II. IMMUNOPATHOLOGY OF DRUG ALLERGY
A. Drug allergic reactions have a wide diversity of immunopathology. Many drug reactions can be readily classified using the Gell and Coombs system of hypersensitivity.
1. The most common form of drug allergic reactions (maculopapular exanthems) are considered Type IV delayed-type hypersensitivity (DTH) reactions. Type IV reactions can be subdivided into four categories involving activation and recruitment of monocytes (IVa), eosinophils (IVb), CD4+ or CD8+ T cells (IVc), and neutrophils (IVd). In addition to maculopapular exanthems, Type IV drug reactions may also present with eczematous, pustular, or bullous lesions.
2. Type I immediate reactions to drugs are another common form of drug allergy and are mediated by drug-specific IgE antibodies. Clinical manifestations of type I reactions may include urticaria, angioedema, bronchospasm, and anaphylaxis.
3. Type II hypersensitivity reactions are cytotoxic reactions mediated by drug-specific IgG or IgM antibodies. Cytotoxic drug reactions most commonly affect cells of the hematopoetic system and may present as hemolytic anemia, thrombocytopenia, or granulocytopenia.
4. Type III immune complex-mediated reactions are the least common of the Gell and Coombs hypersensitivity reactions from drugs and usually present with serum sickness.
B. Several other well-characterized immunologic reactions to drugs have been described, which do not fit into the Gell and Coombs hypersensitivity paradigm.
1. Pseudoallergic reactions resemble type I hypersensitivity clinically but are not caused by IgE-mediated reactions. The pathogenesis of pseudoallergic reactions relates to IgE-independent mast cell activation. Opiates, vancomycin, and radiocontrast media (RCM) may all cause pseudoallergic reactions.
2. Drugs may also cause complement activation, release of bradykinin, or other innate immune responses.
3. Severe cutaneous adverse reactions (SCARs) have variable immunopathology and include three separate syndromes: (1) Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), (2) drug rash with eosinophilia and systemic symptoms (DRESS), and (3) acute generalized exanthematous pustulosis (AGEP).
a. SJS and TEN are now thought to represent a spectrum of a single type of reaction. The basic epidermal pathology in TEN is large-scale epidermal death, the result of apoptosis. The exact mechanism of apoptosis in TEN is unknown but may involve granzymes, granulysin, tumor necrosis factor (TNF), and Fas ligand as effectors of apoptosis.
b. The pathogenesis of
DRESS is not completely understood. Failure of drug detoxification pathways leading to an accumulation of
harmful metabolites has been hypothesized to explain DRESS from anticonvulsants. Drug-specific T cells and reactivation of human herpesvirus 6 may also be involved with the pathogenesis of DRESS.
c. AGEP is primarily thought to represent a type IVc delayed hypersensitivity response with drug-specific T cells, causing a predominantly neutrophilic dermal reaction.
4. Noncutaneous organ-specific immunologic drug reactions include immunologic hepatitis, nephropathies (interstitial nephritis, membranous glomerulonephritis), and pulmonary hypersensitivity (pneumonitis, edema, granulomatosis, and fibrosis). Drug-induced vasculitis, drug-induced granulomatous disease, and drug-induced lupus may be organ specific or have multiorgan involvement.
V. DRUG ALLERGIC SYNDROMES
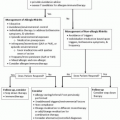
Drug allergic reactions can present with a variety of presentations, as shown in
Table 15-2. Most reactions are organ specific, but some can involve multiple organs.
A. Cutaneous reactions
1. Exanthems
The most common cutaneous manifestation of drug allergic reactions is a generalized exanthem (a.k.a. maculopapular eruption). These lesions are pruritic, often beginning as macules that can evolve into papules and eventually may coalesce into plaques. Drug-induced exanthems are pruritic and typically involve the trunk and spread outward to the limbs in a bilateral symmetric pattern. Many drug-induced exanthems are considered delayed-type hypersensitivity reactions and typically evolve after several days of being on the offending drug. With resolution of an exanthem, scaling may occur. This should be distinguished from the type of epidermal detachment seen in severe cutaneous reactions that occurs early in the reaction. Drug-induced exanthems do not evolve into anaphylactic reactions as they are not IgE-mediated reactions. Numerous drugs are capable of causing exanthems.
2. Urticaria and angioedema
Urticaria and angioedema are the most common manifestations of IgE-mediated drug allergy. It is important to recognize that non-IgE-mediated drug allergic reactions can also manifest with urticaria and angioedema. Urticaria is the most common manifestation of serum sickness; however, the presence of maculopapular lesions of the sides of the fingers and toes or a serpiginous distribution of such lesions along lateral aspects of both soles may be more specific for serum sickness. Angioedema due to ACE inhibitors is likely a bradykinin-mediated manifestation of angioedema. Complement activation may also present with urticaria and angioedema. Urticarial lesions are raised, erythematous, pruritic lesions that wax and wane and range in size from a few millimeters to several inches in diameter. Angioedema presents as
swelling of the tissues and may not be pruritic or erythematous. It has a predilection for the lips and eyelids but may occur almost anywhere.
3. Fixed drug eruptions
Fixed drug eruptions recur at the same skin or mucosal site upon reintroduction of the causative drug. Fixed drug eruptions typically develop within 1 to 2 weeks of drug exposure but may recur more rapidly with subsequent reexposure. Fixed drug eruptions are pleomorphic and may present as eczematous lesions, papules, vesicles, or urticaria. Lesions are often round or oval, sharply demarcated, red to livid, slightly elevated plaques, ranging from a few millimeters to several centimeters in diameter. They may also present with mucosal lesions that are usually bullous. Fixed drug eruptions have a predilection for the lips, hands, and genitalia (especially in men). Fixed drug eruptions can occur
with a number of medications including tetracycline, nonsteroidal anti-inflammatory drugs, and carbamazepine.
4. Eczematous reactions
Drug reactions may present as eczematous lesions. Biologics such as infliximab may cause eczematous lesions with a similar distribution as atopic dermatitis. Symmetrical drug-related intertriginous and flexural exanthema (SDRIFE) specifically refers to a symmetric drug eruption after systemic exposure with distinctive sharply demarcated erythema of the buttocks and/or V-shaped erythema of the thighs along with involvement of at least one other flexural area and the absence of systemic symptoms. SDRIFE was previously referred to as baboon syndrome. While it most commonly presents as an exanthema, SDRIFE lesions may also be papules, pustules, or vesicles.
5. Exfoliative dermatitis
Exfoliative dermatitis is characterized by widespread erythroderma and marked scaling involving >90% of the skin surface. Many more benign cutaneous eruptions can progress to exfoliative dermatitis. Several systemic manifestations can occur including hypothermia, edema, anemia, leukocytosis, and hypoalbuminemia.
6. Photodistributed drug reactions
Photoallergic reactions are DTH reactions and may present with eczematous eruptions in a photodistribution on the face, “V” area of the neck, dorsa of hands, and arms, with sparing of scalp and submental and periorbital areas. Photoallergic reactions typically develop within days of drug and ultraviolet light exposure. Phototoxic reactions typically present with erythroderma within minutes to hours of sunlight exposure but may present with vesicles with severe reactions. Drug-induced cutaneous lupus may also present with eruptions in a photodistribution, typically with erythema, or scaly, annular plaques.
7. Lichenoid eruptions
Some drug reactions may manifest as lichenoid reactions with violaceous, polygonal papules. Eruptions may resemble lichen planus. Medications associated with lichenoid eruptions include ACE-I, furosemide, gold, NSAIDs, proton pump inhibitors, and imatinib.
8. Pustular drug eruptions
Several cutaneous drug reactions may present with pustules. Acne can occur with glucocorticoids, androgens, lithium, phenytoin, and isoniazid and is quite common with the immunosuppressant sirolimus.
AGEP is a rare type of drug eruption that begins with erythema or edema in the intertriginous areas or face. Afterward, fine nonfollicular sterile pustules develop. Fever, neutrophilia, and, in one-third of cases, eosinophilia may also be present. Atypical target lesions, blisters, and oral mucosal involvement are uncommon but may be confused with SJS. Implicated drugs include antibiotics, with development of lesions within a few days. In contrast, AGEP from calcium channel blockers typically develops after a period of weeks after drug initiation. Finally,
drug-induced Sweet’s syndrome may present with fever, painful nodules, pustules, plaques, and a neutrophilic dermatosis. The onset of drug-induced Sweet’s syndrome is variable over weeks to months
after drug initiation. Granulocyte colony-stimulating factor (G-CSF), sulfonamide antibiotics, and minocycline may all cause a drug-induced Sweet’s syndrome.
9. Vesicular/bullous drug eruptions
Drug allergic reactions may also present with vesicles or bullae. Some of these reactions are relatively benign and self-limited, while others are classified as SCAR. Drug-induced pemphigus presents with flaccid blisters and is most often caused by drugs containing a thiol group (e.g., captopril, penicillamine). Drug-induced bullous pemphigoid presents with tense bullae on extremities, the trunk, and occasionally mucous membranes. ACE inhibitors, furosemide, penicillin, and sulfasalazine are some of the causative drugs implicated in drug-induced bullous pemphigoid. Linear IgA bullous disease causes a clinically similar eruption, and vancomycin is the most commonly incriminated drug. Vancomycin-induced linear IgA bullous disease is not dose dependent, and the severity does not appear to correlate with serum vancomycin levels. Erythema multiforme major (EMM) have target lesions with or without blisters. Clinically, EMM is similar to SJS, but there are important differences. The distribution of lesions is symmetric, mainly acral distribution in EMM, and mucosal involvement is less severe and extensive and involves two or more mucosal lesions less frequently then SJS. EMM occurs mainly after herpes simplex infection and less frequently is drug induced, and the prognosis is usually benign. In addition to SJS, TEN and DRESS may also present with vesicular or bullous lesions.
10. Purpuric/petechial drug reactions
The presence of purpura and petechiae are often cutaneous stigmata of vasculitis, which can be drug induced. A number of different types of drug-induced vasculitic reactions have been reported. A wide variety of drugs have been implicated, and the onset of cutaneous symptoms may occur after years of therapy with the offending drug.
11. Severe cutaneous adverse reactions
SCARs are composed of three distinct types of cutaneous reactions with systemic manifestations and include AGEP, SJS/TEN, and DRESS.
a. AGEP
Acute generalized eczematous pustulosis (AGEP) is a rare type of drug eruption that begins with erythema or edema in the intertriginous areas or face. Afterward, fine nonfollicular sterile pustules develop. Fever, neutrophilia, and, in one-third of cases, eosinophilia may also be present. Atypical target lesions, blisters, and oral mucosal involvement are uncommon but may be confused with SJS. Implicated drugs include antibiotics and calcium channel blockers. AGEP is T cell-mediated drug reaction, with drug-specific CXCL8 T cells secreting IL-8 resulting in a neutrophilic dermatitis. While classified as a SCAR, AGEP has a good prognosis with symptoms resolving within days of drug discontinuation with rare complications, more often in the elderly.
b. SJS/TEN
SJS and TEN are considered part of a single disease spectrum. A common classification separates these conditions based on the degree
of body involvement.
SJS is classified as having <10% total body surface area; between 10% and 30% body surface area is considered
overlap SJS/TEN; and involvement of >30% is classified as
TEN. The majority of SJS is drug induced, and TEN is almost always drug induced. Clinical features of SJS/TEN include a triad of mucous membrane erosions, target lesions, and epidermal necrosis with detachment. A prodromal phase of fever, cough, and malaise may precede cutaneous findings by a few weeks. Target lesions, which may evolve from three-ringed iris lesions to purpuric two-ringed lesions, often first appear on the trunk, then rapidly spread to the face, neck, and extremities, usually peaking in 4 days. Blisters of SJS/TEN are flaccid, and there may be a positive
Nikolsky’s sign (slight rubbing of skin results in epidermal detachment), especially in TEN. Mucosal lesions develop with painful lesions involving the lip, oral cavity, conjunctiva, nasal cavity, urethra, and vagina. Corneal involvement may result in ulceration, perforation, and sclerotic corneal changes. Multiorgan involvement including the gastrointestinal tract and hepatic, pulmonary, and renal involvement may also occur with SJS/TEN. Over a hundred drugs have been implicated as causes of SJS/TEN. Drugs associated with a high relative risk of developing SJS/TEN include sulfonamide antibiotics, cephalosporins, carbamazepine, phenytoin, and oxicam NSAIDs. More recent surveys have indicated that nevirapine, lamotrigine, sertraline, pantoprazole, and tramadol have also been associated with a higher risk of SJS/TEN. Prognostic factors and a TEN scoring system have been developed for TEN and include risk factors of age, malignancy, tachycardia, epidermal detachment at admission, renal function, hyperglycemia, and acidosis.
c. DRESS
The
drug rash with eosinophilia and systemic symptoms syndrome is a drug-induced, multiorgan inflammatory response that may be life threatening. The terminology describing this syndrome has varied in the literature, with various terms preferred by some authors, and includes terms such as phenytoin hypersensitivity syndrome, drug hypersensitivity syndrome, drug-induced hypersensitivity syndrome, and drug-induced delayed multiorgan hypersensitivity syndrome. Characteristic features of DRESS vary and may include various cutaneous eruptions, fever, eosinophilia (most but not all cases), hepatic dysfunction, renal dysfunction, and lymphadenopathy. Cutaneous manifestations typically include maculopapular exanthems, but vesicles, bullae, pustules, target lesions, and erythroderma may also be seen. Facial edema, which is often diffuse, occurs frequently in DRESS and can be mistaken for angioedema. Extremity and genital edema can also occur. Hypotension has been reported in up to 42% of DRESS patients. Multiorgan involvement including liver, kidney, lungs, heart, joints, and brain can often occur, and some cases of hypogammaglobulinemia have been reported in association with DRESS. Proposed inclusion criteria for DRESS include three or more of the following: hospitalization, reaction suspected to be drugrelated, acute skin rash, fever >38°C, enlarged lymph nodes in at least
two sites, involvement of at least one internal organ, and hematologic abnormalities. Medications implicated in DRESS include anticonvulsants, sulfonamides, allopurinol, minocycline, dapsone, sulfasalazine, abacavir, nevirapine, vancomycin, and NSAIDs. DRESS is atypical from other drug allergic reactions in that the reaction develops later, usually 2 to 8 weeks after therapy is started; symptoms may worsen after the drug is discontinued; and symptoms may persist for weeks or even months after the drug has been discontinued. Human herpesvirus 6 reactivation has been detected in many patients with DRESS within 2 to 3 weeks of the eruption and may be an indicator of more severe disease.
B. Drug-induced vasculitis
Vasculitis from drugs may present with cutaneous signs or have systemic involvement. Numerous drugs from a variety of therapeutic areas have been implicated in drug-induced vasculitis including propylthiouracil, hydralazine, G-CSF, cefaclor, minocycline, allopurinol, D-penicillamine, phenytoin, isotretinoin, and methotrexate. Some drugs are associated with antineutrophil cytoplasmic antibodies including propylthiouracil, hydralazine, allopurinol, minocycline, penicillamine, and phenytoin. These medications can induce severe systemic vasculitic syndromes resembling microscopic polyangiitis, Wegener’s granulomatosis, and polyarteritis nodosa. As mentioned previously, there can be a very long latency (e.g., years) prior to development of vasculits from certain drugs. Churg-Strauss syndrome has also been reported to occur in association with certain asthma medications including leukotriene modifiers, inhaled corticosteroids, and omalizumab. Several theories have been postulated including that the drug causes a steroid-sparing effect with an “unmasking” of the already present but unidentified vasculitis. To date, a cause and effect relationship for asthma medications and Churg-Strauss syndrome remains to be established.
C. Drug-induced lupus
Drug-induced lupus erythematosus (DILE) is thought to represent up to 10% of systemic lupus erythematosus cases. Similar to idiopathic lupus, DILE can have systemic forms as well as predominantly cutaneous forms.
1. Systemic DILE usually occurs after years of exposure to the offending drug and resolves within weeks to months after withdrawal of the causative agent. The most frequent signs and symptoms of systemic DILE are arthralgias, myalgias, fever, malaise, and weight loss. Procainamide and hydralazine are the most frequently implicated drugs, but causal evidence is also convincing for isoniazid, methyldopa, quinidine, minocycline, and chlorpromazine. Hypocomplementemia and antibodies to double-stranded DNA (dsDNA) are rare, while antihistone antibodies are present in >90% of patients with DILE overall but occur less frequently with minocycline, propylthiouracil, and statins. DILE related to anti-TNFa drugs demonstrates several differences from classic DILE including more frequent rash, antibodies to dsDNA (90%), hypocomplementemia, and less frequent antihistone antibodies.
2. Cutaneous DILE differs from systemic DILE in several aspects. Drugs most commonly associated with cutaneous DILE include hydrochlorothiazide, calcium channel blockers, ACE inhibitors, and systemic antifungal
agents. Anti-Ro and anti-SSA antibodies are usually present in cutaneous DILE, while antihistone antibodies are much less frequent. The onset of cutaneous DILE is much faster than systemic DILE, with disease being triggered typically in 4 to 8 weeks.
D. Serum sickness
Serum sickness is a clinical syndrome mediated by immune complex hypersensitivity. It is characterized by fever, lymphadenopathy, arthralgias, cutaneous eruptions, gastrointestinal disturbances, and may be associated with proteinuria. Symptoms typically appear 1 to 3 weeks after starting an offending drug but may occur more rapidly in previously sensitized individuals. Serum sickness was first described with heterologous antisera such as snake antivenom. Subsequently, many small-molecular-weight drugs have been found to be associated with serum sickness-like symptoms. These include penicillin, sulfonamides, thiouracils, and phenytoin. Monoclonal antibody therapies have also been associated with serum sickness-like reactions to several agents including infliximab, rituximab, omalizumab, and natalizumab. The prognosis for complete recovery is excellent; however, symptoms may last as long as several weeks. Treatment consists of systemic corticosteroids and H1 antihistamines and, in some cases, NSAIDs.
Serum sickness-like reactions have also been described with symptoms of erythema multiforme and arthralgias with or without fever, but no evidence for immune complexes, hypocomplementemia, vasculitis, or renal disease. In children, cefaclor is the most common drug associated with serum sickness-like reactions. Serum sickness-like reactions to cefaclor are thought to result from altered metabolism of the parent drug resulting in toxic reactive intermediate compounds. In vitro tests for toxic metabolites have shown a lack of cross-reactivity between cefaclor and loracarbef, but confirmation of lack of clinical cross-reactivity has not been well studied.
E. Immunologic nephropathy
The most common type of an immunologic drug-induced nephropathy is acute interstitial nephritis. Antimicrobials and NSAIDs are the most common cause, and reactions may include extrarenal manifestations such as fever, rash, arthalgias, and peripheral eosinophilia. Eosinophiluria lacks both specificity and sensitivity for a diagnosis of acute interstitial nephritis. Other types of immunologic drug-induced conditions include membranous glomerulonephritis (e.g., with gold, penicillamine, and allopurinol) or renal vasculitis.
F. Immunologic hepatitis
Many drugs have been implicated with a hypersensitivity-causing hepatitis including NSAIDs, sulfonamides, antidepressants, and halothane. Allergic hepatitis may also be seen in DRESS. Clinically, both hepatocellular injury and cholestasis can occur, and most episodes have a good prognosis with discontinuation of the drug. Resolution of the hepatitis may take 1 to 3 months upon discontinuation but, in some cases, may be associated with fulminant hepatitis, which is associated with high mortality.
G. Pulmonary drug hypersensitivity
Drug-induced pulmonary hypersensitivity can have several manifestations including interstitial lung disease (ILD), alveolar damage (e.g., edema, hemorrhage, pneumonitis), and vasculitis. Numerous drugs can cause the syndrome of pulmonary infiltrate with eosinophilia, but antibiotics and
NSAIDs are among the most common. Other classes of drugs implicated in this syndrome include anticonvulsants, antidepressants, and cardiovascular medications including ACE-I, beta blockers, and amiodarone.
Certain drug-induced pulmonary reactions are worth mentioning specifically.
1. Amiodarone has been associated with various pulmonary reactions including interstitial pneumonitis, bronchiolitis obliterans, and acute respiratory distress syndrome, with some reactions thought to be immunologic in origin.
2. Methotrexate is well known to be associated with an acute granulomatous ILD.
3. A number of chemotherapeutics have been associated with ILD that may progress to fibrosis including bleomycin, mitomycin-C, busulfan, cyclophosphamide, and nitrosourea drugs.
4. Nitrofurantoin is the most commonly reported antimicrobial causing pulmonary toxicity. The acute form of nitrofurantoin pulmonary toxicity is a hypersensitivity reaction and may develop hours to days after treatment. Symptoms may include fever, dyspnea, cough, and rash, with radiographic findings showing a diffuse reticular pattern with basilar predominance. Peripheral eosinophilia is common in acute nitrofurantoin pulmonary reactions.