Analyte
Results
Reference range
Calcium
10.5
8.9–10.1 mg/dL
Parathyroid hormone (PTH)
68
15–65 pg/mL
Creatinine
0.8
0.6–1.1 mg/dL
25-hydroxyvitamin D
31
20–50 ng/mL
24-h urine calcium excretion
439
25–300 mg/24 h
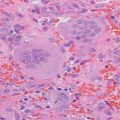
Fig. 8.1
99mTc-sestamibi (first column); iodine-123 (second column) and subtraction (third column) scintigraphy images showing a discordant focus of activity in the superior mediastinum consistent with an ectopic parathyroid adenoma. Ant anterior, RAO right anterior oblique, LAO left anterior oblique
Assessment and Diagnosis
The incidence of ectopic parathyroid glands in patients with PHPT has been reported to range from 5 % to 20 % [1–5]. Ectopic parathyroid glands can significantly impact morbidity and clinical outcomes primarily due to failure during parathyroid exploration and subsequent requirement for reoperation. It has been estimated that 24–53 % of cases of reoperation for persistent or recurrent PHPT are due to the ectopic location of the diseased gland(s) [2, 6, 7].
The clinical and biochemical features of orthotopic versus ectopic parathyroid adenomas have been evaluated in several cohorts. On average, ectopic parathyroid adenomas are both usually significantly larger and associated with higher serum calcium levels [1, 4, 8]. In one cohort, it was also noted that radiographic evidence of osteitis fibrosa cystica was more frequent in patients with ectopic parathyroid adenomas [1]. There do not appear to be other significant differences in terms of patient characteristics (age, gender) or biochemical (serum phosphorus and PTH levels), clinical (presence of nephrolithiasis, hypertension, pancreatitis, and osteoporosis), or histopathologic features (adenoma, hyperplasia, or carcinoma) in subjects with orthotopic versus ectopic parathyroid adenomas.
The parathyroid glands originate from the third and fourth pharyngeal pouches, with differentiation beginning during the fifth and sixth weeks of development. Whereas parathyroid tissue from the fourth pharyngeal pouch eventually migrates to give rise to the superior parathyroid glands, parathyroid tissue from the third pharyngeal pouch migrates caudally before arresting at the level of the thyroid to become the inferior parathyroid glands. Due to their longer migration path, the inferior parathyroid glands have a greater probability of becoming ectopic [9]. Notably, inferior glands commonly have associated thymic tissue due to the common third pharyngeal pouch embryonic origin of the thymus and inferior parathyroid glands. The most common locations for ectopic inferior parathyroid glands are intrathymic, the anterosuperior mediastinum, intrathyroidal, associated with the thyrothymic ligament, or in the submandibular area (Fig. 8.2). Less commonly, ectopic parathyroid glands derived from the inferior parathyroid can be found in the aortopulmonary window or associated with the pericardium, hypopharynx, nasopharynx, vagus nerve sheath, or posterior cervical triangle [1, 3–5, 10–12]. Superior parathyroid glands, when ectopic, are most commonly localized to the tracheoesophageal groove, retroesophageal space, posterosuperior mediastinum, intrathyroidal, carotid sheath, or paraesophageal space. One potential explanation for the ectopy of superior glands is that with disease development the parathyroid gland becomes larger and heavier, leading to vertical displacement by gravity [1, 3, 4, 10, 13].
Fig. 8.2
Anatomic localization of 104 ectopic parathyroid glands. Superior posterior mediastinum (n = 34); anterior mediastinum (n = 21); dorsum of the upper (n = 19) and lower (n = 10) poles of the thyroid; within the thymic tongue (n = 13); retroesophageal (n = 5); at the angle of the jaw (n = 1); and intrathyroidal (n = 1) (Reprinted from Wang et al. [10] with permission)
Surgical and autopsy data demonstrate that most ectopic parathyroid glands originate from inferior glands (62 % vs. 38 % from superior glands) [4]. Most are accessible via a cervical incision due to tracheoesophageal groove (28–43 %), intrathymic (24–31 %), or intrathyroidal (7–22 %) locations. The remainder are most frequently mediastinal (14–26 %) or located in the carotid sheath (7–9 %), aortopulmonary window, or submaxillary region [1, 2, 4]. In a cohort of mediastinal ectopic parathyroid glands performed at the Mayo Clinic, 45 % of patients required open thoracotomy or mediastinotomy, while 55 % of patients underwent a minimally invasive approach (such as video-assisted thoracoscopy, manubrium split, or transcervical approach) [18]. No significant difference in outcomes over a mean 3-year follow-up period was seen between subjects who underwent open versus minimally invasive surgical approaches.
Most surgeries performed for ectopic parathyroid gland resection are reoperations due to recurrent or persistent hyperparathyroidism disease after initial surgery. Reoperations typically occur in referral tertiary care centers. Due to the complexity of these operations and the potential for significant scar tissue present after initial extended parathyroid gland explorations, identifying an experienced parathyroid surgeon can be as essential as detecting the diseased parathyroid gland.
In the absence of preoperative localization, the surgeon typically carefully inspects all four orthotopic parathyroid glands in order to detect any abnormal gland. When less than four glands are found, it is recommended that the surgeon carefully inspects likely ectopic locations accessible via a cervical approach including the tracheoesophageal groove, thymus, ipsilateral thyroid, and upper cervical region [13].
Multiple imaging modalities are available for parathyroid adenoma localization and are associated with varying degrees of localization accuracy. Most reported cohorts, although limited in terms of sample sizes, suggest that patients are more likely to undergo successful surgical resection if localizing techniques are employed preoperatively [6]. Furthermore, preoperative localization for identification of ectopic glands can alter the operative approach depending on the ectopic gland location (i.e., substernal, aortopulmonary, or submandibular locations) [4, 10, 14].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree