As the technology continues to evolve, endoscopy has become not only an imaging modality but also a therapeutic instrument as one of the minimally invasive treatment options. Since late 1960s, when gastric polyps were first removed with endoscopy using an electrocautery snare, the indications have been expanded parallel with improvements in endoscopic techniques as well as the development of new endoscopic devices. In this chapter, we outline the indications for endoscopic resection of early gastric cancer, describe three major endoscopic techniques, and the outcomes of endoscopic treatment including major complications are summarized, followed by our view of the future perspective of endoscopic minimally invasive treatment.
The indications for endoscopic local resection are determined by technical and theoretical conditions. The principles of surgical treatment for cancer are to obtain a margin-free, en bloc resection in order to achieve complete resection of the primary lesion without residual disease and to fully evaluate the tumor by histopathology. The ability to achieve reliable margin-free resection is completely different depending on each resection technique. Therefore, the indication for endoscopic resection should be based on the ability of each resection technique to yield a negative margin. For example, endoscopic resection using a snare for polypectomy or endoscopic mucosal resection (EMR), to remove a small, pedunculated lesion is appropriate to obtain a clear margin as described below. However, en bloc resection for larger lesions or lesions is hardly achievable by these methods.1–4 In this situation, snare resection must be limited to lesions 2 cm or less in size and without scar formation in order to achieve complete resection.5 Endoscopic submucosal dissection (ESD), which is mainly composed of circumferential mucosal incision and subumucosal dissection, has broken new ground in achieving R0 resection of larger lesions via an endoscopic approach.6–9 There is no limitation in size or location of the tumor amenable to ESD for an experienced operator since the targeted area can be freely incised by electrosurgical knives in ESD. Furthermore, the submucosal layer beneath the lesion can be dissected under direct visualization, which enables en bloc resection even for a lesion with severe fibrosis within the submucosal layer.
Endoscopic submucosal dissection, however, is endoluminal surgery that cannot resect extraluminal lymph nodes. Therefore, the indication of ESD is theoretically limited to node-negative cancers. By investigating a large amount of surgically resected cases (more than 5000 cases), the conditions that predict node-negative early gastric cancer were elucidated as follows:10 (1) intestinal-type mucosal cancer without ulcer findings, irrespective of size; (2) intestinal-type mucosal cancer with ulcer findings, 3 cm or less in size; (3) intestinal-type cancer invading superficial submucosa up to 500 µm (SM1), 3 cm or less in size; or (4) diffuse-type mucosal cancer without scarring formation, 2 cm or less in size.11 Early gastric cancer fulfilling one of these four conditions is expected to be node-negative, which can be a good candidate for ESD.
In the so-called “pre-ESD” era, polypectomy and EMR were the two major endoscopic resection options. Polypectomy was the first technique to resect a gastric polyp by an electrocautery snare, initially performed in Japan approximately 50 years ago. Once successful resection by polypectomy was established as an appropriate resection technique, various attempts have been made to facilitate the snare technique and to expand the indication of endoscopic resection. Accordingly, EMR was then developed as a snare resection technique requiring submucosal fluid injection to achieve its intended goal.
Polypectomy is one of mucosal resection techniques that utilizes an electrocautery snare without submucosal fluid injection. This technique is quite simple; snaring, tightening, and cutting a lesion using electrocautery. Because a snare has to be put on surrounding nontumorous mucosa for complete resection, this technique is used mainly for small and pedunculated lesions. Compared to the colonic mucosa, the gastric mucosa is thick, therefore snaring a lesion is sometimes technically demanding, especially for flat lesions. Although a large snare is available, en bloc resection becomes less likely because the larger the snare is, the more technically difficult to excise the lesion completely. Polypectomy is, however, the easiest way to remove polyps endoscopically, therefore it still remains an effective technique for a particular lesions with a stalk, for example, hyperplastic polyp.12
Endoscopic mucosal resection is a mucosal resection technique using a snare after injecting fluid into the submucosal tissue below the lesion.13 After making markings around a lesion, it is elevated by fluid injection into the submucosal layer beneath the lesion and therefore is now a pseudopolyp. A snare is set around the lesion, and the pseudopolyp is gradually tightened as a snare is closed. Finally, the lesion with a part of elevated submucosal tissue is removed by electrocautery. Because the target lesion can be intentionally elevated by submucosal fluid injection, the indication for EMR can be morphologically expanded to flat or depressed lesion, although these lesions are still difficult to resect because the tissue within the snare tends to slip.
Needless to say, the size of a lesion considered resectable by EMR in an en bloc fashion is limited by technical features and the size of a snare. Furthermore, even if EMR is attempted, a lesion with associated severe fibrosis beneath the lesion is unlikely to be successfully resected in an en bloc fashion due to the inability to prevent tissue slippage when the snare is applied. Furthermore multiple additional endoscopic interventions are frequently required or even gastrectomy following unsuccessful EMR, which would be unnecessary if the lesion was completely resected during the initial intervention (EMR). Accordingly, EMR is considered appropriate only for relatively small mucosal cancers sized 2 cm or less without ulcereration.5
In gastric EMR, several variations have been reported. EMR with a ligation device (EMR-L) is a method using an O-ring, which is generally used for esophageal varices ligation.14 After submucosal injection, the lesion is suctioned into an attached hood, and an O-ring is put around the lesion to create a pseudo-stalk. This procedure facilitates subsequent snaring and can prevent slippage of the snare. In EMR using a cap-fitted endoscope (EMR-C), the lesion is suctioned into the large transparent hood attached to the tip of the endoscope, and resected by a snare set along the rim of the hood.15 In two-channel EMR method, so-called “strip biopsy technique,” an elevated lesion with saline injection is grasped by a grasping forceps passed through an already introduced snare from the other working channel beforehand and pulled into a snare to avoid slipping the snare.13 Then, the grasped lesion is captured and resected by the snare (Fig. 95-1). Endoscopic resection with local injection of hypertonic saline and epinephrine (ERHSE) may be the technique that is most equivalent to ESD among EMRs.13 Although a lateral surgical margin is theoretically expected to be tumor-free in ERHSE, this method still requires a snare that restricts the resection size. Furthermore, use of a needle knife used for circumferential mucosal incision is too dangerous for this procedure due to extremely high risk of perforation and serious bleeding. In the current clinical situation, most EMR techniques have been replaced by ESD except for EML-R, which can be still effectively applied to small protruded lesions including carcinoid tumor.
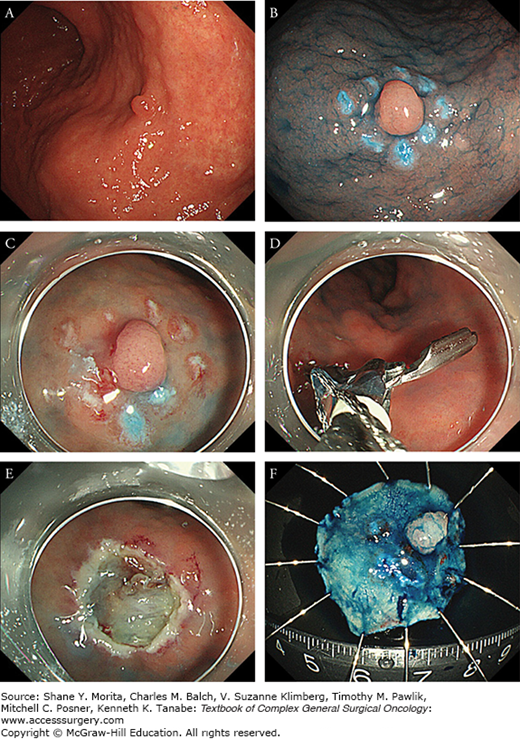
FIGURE 95-1
Procedure of endoscopic mucosal resection (two-channel method). A. A tiny protruded cancer was located on the posterior wall of upper gastric body. B. Markings were placed around the lesion after spraying indigocarmine solution. C. The lesion was well elevated by submucosal injection. D. The lesion was grasped and pulled into snare with grasping forceps. E. A mucosal defect after resection. No markings were left around the defect. F. The resected specimen. Final histological diagnosis was a 6-mm sized well-differentiated intramucosal tubular adenocarcinoma without lymph-vascular infiltration, which was considered to be curative resection.
ESD has emerged and been developed to minimize incomplete resection by EMR and avoid gastrointestinal dysfunction associated with surgery in patients with node-negative early gastric cancer. Since ESD is performed utilizing an electrosurgical knife without the use of a snare, lesions can be resected in an en bloc fashion regardless of size and location of the tumor. Furthermore, since the submucosa just below the lesion can be dissected under direct vision, reliable margin free resection is possible even for superficially invasive submucosal cancer. Although it requires highly advanced endoscopic skills, ESD has been accepted worldwide as a minimally-invasive treatment which can cure early gastric cancer when the risk of lymph node metastasis is negligible.
There are various electrocautery knives developed for ESD. Among them, Dual knife™ (Olympus Medical Systems Co., Ltd., Tokyo, Japan)8 is, in our opinion, the most useful device for ESD since it has the capacity to facilitate every step of the procedure including placing marks, mucosal incision, submucosal dissection, hemostasis, and thermal ablation of exposed blood vessels after resection. Details of the Dual knife technique are described here, as one example of the ESD procedure (Fig. 95-2).
FIGURE 95-2
Procedure of endoscopic submucosal dissection. A. A depressed cancer accompanied with ulcerative findings was located at the greater curvature of gastric antrum. B. Indigocarmine was sprayed to clarify the demarcation line. C. Mucosal markings were made around the lesion. An additional marking dot was placed at the oral side to identify a direction easily after resection. D. A half mucosal incision followed by initial submucosal dissection was made from oral side. E. Submucosal space was widely opened by transparent hood and clearly visualized. F. Circumferential incision was completed. G. Nearly the end of resection. Only a small amount of submucosa was remaining. H. Resection wound after complete resection. Prophylactic coagulation for exposed vessels was done within the resection bed. I. The resected specimen. Final histological diagnosis was a 18-mm sized well to moderately differentiated tubular adenocarcinoma slightly invading into the submucosal layer (300 μm) without lympho-vascular infiltration. Surgical margin was free from cancer and the treatment was judged to be curative.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






