Introduction
The diagnosis of diabetic sensorimotor polyneuropathy (DSP) depends heavily on the demonstration of objective electrophysiological nerve abnormalities through nerve conduction studies (NCS) along with the assessment of clinical signs and symptoms . NCS are highly reproducible and the most reliable, noninvasive method for assessing DSP, especially in the subclinical stages . The American Diabetes Association (ADA) recommends screening for diabetic neuropathy in those with type 2 diabetes mellitus (DM) at diagnosis, and 5 years after diagnosis with subsequent annual evaluations in those with type 1 DM . While NCS are not recommended for routine screening for DSP, various studies have shown that as many as 30%–40% of those referred with presumptive DSP have alternate diagnoses such as lumbosacral radiculopathies, focal neuropathies, or no neuropathy at all after electrophysiological testing, indicating the potential inaccuracy of performing only clinical evaluation . NCS are more sensitive and reliable than clinical examination and accurately identify subclinical neuropathy before the onset of symptoms. NCS also provide an objective, reliable and noninvasive assessment tool and biomarker in clinical trials of DSP and also help in excluding alternate causes of neuropathy. In fact, NCS provide insight into the pathophysiological and functional properties of large nerve fibers helping demonstrate whether the pathology is axonal, demyelinating, or a combination of both. Hence electrophysiological studies should be considered as an extension of the physical examination and are valuable in the evaluation of DSP.
Pathophysiology of diabetic sensorimotor polyneuropathy
DSP is a chronic, symmetric, predominantly sensory, length-dependent, large and small fiber polyneuropathy with progressive axonal degeneration and endoneurial microangiopathy constituting the basic pathology . The increased glucose levels channel metabolism into alternate polyol and hexosamine pathways that generate increased oxidative free radicals and the formation of advanced glycosylation end (AGE) products. These, in turn, modify gene expression resulting in an inflammatory cascade . The pathological changes that ensue are observed as inflammatory mononuclear infiltrates, complement deposition, microvasculitis and necrotizing arteritis resulting in an ischemic neuropathy . Axonal degeneration and regeneration are more frequent than segmental demyelination and remyelination, and progressive axonal loss is considered to be the chief pathological hallmark in diabetic polyneuropathy . Differences in nerve pathology between type 1 and type 2 DSP have been described: in type 1 diabetes, dysfunction is initially focused at the nodes of Ranvier and milder axonal changes are observed whereas in type 2 DM, nerve fiber loss with focal and vascular pathology are more common .
Nerve conduction parameters and correlation with pathology
The various parameters assessed in NCS represent distinct nerve physiological properties. The sensory nerve action potential (SNAP) amplitude reflects the number of sensory nerve fibers while the compound muscle action potential (CMAP) amplitude is ultimately a representation of the number and size of muscle fibers in the activated motor units which in turn depends on the number of axons or neurons in the corresponding peripheral nerve. So, loss of sensory or motor nerve fibers leads to loss of corresponding amplitudes. In addition, a loss of synchronicity of firing of motor fibers due to variably reduced conduction velocities leads to temporal dispersion or conduction block and these reduce the CMAP amplitude. Loss of synchronicity in sensory nerve firing leads to reduced SNAP amplitudes. The motor and sensory nerve conduction velocities (NCV), onset latencies and F-wave latencies are determined by the fastest conducting nerve fibers. These conduction parameters depend on the degree of myelination, cross sectional nerve area and nodal and internodal integrity.
According to classical teaching, an axonal neuropathy is characterized by reduced CMAP and SNAP amplitudes with relative preservation of conduction velocities and distal latencies. In demyelinating polyneuropathies, CMAP and SNAP amplitudes are preserved and conduction velocities reduced, and distal latencies and F-wave latencies are prolonged. However, reduced amplitudes alone are not conclusive proof of axonopathy since reduced amplitudes can be observed in demyelinating pathology due to a combination of temporal dispersion and conduction block. Similarly, slowed conduction velocity or prolonged distal latency are not definitive evidence of demyelination as these findings are observed with loss of the larger and faster conducting fibers in axonopathy . A combination of parameters, including F-wave latencies, conduction block, temporal dispersion and proximal and distal segment conduction velocities and amplitudes, needs to be considered when defining the electrophysiological pathology . Reference values for NCS parameters are determined in each laboratory and cut-offs for axonal versus demyelinating changes can be variable .
Physiological changes in nerve function in diabetic sensorimotor polyneuropathy and correlation with nerve conduction studies
In DSP, the nerves undergo both functional and structural changes. From a physiological point of view, early in the disease process, there occurs a combination of microangiopathy, oxidative stress and energy failure in the neurons resulting in impaired axonal transport, dysregulated Na/K ion channels, increased Na currents and alteration of membrane excitability . The transmembrane ion channels located in the nodal and paranodal regions have a vital role in normal impulse propagation and responsiveness of nerves. The altered distribution of these ion channels and widening of the nodal gap may be responsible for the reversible nerve conduction slowing in newly diagnosed and poorly controlled diabetes, particularly type 1 . Action potential transmission occurs in a saltatory fashion from one node of Ranvier to the next, and the thickness of myelin and internodal distance determine the conduction velocity. During the process of remyelination, the number of nodes increase, internodal intervals decrease, and the myelin thickness relative to axon diameter decreases. All of these factors result in reduced conduction velocity . As the disease progresses, more apparent structural changes evolve, from myelin swelling to axonal pathology, especially at the nodes of Ranvier, and frank segmental demyelination can be observed. Eventually, there is a loss of nerve regeneration culminating in Wallerian degeneration, inexorable progressive axonal loss, and reduction in nerve fiber density. Sensory nerves are the most sensitive in DM, and the sensory NCS are the earliest to show changes with loss of SNAP amplitudes beginning distally in the lower limb. Being a length-dependent process, NCS changes would be observed first in the legs and then later in the hands . It is possible to find axonal changes in the lower limbs when demyelinating features are present in the upper limbs, but this does not imply that demyelination occurs first in DSP as upper limb nerves suffer compression frequently at carpal tunnels and cubital tunnels, and this produces demyelinating change that clouds the diagnosis of DSP . At the later stages of DSP with marked axonal loss, a marked drop in CMAP amplitudes is observed with some slowing of motor NCV. So, it is important to keep in mind that the NCS besides showing pathological changes of DSP, may also reflect other pathological processes including nerve entrapments .
Which nerves to choose and what parameters to test
When selecting the protocol for NCS in DSP, factors such as balancing sensitivity with specificity, technical ease and patient comfort, reproducibility, availability of normative data, comparison across studies, etc. have to be considered. Being a diffuse and symmetrical process, unilateral NCS are sufficient in DSP . Studies differ in the selection of nerves and the methods of nerve testing. In the largest report of more than sixty thousand patients with DSP, the most common nerve conduction abnormalities were abnormalities in sural SNAP amplitudes (62.7%) and latencies (58.3%), followed by peroneal F-wave latencies (33.6%), CMAP amplitudes (32.6%), and distal motor latencies (14%) . This clearly confirms the wisdom of choosing lower limb nerves, that is sural and peroneal nerves, for testing in diabetic neuropathy . An earlier report emphasized the need for lower limb NCS abnormalities to make a diagnosis of polyneuropathy for research purposes, and 75% of the articles that formed the basis of this report were on DSP . In the Diabetes Control and Complications Trial (DCCT), median, peroneal, and sural NCS were tested . In another report, distal tibial CMAP amplitudes correlated well with the severity of DSP . The Toronto expert panel on DSP recommended testing six nerve conduction attributes—peroneal, tibial and ulnar motor NCV, sural SNAP amplitudes, peroneal and ulnar F-wave latencies . Tibial NCS can be challenging due to technical limitations of adequate proximal stimulation at the popliteal fossa. Ulnar nerve parameters can be compromised by compression at the cubital tunnel. We recommend routine testing of upper and lower limb motor and sensory nerves in the evaluation of DSP: sural SNAPs and conduction velocities, peroneal CMAPs, conduction velocities and F-wave latencies, and median motor and sensory nerve parameters. Ulnar and tibial nerve studies can be added as deemed necessary in the electrodiagnostic evaluation although both have technical challenges compared to median and peroneal NCS. Various studies have examined the utility of medial and lateral plantar sensory nerves, dorsal sural nerve, superficial radial nerve, and sural/radial SNAP ratio . While each of these studies has potential benefits, technical difficulties, lack of ease of reproducibility, and less-than-expected sensitivity limit their clinical utility and confine them to select situations or to the research setting .
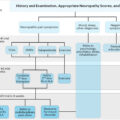
How to diagnose diabetic sensorimotor polyneuropathy with nerve conduction studies
A strict adherence to standardized technical protocols is a prerequisite for accurate measurement and interpretation of NCS results. These include appropriate skin preparation and electrode placements, ensuring supramaximal stimulation, monitoring limb temperature, accurate measurements including stimulator–electrode distances, limb positions and cursor placements on the wave forms. In the Rochester Neuropathy Study, a combination of nerve conduction abnormality in two or more nerves and quantitative autonomic examination was the most sensitive, objective, and best suited protocol for detection of subclinical neuropathy, whereas the summated CMAP amplitude of ulnar, peroneal, and tibial nerves was best for judging severity . A composite score of nerve conduction parameter deviation from normal, was specific and sensitive in the diagnosis of diabetic neuropathy . However, in the clinical and research settings, abnormal findings in one or more parameters in two or more lower limb nerves are sufficient for diagnosis .
Evolution from subclinical to clinical diabetic sensorimotor polyneuropathy
Subclinical diabetic neuropathy is defined as the absence of signs or symptoms of neuropathy in the presence of abnormal NCS or other validated objective measures of neuropathy . Asymptomatic DSP refers to those who have abnormalities on examination and abnormal objective tests, but no symptoms of DSP. NCS can reveal abnormalities well before symptomatic manifestations and the sensitivity of NCS is further increased by using composite scores of amplitude, velocity, and latency from various lower limb nerves . As DSP progresses from the asymptomatic to symptomatic stages, serial NCS changes have been noted. In the presymptomatic stage, motor nerve conduction velocity slowing and reduction in SNAP amplitudes are seen . The reduced SNAP amplitudes at this stage might be a function of demyelination resulting in temporal dispersion rather than a loss in nerve fibers although pathological studies have shown loss of fibers correlating with loss of sural SNAP amplitudes and clinical parameters indicating the primacy of axonal loss . The conduction velocity gradually diminishes at around 0.5 m/s/year . As the disease process evolves, the electrophysiological changes progress: prolongations in distal motor, F-wave and sensory latencies, slowing of sensory and motor NCV, and reduction in CMAP and SNAP amplitudes. Both conduction velocities and amplitudes are significantly lower in symptomatic patients, and these changes in NCS are associated with abnormal electromyographic signals. These findings suggest that early changes in nerve function and myelin progress to axonal pathology by the time patient starts having symptomatic polyneuropathy . A differential pattern between upper and lower limb nerve conduction with an axonal pattern of injury being more common in the legs and a “demyelinating” pattern in the arms is also noticeable although upper limb nerves are susceptible to nerve compressions that can confound the diagnosis. This difference is more apparent in younger patients . As the symptoms worsen and disease progresses, more deterioration in NCS is observed. In a 10-year study of 36 patients with type 2 DM, the prevalence of NCS abnormalities increased from 8.3% at baseline to 16.7% at 5 years and 41.9% at 10 years . The deterioration was in SNAP and motor CMAP amplitudes rather than in conduction velocities indicating predominantly axonal degeneration with time and this worsening correlated with the level of glycemic control . An overview of the evolution of pathological and electrophysiological changes is given in Table 3.1 .
| Stage | Pathophysiological changes | Clinical characteristics | Electrophysiological correlate |
|---|---|---|---|
| I | Small fiber dysfunction | Burning, lancinating pain, hyperalgesia, allodynia | Conventional NCS normal |
| II | Large fiber involvement; ion channel dysfunction at nodal and paranodal regions | Pins and needle, tingling paresthesia | Mild slowing of sensory conduction parameters; can be reversible with treatment |
| III | Beginning of structural changes, reduced myelin thickness, increased nodal number and reduced internodal interval, segmental demyelination, early axonal pathology | Paresthesias and dysesthesia progressing in a glove and stocking pattern | Slowing of nerve conduction velocities and other features of demyelination; early reduction in SNAP and CMAP amplitudes |
| IV | Wallerian degeneration, progressive axonal loss and reduction in nerve fiber density | Paresthesia could be replaced by numbness, gait, and balance issues emerge | Reduction in SNAP more than CMAP, lower limbs more than upper limbs; can have additional features of entrapment neuropathies especially in upper limbs |
Nerve conduction studies features in diabetic sensorimotor polyneuropathy: type 1 versus type 2 diabetes mellitus
Differences in the pathophysiology of type 1 and type 2 DSP have been described although extensive electrophysiological testing has not found any differences between subclinical neuropathy in type 1 and type 2 DM . More severe disease, in terms of NCS, was seen in type 2 DM in some studies, but the impact of age and other confounders make this association questionable . One notable difference in NCS between types 1 and 2 DM has been the response to treatment in the early stages of DSP. Isolated nerve conduction slowing that is prominently associated with worse glycemic control and is partially reversible with treatment can be observed in type 1 DM, but this has not been found in type 2 DM . In all other aspects, NCS parameters cannot differentiate type 1 from type 2 DSP.
Impact of treatment in nerve conduction studies
The concept that DSP is fundamentally irreversible may not be entirely accurate, particularly in the early stages. Nerve conduction slowing and predominant demyelinating features, out of proportion to axonal changes, are seen with poor glycemic control and may be reversible .
Type 1 DM patients in the DCCT who received 5 years of intensive therapy had a 64% reduced risk of DSP, and the NCV remained stable (motor) or improved (sensory and some motor) . The beneficial effect of treatment with pancreatic transplant was observed in type I DM patients who had significant improvement in motor NCV in upper and lower limbs, increased CMAP amplitudes in upper limbs and improved median sensory NCV and SNAP amplitudes as early as 1 year after surgery . Similar improvements in NCS were observed in a Japanese population of type 2 DM treated with multiple insulin injections . These patients had improved median motor and sensory NCV compared to those on conventional therapy who experienced a decline in median NCV .
A perplexing finding has been the improvement of symptoms and even NCS in placebo-treated patients in different intervention studies for DSP. While the symptomatic improvement may be explained partially by the “Hawthorne effect”—behavioral alteration due to study participation—improvements in NCS are more difficult to explain. This might be explained by short-term improvements in glycated hemoglobin and/or triglyceride levels after enrolling in a clinical trial that lead to a more sustained improvement in sensory nerve conduction parameters . Such placebo responses might be avoided by having a placebo run-in period at the start of clinical trials in DSP.
Another interesting observation is that a few studies have showed rapid control of hyperglycemia in both types of DM to favorably alter nerve conduction parameters without any significant clinical improvement . In patients who had preserved sural SNAP amplitudes at baseline, there was a significant improvement in conduction velocities, distal latencies and F-wave latencies from baseline. The improvements were less marked in patients with low baseline sural SNAP amplitudes, but remained significant in the median nerve parameters . Motor and sensory amplitudes did not change indicating that the improved parameters were due likely to improved nerve function and or ion channel function rather than nerve axon structure or number.
Although earlier studies on NCS showed more favorable changes, later studies have not confirmed these responses, and overall the effects of improved glycemic control in type 2 DSP are less robust . The magnitude of any NCS changes is small, perhaps only 1–3 m/s in nerve conduction velocity in 3-year studies . These changes in NCV reflect the improved metabolic state and ion channel activity at the nodes of Ranvier as discussed previously. Early metabolic dysfunction of myelinated fibers can be directly related to the Na + /K + -ATPase pathway, whereas the impact of impaired endoneurial blood flow is seen later and would be less reversible.
Finally, a meta-analysis examined the effects of enhanced glucose control in type 1 DM, and showed prevention of clinical neuropathy and also reduction in nerve conduction abnormalities . However, similar benefits on clinical neuropathy were not apparent in type 2 DM, although there was significant reduction in nerve conduction abnormalities . The presence of multiple additional vascular and metabolic risk factors, in addition to hypoglycemia and weight gain, might offset the benefits of tight glycemic control in type 2 DM .
Atypical features in nerve conduction studies—demyelinating features in diabetic sensorimotor polyneuropathy and when to suspect chronic inflammatory demyelinating polyradiculoneuropathy
Some clinical features raise the suspicion of an etiology alternate to diabetes as the cause of neuropathy . These include prominent asymmetry, upper limb onset or prominent upper limb symptoms, significant motor signs and symptoms, rapid progression and a positive family history . Besides these clinical factors, certain demyelinating findings on NCS suggest a nondiabetic etiology, although DSP is likely the result of a mixed axonal and demyelinating process similar to most other neuropathies. Nerve conduction slowing independent of the CMAP amplitude reduction has been described in DSP, and this is found mainly early in the course of DSP in poorly controlled type 1 patients . Demyelinating features such as conduction block and temporal dispersion are not common in DSP unless the patient has coexisting conditions such as focal entrapment neuropathies, MGUS-associated neuropathy or chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) .
CIDP has a higher prevalence in patients with diabetes with odds ranging from nine to eleven times higher compared to nondiabetics . There was no difference between type 1 and 2 DM in terms of association with CIDP. Other studies have questioned such an association between CIDP and DM, however these included only patients with “classical” CIDP based on both clinical and electrophysiological criteria and excluded patients if they satisfied only demyelinating features by NCS, limiting the sensitivity for the diagnosis of CIDP and therefore the number of patients .
Diagnosing CIDP in diabetes subjects is challenging especially since demyelinating features may be found in DSP and the preexisting diabetic neuropathy can mask the demyelinating changes in CIDP. Significant differences were noted when comparing patients with CIDP alone to those with DSP having demyelinating features (D-DSP). CIDP patients were older, had better glycemic control, a shorter duration of diabetes, and more diffuse reflex changes and nerve injuries than patients with D-DSP pointing to a different pathology of demyelination in the two conditions . On the other hand, patients with CIDP and diabetes (CIDP+DM) compared to CIDP without diabetes (CIDP-DM) had a more severe neuropathy, more proximal weakness and impairment in gait, though the treatment response was similar . A combination of clinical and electrophysiological features needs to be considered before making a diagnosis of CIDP in DM. Electrophysiologically, prominent demyelinating features with significant slowing of conduction velocities as well as conduction blocks and temporal dispersion would increase the possibility of CIDP . Proximal segment NCS would also be beneficial since the changes in DSP affect distal more than proximal segments as this is a length-dependent process, whereas in CIDP conduction velocity slowing in proximal segments can be seen. Also, compared to CIDP alone, patients with CIDP+ DM have more axonal features . Strict electrophysiological criteria for CIDP are highly specific, but may fail to identify CIDP in DM and therefore miss a treatable neuropathy in diabetes patients. For clinical practice, the evolution of new-onset progressive symmetric proximal and/or distal weakness in a patient with DSP, associated with significant demyelinating features on NCS should lead to the suspicion of possible superimposed CIDP, and a trial of immunomodulatory treatment. The presence of more prominent demyelinating features in patients with suspected CIDP and DSP makes a favorable response to treatment more likely ( Table 3.2 ).