treatment as outpatients, 89 % of patients who present with pneumonia are hospitalized.
Microbiology of Pneumonia in Cancer Patients
The spectrum of pulmonary infections in the cancer population depends on the underlying immunologic deficit or deficits. Staphylococcus aureus and S. pneumoniae are the most common Gram-positive organisms. In neutropenic patients, as neutropenia persists, infection with resistant Gram-negative bacteria (e.g., Acinetobacter, Enterobacter, and Pseudomonas species; Stenotrophomonas maltophilia) and fungi (e.g., Aspergillus, Zygomyces, and Fusarium species) can occur, especially in those with hematologic malignancies (Rolston 2001). Other organisms isolated from cancer patients’ respiratory specimens include mycobacteria (mostly nontuberculous); Legionella, Candida, and Nocardia species; P. jirovecii; cytomegalovirus; and community respiratory viruses.
Many patients with HCAP, HAP, or VAP and some with CAP are at increased risk for colonization of and infection with MDR pathogens. Risk factors for MDR pathogen infection include exposure to antimicrobial therapy 90 days before pneumonia diagnosis, current hospitalization of 5 days or more, high frequency of antibiotic resistance (in the hospital or community), all risk factors for HCAP, and immunosuppressive disease and/or its therapy. The clinical and microbiologic features of HCAP are more similar to those of HAP and VAP than to those of CAP. In an epidemiologic retrospective cohort study, Kollef et al. (2005) analyzed 4543 patients with culture-positive pneumonia who were admitted to 59 U.S. hospitals. The distribution of pathogens varied according to the 4 types of pneumonia. Nevertheless, S. aureus (including methicillin-sensitive and -resistant strains) was the dominant pathogen. The incidence rate of methicillin-resistant S. aureus (MRSA) infection was markedly higher in patients with HCAP than in those with the other 3 types of pneumonia. Also, the proportions of patients with HCAP and VAP having Pseudomonas species infections (25 % and 21 %, respectively) were higher than that of patients with CAP (17 %). However, the S. pneumoniae infection prevalence rate was higher in patients with CAP than in those with the other 3 types of pneumonia. Although most pulmonary infections in cancer patients are caused by a single pathogen, a significant proportion can have polymicrobial infections.
Initial Assessment and Management of Pneumonia in the Cancer Patient
Diagnostic Testing
A patient’s history and/or physical examination may be suggestive of pneumonia. The following initial diagnostic tests are recommended:
Chest X-ray or other diagnostic modality, such as chest computed tomography
Complete blood count with differential; basic chemical profile, including blood urea nitrogen, creatinine, electrolyte, serum transaminase, and glucose level measurement
Blood cultures in all patients with pneumonia (1 set with blood from each lumen of an existing central venous catheter [CVC] and 1 or 2 peripheral blood cultures from 2 sites if the patient does not have a CVC) prior to antibiotic administration
Sputum Gram stain and culture if the patient has a productive cough
Arterial blood gas testing is recommended for patients with oxygen saturation less than 90 % or who are unstable
If CAP is suspected, obtaining urine Legionella and pneumococcal antigens is recommended
During seasons with a high incidence of respiratory viral infections, obtain nasal washes for respiratory syncytial virus/influenza antigens and viral cultures from patients with hematologic malignancies or neutropenia
Patients with hematologic malignancies, including bone marrow transplant recipients, may undergo a serum galactomannan test (for diagnosis of invasive Aspergillus infection) and cytomegalovirus antigenemia test
Risk Assessmen t
Major decisions regarding management of CAP revolve around the initial assessment of its severity. Several pneumonia severity-risk stratification systems for CAP help clinicians predict mortality risk and site of care (home versus hospital, ward floor versus ICU). At MD Anderson, we recommend the use of the Pneumonia Severity Index for risk assessment (Aujesky and Fine 2008), as a retrospective case review demonstrated it to correlate better than the CURB-65 criteria with the severity of pneumonia in patients presenting to the EC (Gonzalez et al. 2014). Use of the Pneumonia Severity Index in immunosuppressed patients with pneumonia has yet to be validated.
Management
At our institution, we developed a comprehensive set of pneumonia algorithms and orders to assist clinicians in making important decisions regarding management steps such as selection of antibiotics and respiratory interventions, use of diagnostic testing, consultations with infectious disease and pulmonary specialists or members of a tobacco cessation program, and making recommendations for influenza and pneumococcal vaccines.
Selection of antibiotics is based on the type of pneumonia and relative risk of infection with a drug-resistant pathogen. The choice of order sets for pneumonia is based on the recommendations and guidelines for the management of CAP, HCAP, HAP, and VAP published by the American Thoracic Society and Infectious Diseases Society of America and on MD Anderson epidemiologic data (Fig. 9.2). We recommend obtaining the patient’s antibiotic history over the previous 90 days and considering an alternative agent in a different class of antibiotics. De-escalation of antibiotics and switching to oral agents should be based on microbiologic culture results and the organism’s susceptibility as well as the patients’ clinical response. In patients with HCAP having clinical responses to antibiotics, the therapy duration should be 7 days. At the MD Anderson EC, a high percentage of the patients who present with pneumonia also have signs and symptoms of sepsis. Our recommendation is to give them empiric antibiotics as soon as possible and in the first 2 h after arrival at the EC.
Fig. 9.2
Adult pneumonia order set [pages 1(a), 2(b), 3(c), and 4(d) of 10]
The antibiotic section of the MD Anderson adult pneumonia order set is divided into three options (Fig. 9.2).
Option 1: HCAP with risk factors for MDR pathogen infection or neutropenic pneumonia.
Combination therapy should be used if the patient is likely to be infected with MDR pathogens.
Patients at risk for Gram-negative bacterial infections should receive dual empiric antibiotic coverage.
Patients should receive initial empiric therapy that covers MRSA at the time of HCAP diagnosis.
The duration of antibiotic therapy for HCAP in a patient who has a clinical response should be 7 days.
Option 2: coverage for MRSA is recommended for patients with early-onset HAP or CAP but without risk factors for MDR pathogen infection.
Option 3: specific recommendations are provided for patients with MDR Pseudomonas aeruginosa , S. maltophilia, or influenza infection. We recommend prompt consultation with an infectious disease specialist for patients with fungal/mold infections.
Neutropenic Fever
Febrile neutropenia is a medical emergency. Prompt evaluation and administration of empiric broad-spectrum antibiotics is required for patients with it. Even though the use of human granulocyte colony-stimulating factors such as filgrastim and pegfilgrastim in patients at risk for granulocytopenia has increased over the past few years, fever, including neutropenic fever, is still the most common presenting symptom at the MD Anderson EC. Neutropenic fever algorithms and order sets have been developed to guide clinicians in assessing and treating febrile neutropenia.
Definitions
Fever is defined as a single oral temperature of at least 38.3 °C (101 °F) or a temperature of at least 38 °C (100.4 °F) that persists for 1 h or longer. Neutropenia is defined as an absolute neutrophil count (ANC) of less than 500 cells/mm3 or an ANC of less than 1000 cells/mm3 that is projected to decrease to less than 500 cells/mm3. Profound neutropenia is defined as an ANC of no more than 100 cells/mm3.
Microbiology
In patients with neutropenic fever, knowledge of epidemiologic shifts, local microbiology , and resistance patterns is imperative to initiate effective prophylactic, empiric, and specific treatment. Bacterial infections are most common during the early phase of neutropenic fever, and Gram-positive bacteria have predominated in most cancer centers. The most common Gram-positive bacteria are viridans streptococci and Staphylococcus, Enterococcus, Corynebacterium, and Bacillus species. The most common Gram-negative bacteria are Escherichia coli, P. aeruginosa, Klebsiella and Proteus species, and S. maltophilia. Patients with prolonged, severe neutropenia and/or those who have been exposed to multiple broad-spectrum antibiotics are susceptible to fungal infections. The most common fungal organisms in neutropenic febrile patients are Candida species, Trichosporon beigelii, and Aspergillus, Zygomycetes, and Fusarium species (Rolston 2004).
Risk Assessment
The risk of complications of infection must be assessed upon initial evaluation of a patient with fever. Decisions such as site of treatment (inpatient versus outpatient), type of antibiotics, and duration of treatment will depend on classification of a patient as being at high or low risk. In general, high-risk patients are those with anticipated prolonged (more than 7 days), profound neutropenia and/or significant medical conditions.
At the MD Anderson EC, patients with hematologic malignancies, who undergo hematopoietic stem cell transplantation, or with comorbidities such as hypotension, organ dysfunction, bleeding, and altered mental status who present with neutropenic fever are considered to be at high risk. The high-risk population must be given aggressive treatment and admitted to the hospital.
The Multinational Association of Supportive Care in Cancer developed a scoring system (Table 9.1) to identify febrile neutropenic cancer patients at low risk for a serious medical complication (e.g., hypotension; respiratory, cardiac, or renal failure; disseminated intravascular coagulopathy; severe bleeding). In a prospective observational study, De Souza et al. (2008) found that the Multinational Association of Supportive Care in Cancer risk index score has a sensitivity of 88 %, specificity of 85 %, and positive predictive value of 90.6 %. This scoring system is simple and easy to apply and may be useful in the emergency setting.
Table 9.1
The multinational association of supportive care in cancerrisk prediction model score
Characteristic | Weight (number of points)a |
|---|---|
Age <60 years | 2 |
Outpatient status | 3 |
Clinical status at presentation | |
No severe burden of febrile neutropenia | |
No or only mild symptoms | 5 |
Moderate symptoms | 3 |
No hypotension (systolic blood pressure >90 mm Hg) | 5 |
No dehydration requiring parenteral fluids | 3 |
Medical history, underlying disease, and/or comorbidity | |
No chronic pulmonary disease | 4 |
Solid tumor or hematologic malignancy without previous invasive fungal invasion | 4 |
Evaluation of the Patient with Neutropenic Fever
A very important point to emphasize is that the inflammatory response to an infectious process is significantly altered in a patient with neutropenia, and the patient may not have symptoms or signs of infection or inflammation. A thorough history and complete physical examination are important, including examination of the mucous membranes, skin, catheters, and drains for sources of infection. If the patient has perianal symptoms, the perianal region is examined visually. Digital rectal examination is contraindicated.
Work-up consists of the following:
Complete physical examination
Complete blood count with differential; ANC; platelet count; blood urea nitrogen, creatinine, electrolyte, and CO2 measurement; and liver function tests (total and direct bilirubin, hepatic transaminase enzyme, alkaline phosphatase, and lactate dehydrogenase level measurement)
Lactic acid level measurement (performed in all patients who present to the EC with fever as a screening tool to identify those who may be septic)
Urinalysis
At least 2 sets of blood cultures (1 set with blood from each lumen of an existing CVC and 1 or 2 peripheral blood cultures if no CVC is present), urine cultures, and other cultures as indicated
Chest X-ray
Consideration of the Multinational Association of Supportive Care in Cancer score
Serum galactomannan testing (for diagnosis of invasive aspergillosis) and cytomegalovirus antigenemia testing in all patients with hematologic malignancies, including bone marrow transplant recipients, admitted to the hospital; nasal washes for respiratory syncytial virus/influenza A antigen and a respiratory culture panel during seasons with a high incidence of respiratory viral infections
Outpatient Treatment of Neutropenic Fever
Low-risk patients with febrile neutropenia may be candidates for outpatient treatment. The following are the criteria for a patient to be considered for outpatient treatment at our institution:
Solid tumor
At least 15 years of age
No quinolone allergy (oral regimen)
Able to tolerate oral medications and fluids
Does not use percutaneous enteric gastrostomy feeding as the primary route for nutrition or medication
Temperature greater than or equal to 38.3 °C
ANC less than or equal to 1000/mm3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree