Edematous Reactions
Jared Seth Kahn
David X. Gao
Sandhya Deverapalli
Edema occurs when there is a pathologic accumulation of fluid in either the interstitial spaces or an intracellular compartment. Various tissues can be affected including the skin; edematous reactions often present as skin colored to erythematous doughy plaques in areas of dependence.1 Subcutaneous edema is a commonly encountered problem in the oncologic patient and can have multiple etiologies including treatment-related toxicity. Both conventional chemotherapy (ie, antimetabolites, mitotic inhibitors) and targeted therapy (ie, PI3K inhibitors, PDGFR/kit inhibitors, MEK inhibitors, mammalian target of rapamycin [mTOR] inhibitors) may cause subcutaneous edema. Regardless of the potential anticancer agent culprit, a thorough medical history should be obtained and frequent causes of edema excluded, including deep vein thrombosis, heart failure, chronic venous insufficiency, kidney, liver, thyroid disease, and hereditary angioedema.
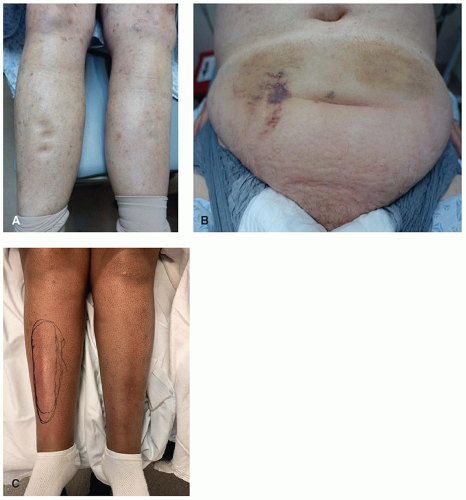
The pathophysiology of edema formation as it relates to cytotoxic chemotherapy is not well understood. The etiology is likely multifactorial with disruption to either hydrostatic or oncotic forces and with increased vascular permeability.2 Commonly affected areas include the lower extremities, periorbital region, and hands, though other sites can be affected (Figure 12.1). The two most common conventional chemotherapy agents associated with edema include gemcitabine (pyrimidine analogue, prevalence 20%) and paclitaxel (taxanes, 21%).
Docetaxel is a taxane with a lower prevalence of edema of 6.5%. Patients can present with severe, symmetric, pitting or doughy, bilateral lower extremity edema and erythema (Figure 12.2). The lower extremity edema and erythema associated with gemcitabine is often termed “pseudocellulitis”; its presence on both legs in the clinical context of cytotoxic therapy should reassure clinicians that it is not in fact the elusive “bilateral lower leg cellulitis.” With both taxanes and gemcitabine, edema may precede sclerosis that can be severe. Thus, it is important to establish the diagnosis; involvement of the arms should raise suspicion for a chemotherapy-induced etiology. It is important to distinguish these findings from other potential diagnoses such as those of infectious etiology in order to ensure correct
management of the patient. In addition to gemcitabine and taxanes, pemetrexed may cause edema that can include the upper and lower extremities (Figure 12.3) as well as periorbital regions. While a rare manifestation, the distribution can help distinguish the culprit drug in cases of combination therapy use.
Docetaxel is a taxane with a lower prevalence of edema of 6.5%. Patients can present with severe, symmetric, pitting or doughy, bilateral lower extremity edema and erythema (Figure 12.2). The lower extremity edema and erythema associated with gemcitabine is often termed “pseudocellulitis”; its presence on both legs in the clinical context of cytotoxic therapy should reassure clinicians that it is not in fact the elusive “bilateral lower leg cellulitis.” With both taxanes and gemcitabine, edema may precede sclerosis that can be severe. Thus, it is important to establish the diagnosis; involvement of the arms should raise suspicion for a chemotherapy-induced etiology. It is important to distinguish these findings from other potential diagnoses such as those of infectious etiology in order to ensure correct
management of the patient. In addition to gemcitabine and taxanes, pemetrexed may cause edema that can include the upper and lower extremities (Figure 12.3) as well as periorbital regions. While a rare manifestation, the distribution can help distinguish the culprit drug in cases of combination therapy use.
With regards to targeted therapies, edema associated with mTOR inhibitors has been well documented. The proposed pathogenesis involves interference with lymphatic endothelial expression of vascular endothelial growth factor receptor-3 leading to altered lymphatic drainage.3 Sirolimus is more frequently associated with edema than everolimus (cutaneous edema: 55% vs 10%-20%, lymphedema: 64% vs 14%)4,5,6,7 and can involve the hands and periorbital region. Case reports have also presented the finding of unilateral abdominal lymphedema in patients on everolimus.8 Imatinib, a BCR/Abl tyrosine kinase inhibitor, has also been associated with the development of cutaneous edema, most notably in the periorbital region (Figure 12.4) in addition to lower extremities. Imatinib is more commonly
associated with edema than dasatinib (cutaneous edema: 39%-75% vs 17%); periorbital edema associated with imatinib has been reported to occur in 47% to 70% of patients and other fluid-related adverse events (pleural effusion, pulmonary, pericardial, and ascites) have been reported at prevalence of 14%.9,10 Doses >400 milligrams have been shown to be associated with higher incidences of periorbital edema.11
associated with edema than dasatinib (cutaneous edema: 39%-75% vs 17%); periorbital edema associated with imatinib has been reported to occur in 47% to 70% of patients and other fluid-related adverse events (pleural effusion, pulmonary, pericardial, and ascites) have been reported at prevalence of 14%.9,10 Doses >400 milligrams have been shown to be associated with higher incidences of periorbital edema.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree